MOJ
eISSN: 2374-6939


Case Report Volume 8 Issue 2
1Arthroscopy & Sports Surgeon, Sunshine Hospitals, India
2Department of Radiology, Sunshine Hospitals, India
Correspondence: Sarthak Patnaik, Consultant, Arthroscopy & Sports Surgeon, Sunshine Hospitals, Bhubaneswar, India
Received: February 14, 2017 | Published: May 2, 2017
Citation: Patnaik S, Mishra J (2017) Ultra Sound Guided Needling for Giant Calcific Tendinitis of the Shoulder Joint - A Peculiar Case Report. MOJ Orthop Rheumatol 8(2): 00308. DOI: 10.15406/mojor.2017.08.00308
Calcific tendinitis of the shoulder is an acute or chronic painful condition due to the presence of calcific deposits inside or around the tendons of the rotator cuff. It is caused by the deposition of calcium hydroxyapatite crystals commonly within the supraspinatus and infraspinatus tendons.1
Calcific tendinitis predominantly affects individuals aged between 40 and 60 years. Women seem to be more affected than men. Perhaps surprisingly, the incidence of this disease is not higher either in individuals who do heavy duty work involving the upper limbs, or in overhead athletes.
This cell-mediated process can be chronic in nature, but is usually self-limiting. Tendinopathy of the supraspinatus tendon usually develops in the ‘critical area’ between 1.25 and 2.5 cm proximal to the insertion site,1-3 owing to vascularisation deficits when the arm is in abduction,3-7 The rotator cuff tendons, particularly the deepest portion of the supraspinatus, undergo a transient irrigation deficiency. In 1872, Duplay8 was the first to describe calcific tendinitis of the shoulder; he defined this arthropathy as “painful periarthritis of the shoulder”. In 1934, Codman9 realized that the calcific deposits, which initially were thought to be inside the subacromial bursa, actually developed either inside or near the tendons. Bosworth10 in a large series of patients, recorded a 2.7% incidence of calcific tendinitis of the shoulder. The pathology was asymptomatic in 35% of the cases and supraspinatus tendon involvement was found in 51%.
Loew et al.11 described the most commonly affected sites, and also reported the prevalence rates of involvement of the different rotator cuff tendons (Table 1). Treatments for calcific tendinitis entail physical therapy, kinesotherapy, application of ultrasound, extracorporeal shock wave therapy, and corticosteroids injection. Platelet-rich plasma has also been used for this condition. The authors report a case of an atypical large calcification at the supraspinatous tendon treated successfully by ultrasound-guided needling and corticosteroid injection in a 50yr old woman. Calcific tendinitis is a multifocal, cell-mediated disease in which metaplastic transformation of tenocytes to chondrocytes induces subsequent calcification inside the tendon. This is followed by phagocytosis of the metaplastic areas in the tendons by multinucleated giant cells.
The etiology of calcific tendinopathy is still unknown. Rathbun & Macnab6 described ischemia of the rotator cuff tissue during calcific tendinitis. Booth & Marvel7 described degeneration of the tissue as a result of ischemic injury. Riley et al.8 described a metabolic disorder associated with ischemic injury and degeneration of rotator cuff tissue. The two most accredited etiological theories are the degenerative theory, proposed by Refior et al.9 which highlights similarities with degenerative lesions of the rotator cuff, and the multiphasic disease theory, proposed by Uhthoff & Loehr,10 which suggests that deposition of calcium in the tissues is followed by spontaneous resorption of the calcific deposit (a cell-mediated process).
|
Prevalence (%) |
|
|
Supraspinatus Tendon |
63% |
|
Supraspinatus and Subscapularis Tendons |
20% |
|
Subscapularis Tendon |
3% |
|
Infraspinatus Tendon |
7% |
|
Subacromial Bursa |
7% |
Table 1 Prevalence rates of involvement of the different rotator cuff tendons10
Other theories introduced in recent years hypothesize involvement of other factors, such as: chemical factors responsible for inducing the calcium deposition, cell proliferation, the production of anti-inflammatory agents, abnormal activity of the thyroid gland, metabolic diseases (e.g. diabetes), and genetic predisposition to the formation of calcific deposits.11 Uhthoff & Loehr10 described a three-phase process: pre-calcific, calcific (divided into three sub phases: formative, resting and resorptive), and post-calcific (Figure 1). Gosens & Hoftsee12 identified four phases (pre-calcific, formative, resorptive and recovery). Both these models identified a pre-calcific phase, characterized by a fibrocartilaginous metaplasia; a calcification phase, characterized by formation of the calcium deposit; a stable phase, with the presence of “mature” calcifications; and a resorptive phase. The latter phase, of varying duration, includes a period of spontaneous resorption during which there is both neoangiogenesis, beginning at the margin of the deposit, and infiltration of phagocytes.
A 50yr/Female with left upper limb monoplegia presented in outpatient department with complaints of pain in the right shoulder, with restricted movement of the right shoulder thereby affecting her activities of daily living, pain was sudden in onset present since last 3 months but was never shown to any physician since the intensity of pain was tolerable. On examination, the left upper limb had a power of Gr 0, Right shoulder there was wasting of the scapular and deltoid muscles. Tenderness was present on the right sterno clavicular joint, with flexion of 30 degree, abduction 20 degree and extension 10 degree. Drop arm sign positive, positive impingement sign, Test for subscapularis musculo tendinous belly press and lift off test was not possible. Blood test did reveal an uncontrolled Type II diabetes and echo showed a compromised cardiac status. Plain radiography showed a calcific deposit on the anterior and upper part of the humerus (Figure 1). Magnetic resonance imaging showed evidence of a calcific lesion in the supraspinatous tendon with evidence of partial tear of the rotator cuff (Figure 2). On the basis of these finding we made a diagnosis of calcific tendinitis of the supraspinatous tendon. The removal of the calcific tendon was challenging considering the disability of the patient, uncontrolled diabetes.
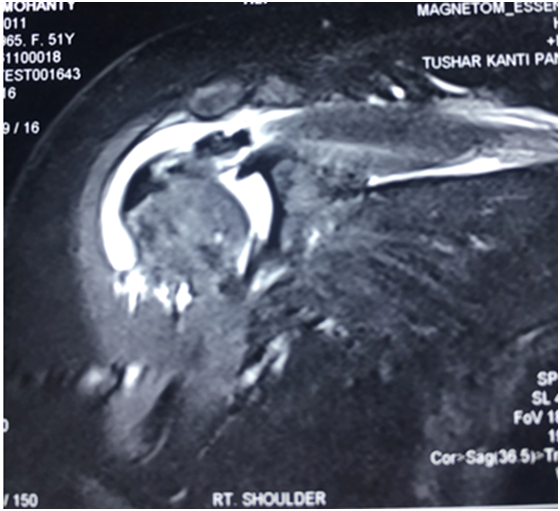
Figure 2 Magnetic resonance imaging showed evidence of a calcific lesion in the supraspinatous tendon with evidence of partial tear of the rotator cuff.
The patient was put in a semi beach chair position under local anaesthesia, General Anaesthesia was not recommended in this patient due to the poor cardiac status and also non consent by the patient. Patient also didn’t wish for local blocks as she was not comfortable with it. So it was bit challenging to do the procedure with simple local anaesthesia. With the help of radiologist under ultrasonographic guidance the calcific body was determined. It was a single 20 mm calcific body embedded in the rotator cuff sheath with no oedema in the surrounding structures. With the help of 19 and 21 gauge spinal needle the calcific body was broken into multiple fragments. The ultrasonographic guidance approach helped to reach both the ends of the calcific body with ease by keeping the needle slightly vertical and at an angle of 30 degrees to the skin (Figure 3).The procedure continued till we found the single large fragment broken down into multiple fragments under ultrasonographic guidance. After the procedure, 80 mg of Methyl Prednisolone with 5% Bupivacaine was injected at the site of lesion. Smear and culture tests were negative for possible bacterial infections of calcific material. The patient wore a sling for 1 week and mobilization was started 24 hours post procedure. Radiography performed 1 day after procedure revealed removal of large area calcifications with few calcific deposits on the humeral head, and the patient showed significant improvement with resolution of pain and improvement in the range of motion (Figure 4).

Figure 4 Postoperative radiographs (anteroposterior view) showing the subsidence of the calcific deposits.
The reason for reporting this case is patient selection, large calcific mass, technique of the procedure, avoidance of major interventional procedure.
The incidence of calcific tendinitis in asymptomatic patients is about 2.7% to 20%.12-15 35% to 45% of these patients eventually become symptomatic.12,13 The incidence of calcific tendinitis in patients with painful shoulders is about 6.8%.14 Nearly 90% of the calcifications occur in the supraspinatus and infraspinatus tendons.12,13,16,17 This ‘stress area’ is hyper vascularised, and calcium tends to deposit in 1.5 to 2 cm from the tendon insertion in the major trocar.18,19 Calcific tendinitis has a predilection for women (60 to 77%).12-14,17 The mean age at presentation is 47 (range, 31-60) years in women and 51 years in men.14,17 It rarely occurs before the age of 40 years, as calcium tends to deposit only in degenerated tendinous fibres.20-21 There was no correlation between calcific tendinitis and trauma.22 Nonetheless, others consider tenocyte necrosis is the cause of calcium deposition.23 The process of calcification is actively mediated by cells in a viable environment.23-25 Calcific tendinitis develops in 3 stages. In the precalcification stage, tenocytes become metaplastic and transform into chondrocytes, and then fibrocartilage. In the calcification stage, calcium phosphate is deposited and then resorbed, which increases regional vascularisation. In the post-calcification stage, calcium is resorbed and the area is remodeled.19,26 Based on the pathogenesis of histic hypoxia, the hypoxic state produces a lack of irrigation of the ‘critical area’ near the insertion of the supraspinatus tendon and induces calcified deposits.27,28
The main symptom of calcific tendinitis is pain, which increases in the beginning of the resorptive stage. There is no increase in vascularisation or pressure in the beginning of calcium deposition, and thus symptoms are mild. Further accumulation of calcium can lead to compression of the coracoacromial ligament. In the resorptive stage, vascularisation increases, and this increases intratendinous pressure, this exacerbates the pain.29 Symptoms usually last 2 to 3 weeks in the acute phase, 8 weeks in the subacute phase, and >3 months in the chronic phase. Calcium deposits are formed within the tendon tissue and do not affect the bone. Their extension and density are visible on radiographs.30 The type I pattern has a velvety appearance with a poorly defined periphery, and is usually seen in acute cases.17 In type II, the density is homogeneous and the limits of the lesion are better defined.17 In the chronic stages, the deposit is dense and well-defined, with a homogeneous density. In the resorptive or acute stage, the deposit is hairy, misty, and undefined, and shows irregular density. Ultrasound is also useful for visualising calcific tendinitis, and has a diagnostic performance of 90%.31
We have presented an unusual case of calcific tendonitis occurring at the supraspinatous insertions in which ultrasound guided needling was performed and no surgical detachment and subsequent reattachment were performed. When the calcifications are diffusely scattered over a wide area, the less invasive ultrasound guided needling procedure may offer a treatment option for rotator cuff tendonitis.
Consent was taken from the patient to publish about her ailments.
None.
None.

©2017 Patnaik, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.