MOJ
eISSN: 2374-6939


Research Article Volume 8 Issue 6
Hospital Brit
Correspondence: Santiago P Vedoya, Hospital Britznico de Buenos Aires. Perdriel 74, (1280 AEB) CABA, Buenos Aires, Argentina
Received: August 04, 2017 | Published: September 12, 2017
Citation: Vedoya SP, Garabano G, Sel HJ (2017) Total Knee Arthroplasty Associate with Extra-Articular Deformity. MOJ Orthop Rheumatol 8(6): 00335. DOI: 10.15406/mojor.2017.08.00335
Introduction: Satisfactory longterm results on total knee arthroplasty (TKA) depend on restitution of the limb’s mechanical axis, correct positioning of the prosthesis, and appropriate balance of soft tissue. Patients with osteoarthritis of the knee associated with femoral or tibial extra-articular deformity require thorough preoperative planning in order to decide if the axis correction can be made through “unusual” intra-articular bone cuts or if it should be associated to an osteotomy.
Methods: 22 TKA were performed in 20 patients with osteoarthritis of the knee associated to significant extra-articular deformity of post-traumatic etiology in 8 cases and post-osteotomy in 14 (8 femoral and 6 tibial).
Results: In all cases the limb’s axis was corrected through a TKA with “unusual” intra articular bone cuts, without need of an osteotomy. The clinical and functional evaluation was made through the Knee Society scoring system. The average score for clinical evaluation was of 24.3 points preoperatively and 86 points one year after surgery. As to the functional score, it improved from 34 points preop to 85.3 points one year after surgery.
Discussion: There is not an undisputable criteria regarding the treatment of patients with symptomatic osteoarthritis of the knee associated with severe extra-articular deformity. Correction of the extra-articular deformity by intra articular “unusual” bone cuts at the time of TKA is indicated if these cuts do not affect the femoral insertions of the collateral ligaments of the knee. This method can be applied to angular deformities up to 20º in the femur and up to 30º in the tibia. Through this technique, we have achieved good results, after more than 7 year of follow up, in 20 among 22 of the operated patients.
Long-term success on total knee arthroplasty (TKA) depends mainly on restitution of the limb’s mechanical axis and appropriate balance of soft tissue, as these factors optimize the load distribution to the interfaces.1-4 Almost all patients with osteoarthritis have some degree of articular deformity, in varus or valgus, associated or not to certain ligament instability. In most cases, conventional surgical technique and equipment are used without any problem.5 achieving the correction of the axis by release and balance of soft tissues and intra-articular bone cuts in the tibia and femur.3,4,6
We consider as extra-articular the deformity located proximal to the femoral epicondyles or distal to the fibular neck. In patients with osteoarthritis of the knee, associated with extra-articular deformity, a thorough evaluation of the situation will be necessary as well as a different approach when planning a prosthetic knee replacement.2,5 The femoral and tibial extra-articular deformities can result from malunion or nonunion of previous fractures, osteotomies, metabolic bone diseases, Paget`s disease or congenital malformation. The deformity can occur in the coronal, sagital or axial planes and be even combined in different planes.2-5,7
There is a wide range of opinions regarding which is the most appropriate way to correct the axis of a limb with extra-articular deformity when performing a TKA.1,3,7-11 However, there is certain consensus in the fact that if the femoral deformity in the coronal or sagital plane is over 20° or if the tibial deformity exceeds 30°, the correction performed only by means of intra-articular “unusual” bone cuts and the consequent release of soft tissues might generate a complex instability. Therefore, the essential decision when planning a TKA will be if the correction of the limb`s axis will be obtained by means of intra-articular “unusual” bone cuts or with an osteotomy to correct the deformity.3,4,8,11-3,
This study presents the retrospective analysis of our experience in TKA in patients with knee osteoarthritis associated to extra-articular homolateral femoral or tibial significant deformity (over 10°). Its purpose is to describe the difficulties in the interpretation and planning previous to the surgery, the surgical technique, the treatment options and our results.
Between 2004 and 2014, 1116 TKA were performed in our hospital due to knee osteoarthritis, 22 of which (1.97%) where associated to a significant extra-articular deformity. In order to be included in this study, the knee must present a symptomatic gonarthrosis with TKA indication, associated to an angular deformity greater than 10° in the middle or distal third of the femur or in the middle or proximal third of the tibia.
This series includes 22 TKA (2 bilateral, non simultaneous), with 14 women and 6 men, and an age average of 67.7 years (47 to 84 years). 11 patients were operated of the right knee and 11 of the left one. The average follow up was of 7.2 years (3 to 13 years).
The causes of the deformity were: A- Post-traumatic in 8 patients (36.4 %): 3 due to malunion of femoral shaft fractures, 3 due to malunion of femoral supracondylar fractures and 2 nonunion of the proximal third of the tibia; B- Supracondylar Femoral osteotomy in 8 patients (36.4%): 7 varus (Figure 1) and 1 valgus; and C- Tibial osteotomy in 6 patients (27.2%): 3 Varus and 3 valgus osteotomies. We must point out that even if the majority of the valgus osteotomies of the proximal tibia create an extra-articular deformity, only those exceeding 10° have been included in this study.

Figure 1 A-70 year old man with valgus osteoarthritis of the right knee, a previous femoral varus osteotomy, an 11° femoral varus deformity and valgus anatomical axis of 13°. Note the limitation for using the femoral endomedular guide due to the deformity and the hardware. B- TKA with a valgus final axis of 3°. In this case we used an extra-medulary femoral guide. The femoral prosthesis stays centered in the epiphysis and appears as “not centered” with the femoral shaft.
There were 13 varus knees (average of intra-articular deformity of 9.2°) and 9 valgus knees (average of intra-articular deformity 16.6°). The extra-articular deformity was situated in the middle third of the femur in 3 patients (13.6%) (Figures 2 & 3), in the distal third of the femur in 11 (50%) (Figure 1), in the proximal third of the tibia in 6 (27.2%) and in the middle third of the tibia in 2 (9.1%). Regarding the type of deformity, all of the patients had a coronal deformity, 10 in varus (average 16.3°), 11 in valgus (average 14.4°) and 1 case with a medial displacement of the distal femoral segment of 3 cm. (Figure 3). In 6 patients, the deformity was biplanar, also with alterations in the sagital plane, 3 in flexion and 3 in extension, with an average of 19.7° and 8° respectively. No patients showed a significant rotational deformity.
The prosthesis used were 14 PFC SigmaTM (Johnson & JohnsonTM), 8 with metal trays and 6 with an All Poly trays, 3 ScorpioTM (StrykerTM) and 5 Insall Burstein (ZimmerTM). In 3 cases tibial stems were used (in the 2 patients with tibial nonunion and in 1 with a previous tibial valgus osteotomy). In 2 patients, a tibial tuberosity osteotomy was necessary to facilitate surgical access due to severe knee stiffness. The average number of previous surgeries was of 1.5 (0 to 3) and the time between the cause of the extra-articular deformity and the prosthetic replacement was 13 years in average (6 months to 44 years).
All surgeries were performed in a laminar air flow enclosure, and using hipotensive peridural anesthesia. Three doses of Cefazolin in 24 hs. (1 gr. in the anesthetic induction and afterwards 1 gr. every 8 hours) and 3 weeks of low molecular weight Heparin were administered.
Pre-OP planning and considerations about surgical technique
Surgical planning is essential in order to anticipate and avoid most of the potential difficulties and complications related to this kind of surgery. Several additional aspects must also be evaluated including age, clinical and surgical previous records of the patient, its activity level, cause and type of deformity and number of joints affected.3,6,14
The previous examination of the patient must include a thorough assessment of the limb, evaluating joint motion, stiffness and/or flexion contracture, multi-plane deformities, neuro vascular status, retained hardware and the quality of the muscles and other soft tissues. Regarding the surgical approach, in order to prevent skin and soft tissue necrosis, it is advisable to use one of the previous incisions.3,13-15,6,11,12,14 or otherwise keep a distance of at least 5 cm. between them.
It is essential to know the etiology of the deformity and its location regarding the knee in order to evaluate its real incidence in the mechanical axis of the limb.3,1,4 The nearer to the joint the deformity is, the more it will affect such articulation and the more it will condition the possibility of correcting the axis through intra-articular bone cuts.4 (Figure 4). In the radiological evaluation it is important that the weight bearing AP view includes the femoral head and the ankle in standing position (Figure 5). If this kind of studies are not available, conventional X-rays may be used, taken separately, with the same magnification in order to afterwards put together the limb as a puzzle (Figure 2). The knee must be in extension and in neutral rotation. These images will allow to evaluate the effects of the deformity in the final axis of the limb, measure the implant and calculate the necessary bone resections. It is advisable to also have a conventional AP view centered on the joint line.2,3

Figure 2 Use of conventional X-rays as a puzzle to measure the limb`s axis. A- 47 year old male showing a 2 site left femoral shaft deformity, consequence of a fracture. Valgus knee osteoarthritis, ROM 10° to 40°, femoral varus deformity of 18° and valgus anatomical axis of 23°. B- An All Poly TKA was made, obtaining a final valgus axis of 7°. In order to facilitate the access to the joint, an osteotomy of the tibial tuberosity was performed.
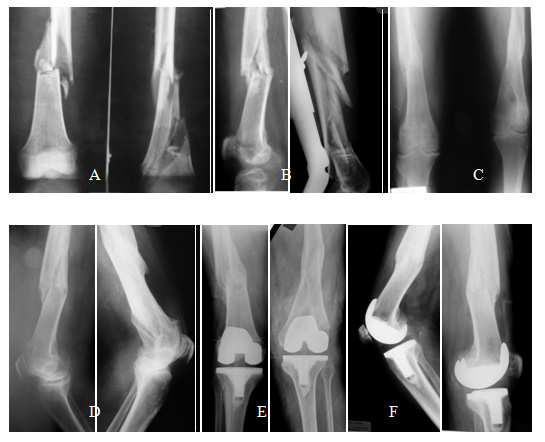
Figure 3 A and B- 79 year old man who suffered in 1974 a bilateral femoral shaft fracture that were treated non operatively. C and D- Malunion: Right femur with a medial displacement of 3 cm. of the distal bone segment and 13° of recurvatum, and left femur with a valgus deformity of 12° and 9° of recurvatum. Note the bilateral obliteration of the femoral canals precluding the use of long intramedullary guides. E and F- Bilateral non-simultaneous TKA, the left one 13 months after the right one.
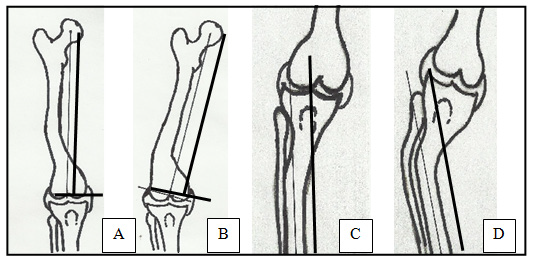
Figure 4 -For the distal femoral cut planning, a line at 90° to the mechanical axis of the femur is used: A- If the line passes below both epicondyles, the intra-articular bone cuts should be enough to correct the deformity. B- If the epicondyle ligament insertions are compromised, a correcting femoral osteotomy at the apex of the deformity may have to be performed. C-For tibial planning, the projection of the tibial segment axis distal to the deformity is used. If the axis passes inside the tibial plateaus, the correction can be made through intra-articular bone cuts without compromising the knee stability. D- If it passes outside of the tibial plateaus, a correcting osteotomy may have to be accomplished.
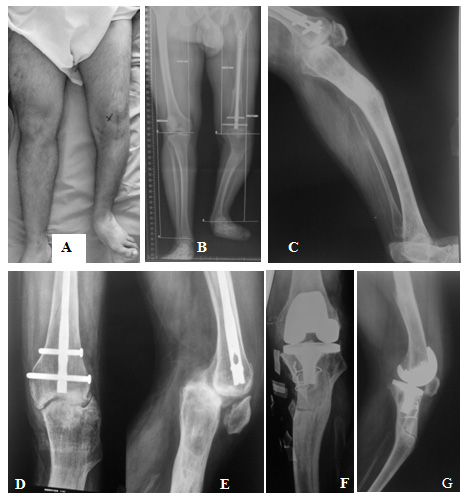
Figure 5 A, B & C- 35 year old man, with terminal fibular Hemimelia of the left lower limb, homolateral knee osteoarthritis, previous femoral nailing and a 20° varus and 28° sagital antecurvatum tibial deformity, as a sequel of a lengthening treatment. D & E- AP severe knee osteoarthritis, posterior tibial subluxation and Patella baja. F & G- AP and lateral view of the TKA. An osteotomy of the tibial tuberosity was performed.
The mechanical axis of the limb is outlined on these images (from the center of the femoral head to the center of the ankle), which should pass through the center of the knee. In patients with a varus deformity (intra or extra articular) the mechanical axis will pass medial to the center of the knee, and if the deformity is in valgus, it will pass laterally.
In order to evaluate the extra-articular deformity, the angle formed by the axis of the shaft at both sides of the deformity are measured. If the extra-articular and articular deformities have opposite axis (one in varus and the other in valgus), the resulting axis can be normal. If both deformities are in the same axis they will add up and the correction to make with the bone cuts will be greater. Rotational deformities cannot be properly evaluated with X-Rays, so a CT scan with cuts at the hip and the knee is suggested.
The distal femoral bone cut must be planned using as reference the femoral mechanical axis (cut in 90°). The correction of the extra-articular deformity can be made through intra-articular cuts of the condyles when the femoral distal cut line respects the insertions of the collateral ligaments in both epicondyles (Figure 4 A & B).2,3,4,6,8,15
We prefer the intramedullary guide if it achieves to cross over the angular deformity. If this is not possible, for example in deformities in the middle third, we recommend to use an extramedullary guide centered on the femoral head. It is important to understand that for varus femoral deformities near the joint, the entry point for the intramedullary guide can be at the articular surface of the lateral condyle and that this condyle will be the most resected. For valgus deformities, the entrance and the greatest resection will be in the medial condyle.4,6,18,20.
Is important to keep in mind that, when performing intra-articular bone cuts compensating the femoral extra-articular deformity, an asymmetrical extension box is generated, which must be compensated through a correct soft tissue release.4,6
The proximal tibial bone resection must be made at 90° to the axis of the tibial shaft distal to the deformity (Figure 4 C & D).8,2,3,15 The use of guides is ruled by the same principles as for the femur.6 A difference is that an “unusual” cut of the tibia generates an asymmetrical box in all the range of motion of the knee, which makes these deformities easier to correct through the proper soft tissue release.
Nevertheless, there is a lot of controversy about the severity of the deformity in which the correction must be performed with an extra-articular osteotomy.2-4,10,11,16 In patients with multiplanar or complex deformities, this possibility is more evident. In case of planning the extra-articular osteotomy in the same surgery than the TKA, the method used to stabilize the osteotomy must be defined. We prefer, if possible, to use femoral or tibial stems instead of plates and screws.
The Knee Society Score.7 2 was used to perform a clinical and functional evaluation before surgery and 1 year after it. The clinical average score was 24.3 points pre-operative (10 to 46), and 86 points (69 to 90) 1 year after surgery. Regarding the functional score, it passed from an average of 34 points pre-operative (12 to 53) to 85.3 points (73 to 91) one year after.
In the 2 bilateral cases, time between surgeries was 3 months in one 55 year-old patient and 13 months in a 79 year-old patient. The post-surgery average range of motion was 107º (86º to 125º) at the last control, with an average improvement of 23.3º. The average anatomical postoperative axis was 6.3º of valgus for the varus knees and 5º of valgus for the valgus knees.
There were 2 complications. A patient with femoral osteomyelitis and poor soft tissue coverage due to previous surgeries developed a deep infection. Currently, this patient has a cement spacer with antibiotics and an expansor to improve the coverage. Another patient with a 20º valgus deformity and a sequel of a distal femoral varus osteotomy developed a medial instability due to insufficiency of the medial collateral ligament, requiring revision to a constrained prosthesis 2 years after the index surgery.
When we perform a TKA we aim to restore normal anatomy by correcting the axis of the limb, to conserve as much bone as possible, to preserve the collateral ligaments and the extensor mechanism and to place the prosthesis in a correct position (if possible, a non-constrained implant).
Most of the extra-articular deformities can be corrected through intra-articular “unusual” bone resections associated to an adequate balance of soft tissues. The pre-surgical evaluation of the limb is essential to plan this unusual bone resections, as the cuts must not affect the insertion of the collateral ligaments of the knee.2,3,4,6,7,12
In patients with a varus extra-articular femoral deformity, pre-operative planning will show that a greater resection of the lateral femoral condyle will be necessary, while in a valgus deformity, there will be a greater medial condyle resection. Besides, tibial varus deformities will need a greater resection of the external tibial plateau, and those in valgus, of the internal plateau.3,4,6 These resections, which generate an asymmetrical box (of extension in femoral deformities and of all the range of motion in tibial deformities) produce a ligament disbalance which must not be underestimated. This situation, if not compensated, generates different degrees of joint instability.3-6 Therefore, without exception, the corresponding release of soft tissues in the concave side of the deformity must be performed.5
Mann.8 7 treated, through intra-articular bone cuts and soft tissue releases, 11 patients with a femoral deformity with an average varus of 14° in the coronal plane (5° to 22°) and 12° in the sagital plane (0° to 23°), achieving good results after 2 years of follow up. Wang & col.6 reported 7 patients with tibial coronal deformity of 20° average in varus (12° to 30°), treated through a large medial soft tissues release and resecting a greater quantity of the external tibial plateau. In all cases, posterior stabilized prosthesis were used.
The approach of correcting the axis through intra-articular unusual bone cuts and soft tissues release shows certain advantages, as it requires only one surgery, it allows a fast rehabilitation and avoids the possible complications of a complementary osteotomy (nonunion, infection and hardware failure) or of the ligament tightening proposed by Wolff.4 In our opinion, the ligament retightening is not a good option to achieve stability after any TKA and least of all in these difficult cases.
Some authors consider that when the deformity exceeds 10º in the tibial or femoral coronal plane, special consideration must be had due to the resulting complex instability.3,13,14,17 Even if there is no consensus, most of the publications point out that unusual bone cuts can be used in patients with femoral deformities in the coronal and/or sagital plane of up to 20º, and we agree. Regarding the tibia, deformities of up to 30º in the coronal plane can also be treated this way.7,3,6 When the deformity exceeds such limits, the bone cuts can affect the insertions of the collateral ligaments or generate an extension box too asymmetric and non compensable through soft tissue release. In these cases, an extra-articular osteotomy must be evaluated.7,10,14,17,18 and even the need of a constrained or hinged implant. It should also be remembered that, when the deformity gets closer to the knee, its impact increases due to its effect on the intra-articular bone cuts.4
If it is decided to perform the extra-articular osteotomy and the TKA in the same surgery, the osteotomy must be done in the first place, and if it is possible, using the same approach of the TKA. The osteotomy can be stabilized in different ways.5,9,10,14,19 but stems are our first choice. In these cases it is important to have modular prosthesis that allow to choose the stem that better fills the medulary canal, in order to optimize the post-surgical stability of the osteotomy.
When we perform a TKA in a patient with an extra-articular tibial deformity, the purpose of the tibial cut is to achieve the most possible parallelism between the articular lines of the knee and the tibio-talar joint. If the tibial deformity is too close to the ankle, it is advisable to correct this before the knee replacement, as if this situation is severe, it can be very badly tolerated.4 Therefore, the suggestion of Wolff to use, in patients with tibial deformity, the mechanical axis of the tibia as a reference for the cuts, is not correct, as this does not correct the obliquity between the articular lines after the TKA.4
A different issue are the patients with limited life expectancy, low functional demand, bad bone quality due to the use of steroids, rheumatoid arthritis, etc. In such cases, a better alternative could be to use a constrained implant, a hinge or even a mega prosthesis to minimize the possibility of complications associated to the osteotomy or the ligaments.20
Performing a TKA in patients with knee osteoarthritis associated to an extra-articular deformity exceeding 10º is an uncommon situation which must be thoroughly evaluated, bearing in mind that each patient has its very own characteristics and challenges, therefore needing a particular approach by the surgeon. Careful pre-surgical planning is essential to avoid the multiple possible complications (instability, nonunion, persistence of the deformity, incorrect intra-articular cuts) and thus optimizing the evolution of the prosthesis, even in the short term.
We consider two possible ways to correct the deformity of the limb. In coronal femoral deformities up to 20º and in tibial ones up to 30º, we perform intra-articular (unusual) bone cuts that should not affect the ligament insertions, associated of course to a proper soft tissue release. Otherwise, we recommend to perform an osteotomy to correct the deformity, if it is possible, in one surgical act, stabilizing it with the same stems of the prosthesis.
None.
None.

©2017 Vedoya, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.