MOJ
eISSN: 2374-6939


Case Report Volume 7 Issue 6
Department of Surgery, Agha Khan University, Pakistan
Correspondence: Muhammad Ali, Department of Surgery, Agha Khan University, Block-I, House no -4 shahruknealam colony Multan, Karachi, Pakistan, Tel 923000000000
Received: November 21, 2016 | Published: April 13, 2017
Citation: Ali M (2017) Osteopoikilosis: an Incidental Finding in a Patient with Olecranon Fracture. MOJ Orthop Rheumatol 7(6): 00294. DOI: 10.15406/mojor.2017.07.00294
Osteopoikilosis (OPK) or osteopathia condensans disseminate or spotted bones is a benign osteosclerotic dysplasia of unknown origin. It is an inherited autosomal disorder. It is usually detected as a coincidental finding at radiographic examination. Both sexes are equally affected. The condition is usually asymptomatic. The most common localization of these lesions is in the phalanges of the hand, carpal bones, metacarpals, metatarsals, foot phalanges, pelvis, femur, and humerus. They are occasionally associated with cutaneous lesions as well as other osteosclerotic skeletal disorders. We report a case who presented to us in emergency with fracture of olecranon. On reviewing radiographs, in addition to olecranon fracture; diffusely distributed round sclerotic foci were also seen. These findings were strongly suggestive of osteopoikilosis.
Keywords: Osteopoikilosis, Sclerosing bone dysplasia, Olecranon fracture
Osteopoikilosis (osteopathia condensans disseminate, spotted bone; OPK) is a rare bone dysplasia. The skeletal changes of osteopoikilosis were first described by Stieda in 1905 followed by Albers-Schoenberg (1915). It has an autosomal dominant inheritance, and can be observed equally in both sexes and in all age groups. It is an uncommon disorder with an estimated incidence of 1/50,000.1 The etiology and pathogenesis remain unclear. It is usually asymptomatic and is a coincidental finding at radiographic examination. However, mild joint pain and swelling may be seen in 15-20% of cases. The most common localization of these lesions is in the phalanges of the hand, carpal bones, metacarpals, metatarsals, foot phalanges, pelvis, femur and humerus. There is no involvement of the clavicles, ribs or skull, typical of osteopoikilosis. In the affected bone these lesion are seen in the epiphysis and metaphysic. These multiple, sclerotic, roundish lesions vary in size from a few millimeters to several centimeters. They are scattered within the cancellous bone and concentrated near the joint surface.2 In 25% of the cases osteopoikilosis is associated with skin manifestations (dermatofibrosis lenticularis disseminata, keloid formation, plantar and palmar keratomas), rheumatic and skeletal disorders (arthritis,exostoses, osteitis condensans ilii, melorheostosis, spinal stenosis, chondrosarcoma, osteosarcoma), organ anomalies (aorta coarctation, double ureter, growth abnormalities, hare lip, dental abnormalities), and endocrine dysfunction (diabetes mellitus).3 Histologically, osteopoikilosis is defined as focal condensations of compact lamellar bone within the spongiosa and is related to other osteosclerotic disorders like osteopathia striata, fibrous dysplasia and melorheostosis. This disorder may resemble osteoblastic metastasis, mastocytosis and tuberous sclerosis.4
A 33 years old man was presented to us in the emergency room with the history of road traffic accident. He slept from motor bicycle and sustained injury in his right elbow. He has no associated other injury. After usual pain management, we offered radiograph of injured elbow.
On reviewing his radiographs, in addition to olecranon fracture; diffusely distributed round sclerotic foci were also seen (Figure 1). Patient was asymptomatic before RTA. He was initially managed with back splint. In order to confirm the diagnosis, additional radiographs were performed that included, shoulder (Figure 2) and pelvis (Figure 3). These entire radiographs revealed diffusely distributed round sclerotic foci. Bone scintigraphy for whole body with Tc-99 m was normal. In order to exclude any other pathology laboratory work up was also done that included complete blood count, sedimentation, C-reactive protein, rheumatoid factor, thyroid, renal, liver function tests, calcium, phosphor, alkaline phosphatase, parathyroid hormone, urinalysis that were all normal. Bence Jones protein and tumor markers were negative. In order to confrm the autosomal dominant inheritance of these lesions, the medical histories of the closest family members were taken and radiographs of the wrist were also done .We found no signs of similar lesions. We thus concluded it was a sporadic case. Finally the diagnosis of osteopoikilosis was made. Lastly the fracture was fixed with tension band wiring (Figure 4).
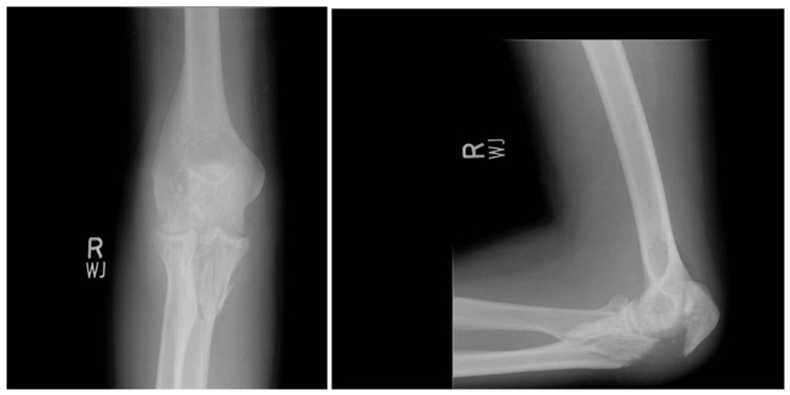
Figure 1 Radiograph of elbow showing fracture of olecranon and associated small, roundish, sclerotic lesions.
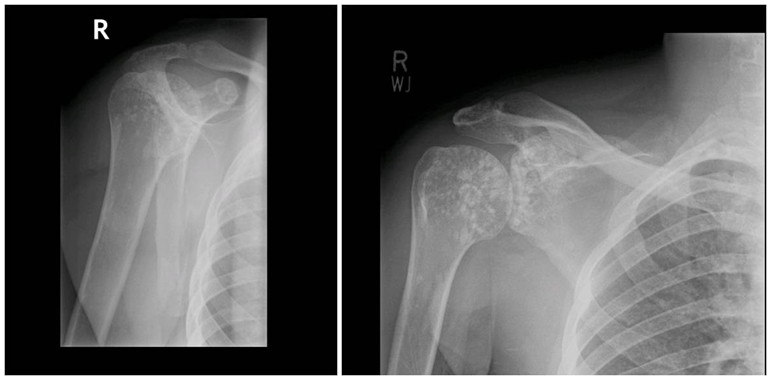
Figure 2 Radiograph of the shoulder showing multiple ovoid radiodense sclerotic foci of the proximal humerus and scapula adjacent to the glenohumeral joint.
Osteopoikilosis osteopathia condensans disseminata, is an osteosclerotic dysplasia with an unclear etiology and pathogenesis which takes place during childhood and persists for life. The patteren of inheritance is autosomal dominant, although sporadic cases do exist, as in our case (since no family member had the disease).1-3 The diagnosis is usually made incidentally after radiographric review is done for another reasons as in our case for elbow injury, assessing numerous small, well-defined, homogeneous, circular-to-ovoid foci of increased radio density clustered in periarticular osseus regions. Sites of predilection include phalanges (100%), carpal bones (97.4%), metacarpals (92.5%), and foot phalanges (87.2%), metatarsals (84.4%), tarsal bones (84.6%), pelvis (74.4%), femur (74.4%), radius (66.7%), ulna (66.7%), sacrum (58.9%), humerus (28.2%), tibia (20.5%), and fibula (2.8%).5 The ribs, skull and vertebrae are typically spared as in our case. Typically patients are asymptomatic as is the case of our patient but 15-20% may have slight articular pain and joint effusion The number of sclerotic lesions in a single bone range from 1 to 1,000 and they can both increase and decrease in number, size and radiodensity or even disappear eventually. Histologically, osteopoikilosis is defined as focal condensations of compact lamellar bone within the spongiosa.6
|
Isolation method |
Number of isolated |
||
|
Site 1 |
Site 2 |
Total |
|
|
Rotting – Vortexed |
148 |
123 |
271 |
|
Rotting- Directly Plated |
123 |
88 |
211 |
|
Fresh – Vortexed |
82 |
131 |
213 |
|
Fresh - Directly Plated |
50 |
104 |
154 |
|
Total |
403 |
446 |
849 |
Table 1 Organisms isolated from different study sites against different isolation methods
|
Genus |
Number of isolates |
Number of organisms positive for various activities |
||||
|
Ulvan Lyase |
Carbohydrate Sulfatase |
Exocellulase |
Endocellulase |
β- glucosidase |
||
|
Vibrio |
83 |
49 |
24 |
6 |
0 |
52 |
|
Halomonas |
20 |
19 |
0 |
0 |
0 |
1 |
|
Cobetia |
9 |
9 |
0 |
0 |
0 |
0 |
|
Psychromonas |
1 |
1 |
0 |
0 |
0 |
0 |
|
Pseudoalteromonas |
14 |
10 |
0 |
0 |
5 |
1 |
|
Zymobacter |
1 |
1 |
0 |
0 |
0 |
0 |
|
Moritella |
1 |
1 |
0 |
0 |
0 |
0 |
|
Photobacterium |
1 |
1 |
0 |
0 |
0 |
0 |
|
Winogradskyella |
1 |
1 |
0 |
0 |
0 |
0 |
|
Aliivibrio |
1 |
1 |
0 |
0 |
0 |
0 |
|
Unidentified |
103 |
73 |
3 |
10 |
55 |
14 |
|
Total |
235 |
166 |
27 |
16 |
60 |
68 |
Table 2 Number of organisms identified from each genus and the activities they possess
The major differential diagnostic considerations in cases of widespread focal round or oval radiodense lesions are osteopikilosis, osteoblastic metastases, mastocytosis, tuberous sclerosis and synovial chondromatosis. The symmetric distribution, the predisposition for epiphyseal and metaphyseal involvement, and the uniform size of the lesion are features that suggest osteopoikilosis7. A bone scan is essential in distinguishing osteopoikilosis from primary bone tumors or osteoblastic bone metastases. Scan is usually normal in patients with osteopoikilosis, but may show slightly increased tracer uptake8. Bone scan for whole body with Tc-99 m was normal in our patient. Several other rheumatologic diseases can coexist with OPK, such as rheumatoid arthritis, lupus erythematosus, reactive arthritis, ankylosing spondylitis and familial mediterranean fever,3,4,6 but these were absent in our patient. Various developmental abnormalities have been reported to be associated with osteopoikilosis, including: coarctation of the aorta, double ureter, pubertas praecox, urogenital defects, growth abnormalities, peptic ulcer, diabetes mellitus at the endodermal strata level, arthritis, exostoses, osteitis condensans ilii, Klippel-Feil syndrome, melorheostosis, spinal stenosis, cervical myelopathy, dacryocystitis, giant cell tumor, fbrous dysplasia, chondrosarcoma, osteosarcoma, synovial chondromatosis at the mesodermal level; facial abnormalities, hare lip, dental abnormalities, dermatofibrosis lenticularis disseminata, keloid formation, and plantar and palmar keratomas at the ectodermal level.7-10 None of these developmental abnormalities were seen in our patient.
Whenever uniform multiple radio opaque lesions are found on radiographic examination, osteopoikilosis must be in the differential diagnosis before invasive diagnostic procedures and dangerous and unnecessary treatments are planned.
None.
None.

©2017 Ali. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.