MOJ
eISSN: 2374-6939


Case Report Volume 9 Issue 2
Servico de Ortopedia, Hospital De Braga, Braga, Portugal
Correspondence: Ana Costa Pinheiro, Servico de Ortopedia, Hospital De Braga, Braga, Portugal
Received: September 25, 2017 | Published: October 18, 2017
Citation: Pinheiro AC, Pereira B, Melo J, Freitas D, Silva MVD (2017) Ankle Osteochondroma: A Case Report. MOJ Orthop Rheumatol 9(2): 00350. DOI: 10.15406/mojor.2017.09.00350
The osteochondroma is a benign bone tumor surrounded by a cartilaginous capsule.1 Most osteochondroma is asymptomatic, being accidentally detected during radiographic examination.2 The osteochondroma usually reach the metaphysis of long bones and pelvis and are rarely located in the foot and ankle, except in the case of Multiple Hereditary Exostoses.3
Thus, its location on the ankle is rare, and very few cases are published in the literature. To date we have not found any ankle osteochondroma reported in Portugal. The aim of this paper is to present a case of distal tibia osteochondroma with more than 20 years of evolution, treated surgically.
The authors present the case of a female patient, 45 years old, with neoformation in the left tibia, with several years of evolution. It was a massive osteochondroma of the distal tibia involving the left tibio-peroneal syndesmosis (Figure 1) and fibula deformity. The patient observed apparent increase in size in recent years with episodes of associated pain or discomfort in this location.
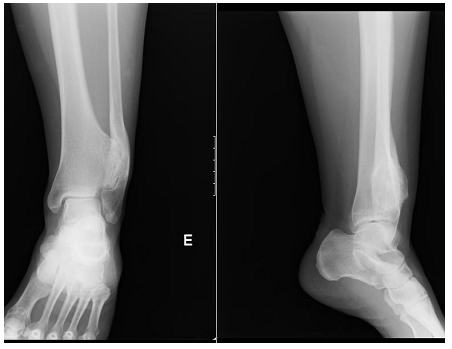
Figure 1 Left ankle X-Ray that demonstrates exostosis in the distal tibia, causing pressure and deformity in the fibula.
Physical examination revealed normal range of mobility and swelling of regular contours of the anterolateral region of the left ankle, hard, painless to palpation, without neurovascular compromise and without ankle instability. No other exostosis in the limbs was observed.
In addition to the X-ray of the left ankle, it was performed Computed tomography (CT) and preoperative Magnetic resonance imaging (MR) for a better definition of the lesion (Figures 2-3).
She was submitted to lesion excision and osteosynthesis with syndesmosis tibio-peroneal and fibula stabilization with plate and 2 trans-syndesmotic screws (Figure 4).
Histopathological examination confirmed the diagnosis of osteochondroma. At 2 months after surgery it was performed the extraction of two trans- syndesmotic screws (Figure 5), and after 18 months it was removed all material of osteosynthesis (Figure 6).
At 3 years after surgery, the patient shows a complete recovery, with full mobility and no residual pain and radiologically without evidence of recurrence (Figure 6).
The osteochondroma discovered incidentally in asymptomatic patients are treated conservatively with follow-up.4-6 The patient should be informed of the rare possibility of malignant transformation (<1%) and should be reevaluated if the injury becomes greater or more painful.7-9
Surgical resection is indicated in symptomatic patients due to irritation of the surrounding soft tissues; injury subject to minor trauma; injury with cosmetic deformity or potential damage to joints or surrounding neurovascular structures and lesions with features of malign transformation.7-10
In the literature, there are described various surgical approaches: anterior, posterior and trans-peroneal approach associated with peroneal reconstruction. The anterior approach without fibular osteotomy, as performed in this case, is associated with lower morbidity after surgery.10,11
Note: that there is little information about the clinical course of the ankle osteochondroma after its surgery, hence the need for a follow-up extended to these patients.
None.
None.

©2017 Pinheiro, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.