MOJ
eISSN: 2374-6939


Research Article Volume 8 Issue 1
1Physical medicine and rehabilitation, (Chief Therapist & Clinical Supervisor), Spinal Correction Center of Quebec, Canada
2Doctor in chiropractic, Spinal Correction Center of Quebec, Canada
Correspondence: Noureddine Soual, Chief Therapist & Clinical Supervisor, Spinal Correction Center of Quebec, Boulevard de la chaudiere, no 125. Quebec, G1X 4M8, Canada, Tel 1 418-446-8646
Received: March 24, 2017 | Published: April 20, 2017
Citation: Soual N (2017) Non Surgical Disc Decompression & Clinical Efficacy. MOJ Orthop Rheumatol 8(1): 00299. DOI: 10.15406/mojor.2017.08.00299
Low back pain and neck pain are a public health problem in developed countries. Studies assessing the prevalence of this condition in the general population have led to different results. 85% of North American adults suffer from low back and neck pain at some point in their lives and more than 26 million Americans aged 20 to 64 have had frequent experience of back pain.
Excessive loads on the spine by changes in our lifestyle and long periods of sitting while driving or working in the office is a cause of premature degeneration of the intervertebral discs, and of repeated injuries to the annulus.
Low back pain is particularly widespread. It is the second most common reason to consult in medicine, the fifth most common cause of admission to hospitals, and the third most common cause for surgery.
Given the enormous cost, over 50 billion dollars is involved in this epidemic, in the United States alone. (Especially low back pain), the medical consensus based on evidence, recommended a new emerging model of care, described in this study.1
According to Scott Boden, MD, director of the Emory Orthopedic and Spinal Center in Atlanta "A disease like lower back pain can cause a lot of variability in how health professionals" approach it.
The standard medical approach to back pain currently is prescribing analgesic, anti-inflammatory drugs, muscle relaxant and sometimes morphine derivatives. This is often not very effective. "Medical care for low back pain in the 20th century was catastrophic. Most approach did not solved the daily symptoms of lower back pain and may even have reinforced and exacerbated the problem," Gordon Waddell, MD, orthopedic surgeon and researcher of the spine.1
Back surgery is a risky solution, expensive and of restricted indication. Non-surgical treatment is the preferred method for practitioners and patients. The traditional method of lumbar traction can actually reduce the bulging disc and relieve symptoms by reducing intradiscal pressure. However, the effects of the treatment vary widely because of different devices or equipment used.2
Researchers around the world have studied and explored the therapeutic mechanism of spinal traction and updated processing devices.
The purpose of this study is to explore the effect of the non-surgical Spine-Med Decompression system on cases of low back pain and neck pain and to determine the effectiveness of such approach.

This study is a pilot project in Quebec City, Canada. It is a retrospective cohort of a patient group with a single practice, this group is treated for back and / or neck pain. The patients received non-surgical spinal decompression treatment protocol 3 times per week for 4-8 weeks.
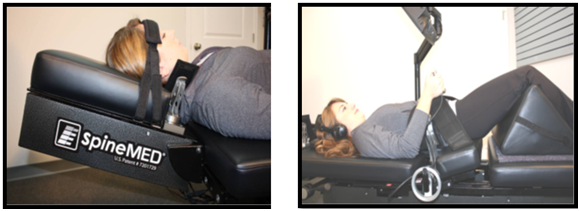
All treatments were undertaken using the decompression table Spine MED® (Universal Pain Technology) It is a patented design which represents the latest evolution of the non-surgical disc decompression technology.
The Spine MED® table uses a computerized system permitting targeted computer a sized pulling of the intervertebral discs; it is a proprietary design to provide an intermittent distraction for either of the lumbar or cervical spine.
All data were manually extracted from patient medical records (paper or computerized) and data reporting forms. Data were entered into a Microsoft database and analyzed using statistical software - JMP from SAS Institute.
Descriptive statistics were used to communicate clinical and other similar data. Patients undergo 2-3 clinical revaluation at different levels, namely (joint assessment, neuromuscular and functional assessment) performed by the Chiropractor and Chief Therapist. Each examination is preceded by a surface EMG of the spine. (The adaptations of the neuromuscular system and the electrical activity of the para-vertebral muscles can be verified).
Disc decompression protocol consists of a series of two phases on the disc per cycle; a maximum tension phase which last 60 sec., called high power, followed by a phase of releasing tension which last 30 sec., called low power. The treatment period last approximately 30 minutes. The tension in the high power phase is calculated in pounds (lb), which represents a quarter of the patient's weight minus 10 lbs. The low power phase is 1/2 of the maximum tension during high power.
This SpineMed table is able to make adjustments every 20 milliseconds. This capability to adjust almost instantly the right tensions is an essential difference that distinguishes this SpineMed decompression devices from other conventional traction systems. Pain was assessed using the visual analogue scale (VAS) from 0 to10, 10 being the most painful.
From January 1st, 2014 to December 31st, 2014, we used the Spine-Med decompression table, a new patented device developed by the American Institute of Health and approved by Health Canada, to treat and monitor 121 patients with low back pain or neck pain. We observe the level of satisfaction in the short to medium term after completing the recommended decompression treatment.
Most patients who received lumbar decompression (90%) had a hernia or a degenerative disc disease at L4-L5 and / or L5-S1 (Figure 1).
On the other hand the majority of patients who received cervical decompression (80%) had a hernia or degenerative disc at C5-C6-C7 and D1 (Figure 2)
36% of patients had the confirmation of a herniated disc by MRI / CT scan, while 29% had confirmation of degenerative disc disease (detected by standard X-ray) (Figure 3).
Disc degeneration is the most common lesion (44.62%). Facet arthrosis and spinal osteophytes are also seen quite often (11,57 %) (Figure 4).
There is a very significant improvement in lowering pain with a VAS from 7 on day 1 to 3 on day 20 on average (statistically significant p <0.0001) (Figure 2 &Table 1).
A very significant improvement in the level of patient satisfaction after the decompression protocol (Table 2).
|
lumbar disc injury |
Nber et % |
cervical disc injury |
Nber et % |
|
L4-L5 et L5-S1 |
37 (34.9%) |
C5-C6 |
2 (10%) |
|
L5-S1 |
50 (47.1%) |
C5-C6-C7-D1 |
14 (70%) |
|
L4-L5 |
8 (7.5%) |
C4-C5 et C5-C6 |
3 (15%) |
|
L3-L4 et L4-L5 |
9 (8.5%) |
Other |
1 (5%) |
|
L2-L3 et L3-L4 |
2 (2%) |
||
|
Lumbar |
106 |
Cervical |
20 |
Table 1 Statistical data on treaties levels:
N-B: There are 5 patients who have received, in the same period, a lumbar and a cervical decompression.
The effectiveness is not age related. Patients older than 57 years (median) have a decrease in pain from 6.9 to 3.2 (p ˂ 0.0001) and patients younger than 57 years have a decrease in pain from 6.8 to 3.0 (p ˂ 0.0001) (Figure 6).
|
Satisfied (81%) |
Not satisfied (19%) |
||
|
Very satisfied |
satisfied |
Moderately Satisfied |
Not satisfied |
|
46% |
35% |
15% |
4% |
Table 2Statistical data on the degree of satisfaction.
There is also a similar effectiveness in decreasing pain between women (3.2 vs 7.3, p ˂ 0.0001) and men (3.0 vs 6.6, p ˂ 0.0001) (Figure 7).
No difference was found on the effectiveness of treatments based on the chronicity of the lesions (Figure 8).
Pain present more than 2 years (71.9%): 3.3 vs 7.0; p ˂ 0.0001. Pain present less than 2 years (28.1%): 2.6 vs 6.7; p ˂ 0.0001.
Whether the onset of injury was sudden or progressive (accident or chronic), has no influence on the results of the decompression: 40% of patients have had a sudden onset (accident, sprain), while 60% of patient consulted following a gradual onset of symptoms. Both type of onset did not influence the degree of patien tsatisfaction.
So the improvement of pain on a visual analog scale was not based on the difference between patients depending on the circumstances it occurred, with a (p˂0.0001) (Figure 9).
A very significant improvement in the physical condition of the patients was noted in the last re-evaluation examination performed at the end of the decompression protocol (Table 3). NB: The improvement is based on the clinical condition (Lasegue, distance finger-floor muscle testing, deep tendon reflex sensitivity ... etc.), on endurance, fluidity, and the activities of daily living.
A good clinical improvement is justified by the reduced medication intake: 70% of patients under care had reduced significantly or stopped entirely their medication intake (Table 4).
|
Satisfied (81%) |
Not Satisfied (19%) |
||
|
Very satisfied |
satisfied |
Moderately satisfied |
Not satisfied |
|
46% |
35% |
15% |
4% |
Table 3 Statistical data on the clinical improvement.
Whatever the type of spinal injuries, the satisfaction rate with spinal decompression was over 80% on average (Table 5).
|
Medication after Decompression |
||||||
|
Medication Before |
0 |
1 |
2 |
3 |
||
|
0 |
20.66% (25) |
0 |
0 |
0 |
20.66% (25) |
|
|
1 |
23.14%(28) |
4.96%(6) |
0 |
0 |
28.10% (34) |
|
|
2 |
11.57%(14) |
26.45%(32) |
2.48%(3) |
0 |
40.5% (49) |
|
|
3 |
4.96%(6) |
0.83%(1) |
2.48%(3) |
2.48%(3) |
10.74% (13) |
|
|
60.33% (73) |
32.23% (39) |
4.96% (6) |
2.48%(3) |
100%121 |
||
Table 4 Statistical data on drug intake before and after decompression treatments:
0: No medication.
1: Analgesics as necessary.
2: Analgesic NSAID + analgesic.
3: Derivatives morphine + NSAID + analgesic.
The clinical improvement of patients on all levels, articular, neuromuscular and functional level, was not influenced by the type of associated injury. 74% of all patients had satisfactory clinical improvement in degenerative disc disease cases and 85.71% of patients with facet arthrosis had satisfactory clinical improvement (Table 6).
|
Not satisfied |
Moderately Satisfied |
Satisfied |
Very Satisfied |
Total |
|
|
No associated lesion |
2.56%(1) |
15.38%(6) |
30.76%(12) |
51.28%(20) |
100%(39) |
|
Degenerative disc disease (discarthrosis) |
5.55%(3) |
14.81%(8) |
33.33%(18) |
46.29%(25) |
100%(54) |
|
Facet arthrosis |
7.14%(1) |
7.14%(1) |
28.57%(4) |
57.14%(8) |
100%(14) |
|
Other injury (osteophytes) |
0 |
21.42%(3) |
57.14%(8) |
21.42%(3) |
100%(14) |
Table 5 Spinal lesion and associated clinical satisfaction.
|
Not Satisfactory |
Moderately Satisfied |
Satisfactory |
Very Satisfactory |
Total |
|
|
No associated lesion |
0 |
23.07%(9) |
33.33%(13) |
43.58%(17) |
100%(39) |
|
Degenerative disc disease (discarthrose) |
3.70%(2) |
22.22%(12) |
40.74%(22) |
33.33%(18) |
100%(54) |
|
facet arthrosis |
7.14%(1) |
7.14%(1) |
35.71%(5) |
50%(7) |
100%(14) |
|
Other injury (osteophytes) |
0 |
28.57%(4) |
57.14%(8) |
14.28%(2) |
100%(14) |
Table 6 Type of spinal lesion and associated clinical improvement.
NB: In order to correlate the degree of patient satisfaction and clinical improvement observed during the various evaluation tests.
According to the statistical method of Pearson, r = 0.8469027 (There is 85% of the correlation between what the patient reports as improvement and the physical examination results).
During this cohort study, we extracted data from 121 patients with low back pain and / or neck pain. An average reduction in pain from 7 to 3 on a scale from 1 to 10 was detected following non-surgical disc decompression treatment. These results are consistent with previous studies.2-4 We are fully aware that the measurement of pain is subjective and is based primarily on the patient's perception. (Farrar et al, reported that an average intensity reduction of pain in at least 2 points represents a clinically significant change).5 Following our study. The average pain reduction was 4 points.
However, we have systematically studied the influence of the starting mode of the lesions of the spine on the therapeutic efficiency. It was revealed that whatever the mode of onset of the injury, either early, progressive or sudden, the pain on the visual analog scale went down from 7 to 3. The age of the lesion does not constitute an aggravating factor, and the level of pain went down 3.8 and 4.1 on the pain scale for both, recent lesions and older injuries.
When analyzing the influence of age and sex on the efficiency of non-surgical disc decompression, no correlation was found between age or sex and treatment success. Even the hypothesis that a population of younger patients may react differently to the treatment of non-surgical decompression as they normally have less disc degeneration, is false because according to our results, the efficiency is similar to older patients.
Pain decreased from 6.9 to 3.2 for patients older than 57, and 6.8 to 3 for those patients younger than 57 years old. ˂0.0001 p (Figure 2).
The fact that disc degeneration is the most common lesion, with 45 %, did not influence significantly the clinical improvement of patients. A large proportion of our patients (70%) with low back pain or neck pain were under a wide range of analgesics, (analgesics, NSAIDs, muscle relaxants and morphine derivatives). The significant reduction in drug consumption observed after the non-surgical disc decompression protocol (Suppressive effect), is the proof of the clinical efficiency of such approach.
In the end, the limitation of our study is the lack of a control group (placebo), due to the possibility of a spontaneous evolution.6-8 However, the objective of our study is to demonstrate the clinical efficiency of non-surgical disc decompression which we did.
Obviously we observed a significant improvement in over 80% of our patients. This demonstrate improvement in the ability to conduct activities of daily living; significantly improving pain scores and a significant decrease in disability status and increase in functional status of patients. We have shown through this retrospective study, the clinical efficiency of non-surgical disc decompression. This study need to be followed by a randomized double blind clinical trial, and make the long-term monitoring of the clinical status of patients.
The paradox of low back pain and acute neck pain has received considerable attention lately for good reasons.3 Different approaches and treatments abound among practitioners of different skill. Because of the huge costs involved in this epidemic, the consensus of medicine based on evidence, recommended a new emerging model of care which is non-surgical disc decompression.1 A health problem like back pain can have a lot of variability in how it is approach by health professionals, according to Scott Boden (MD, director of the Emory Orthopedic and Spinal Center in Atlanta).9 "Many, if not most, primary care providers have little training on how to manage locomotor disorders ». The practitioner should open their mind to more than medical processes.
Indeed, low back pain, neck pain and lumbosciatica become a problem because the standard medical approach such as pain removal with: NSAIDs, pain relief, muscle relaxant, steroid injections, MRI explorations. TDM and disc surgery, was shown to be costly, risky and often ineffective according to Gordon Waddell MD, orthopedic surgeon and researcher of the spine "medical care has certainly not solved the daily symptoms of pain in the lower back and even perhaps reinforced and exacerbate the problem".1
Disc decompression is an effective and safe uncomplicated technique and is also non-invasive; it should be the first choice for the care of damaged discs as indicated. Overall, the study presented favorable results and reflects what practitioners and SpineMED® patients testify daily. The success rate of the disc decompression in this study, and the others that proceeded is especially notable compared to the risk factors involving surgical treatment in similar conditions (Street et al., 2012). The American Journal of Pain Management reported "good to excellent relief" in 86% of patients with a herniated disc, back pain and sciatica symptoms. Good to excellent result was also obtained in 75% of people with facet syndrome after a series of 20 disc decompression treatment.10 According to Dr. Deyo chiropractic was a popular solution: "Chiropractic is the most common choice, and there is mounting evidence that spinal manipulation can indeed be a cure for the effective short-term pain for patients with back problems the past".11
None.
None.

©2017 Soual, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.