MOJ
eISSN: 2374-6939


Research Article Volume 7 Issue 4
Lecturer of orthopedic surgery, Suez Canal University, Egypt
Correspondence: Mohamed Nabil, Lecturer of orthopedic surgery, Suez Canal University, Ismailia, Ring Road, Suez Canal University Hospital, Egypt, Tel 1009797107
Received: January 03, 2017 | Published: February 23, 2017
Citation: Nabil M (2017) Dual Mobility Cups in Primary Total Hip Arthroplasty for Patients at Risk of Dislocation. MOJ Orthop Rheumatol 7(4): 00277. DOI: 10.15406/mojor.2017.07.00277
Introduction: Dislocation after total hip arthroplasty (THA) is a cause of much morbidity and its treatment has significant cost implications. Dual mobility cups provide an increased range of movement and may reduce the risk of dislocation. They may be used at primary surgery where the risk of dislocation is high, such as in patients with acetabular deficiency, or those with abductor deficiency.
Objective: To assess the results of dual mobility cups in primary total hip arthroplasty for patients at risk of dislocation.
Methods: Twenty three patients of total hip arthroplasty were enrolled in the current prospective study in the period from October 2012 till December 2014. The inclusion criteria were patients at risk of dislocation such as patients with acetabular deficiency, or those with abductor deficiency. The Harris hip score was used for measuring the outcome of surgeries after a minimum of 24 months post-operative. Of the 23 patients, cemented dual mobility cups were used in 12 patients while cementless dual mobility cups were used in 11 patients.
Results: The SPSS program was used for statistical analysis of the results. The mean Harris hip score improved from 39.4 preoperative to 87.6 postoperative after two years follow up. Two patients had deep wound infection which responded to multiple debridement of the wound and extended intravenous antibiotics according to culture and sensitivity. Another patient experienced deep venous thrombosis two weeks postoperative. No registered cases of dislocation postoperative.
Conclusion: The short term results of Dual mobility cups give a promising outcome in primary total hip replacement for patients at risk of dislocation. A longer period of follow up is recommended for assessment of stability and overall outcome.
Keywords: Dual mobility cups, Total hip arthroplasty, Dislocation
DMCs, Dual Mobility Cups; ASA, American Society of Anaesthesiology; DM, Diabetes Mellitus
Total hip arthroplasty is a satisfactory solution for improving function and quality of life. Though, dislocation, infection and aseptic loosening remain foremost worries. Recurrent dislocation could lead to revision hip arthroplasty and is accompanied with increased risk of complications. The cause of prosthesis instability is multifactorial. Old age, female gender, prior hip surgery, malpositioned prosthetic components, posterior surgical approach and inadequate surgical experience are all linked with high risk for instability. Another chief factor is the indication for surgery i.e. the incidence of dislocation following femoral neck fracture is between 2% and 22% and after primary arthroplasty 1.7% and 3.9%.1-4 After revision arthroplasty the incidence of dislocation rises up to 35%.5,6
Many techniques have been promoted to report the topic of early dislocation. Large prosthetic heads, trochanteric advancement, constrained liners, modular components, constrained and unconstrained dual mobility components are different modalities used to decrease the incidence of dislocation.7 Dual mobility cups (DMCs) have been used to preclude dislocations in patients at risk, such as in revision arthroplasty or in primary procedures for osteoarthritis or fracture of femoral neck in patients with neuromuscular diseases or dementia.8-13 These studies have shown promising results. However, most of these studies come from university hospitals with high rates of surgery or by authors linked with the inventing centers.9,12,14
The aim of the current study was to evaluate the early results in a group of patients at risk treated with dual mobility cups (DMCs).
Patients and methods
Twenty-three consecutive patients (12 females, 11males) with ages ranged from 34 to 63 years (mean: 56.6) were operated with DMCs between October 2012 and December 2014 at our hospital. The inclusion criteria were patients at risk of dislocation such as patients with acetabular deficiency, prior acetabular fracture fixation, high demanding physical activity patients, or those with abductor deficiency.
The American Society of Anaesthesiology (ASA) score of the treated patients was I in 4.3%, II in 47.9%, III in 43.5% and IV in 4.3%.15
Surgical procedure
Of the 23 patients, cemented dual mobility cups were used in 12 patients while cementless dual mobility cups were used in 11 patients. All stems were cementless. One patient required a cage and femoral head allograft to reconstruct the acetabulum during surgery then a cemented DMC was applied. All patients were put in the lateral decubitus position for surgery. At the operating theatre surgery was performed with sterile disposable draping and plastic adhesive coverings over the incisional area. The lateral approach was used in all patients.16
Postoperative care
Prophylactic subcutaneous low molecular weight heparin daily was given for 35 days postoperatively. The sutures were removed at two weeks after surgery. X-rays were taken immediately postoperatively, one, three months, and one year after surgery. With the help of a physiotherapist, all patients were encouraged to start partial weight bearing during the first week post-operative. Full weight bearing was started after 4 weeks post-operative.
Follow up
Follow up of the patients continued for at least 24 months post-operative.
Results
The postoperative radiographs of the operated DMCs showed a mean cup inclination of 46 degrees (SD = 7) and an anteversion of 21degrees (SD = 8) (Figures 1-4).
No periprosthetic fractures were encountered during the two-year follow-up.
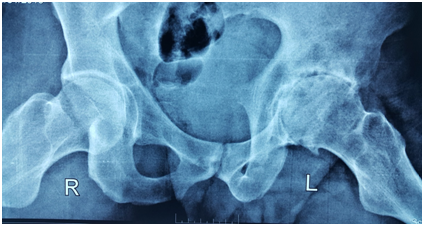
Figure 1a Preoperative x-ray of a 39 y. man with severe arthritis of left hip due to Ankylosing spondylitis.

Figure 3a preoperative x-ray of a 37 y. female with post traumatic and post infection resorption of right femoral head and posterior wall of acetabulum.
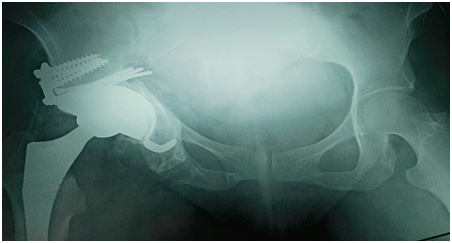
Figure 3b Postoperative x-ray showing total hip replacement using femoral head allograft to reconstruct the posterior wall of acetabulum, cementless cage, cemented dual mobility cup, and cementless stem.
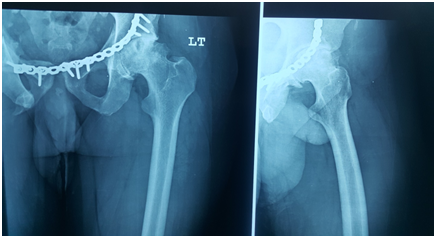
Figure 4a Preoperative x-ray of 42 years old male patient showing left hip arthritis with avascular necrosis following open reduction and internal fixation to treat previous acetabular fracture.
The mean Harris hip score improved from 39.4 preoperative to 87.6 postoperative after two years follow up.
One patient experienced deep venous thrombosis two weeks postoperative which required prolongation of anti-thrombotic therapy for 3 months, and the condition improved after that.
Hip arthroplasty to be successful rests on the biomaterials consumed in bearing surfaces. The customary ceramic on ceramic and metal on polyethylene res ascertained to be durable with low wear rate. The introduction of DMCs, where the bearing surfaces involved polyethylene on metal articulation, generated some inquiries. Adam et al., verified a volumetric polyethylene wear of 54.3 mm3 annually in cementless DMCs, which is comparable to traditional metal-on-polyethylene bearings with 22 mm heads.17 Moreover, studies of long-term survival of these cups are scarce and chiefly come from French centers.18 The first productions DMCs utilized in primary hip arthroplasty were assessed by Vielpeau et al.13 who stated 84.4% endurance with mean follow up of 16.5 years.13 Following revision hip arthroplasty, Leiber Wackenheim et al.11 reported a survival rate of 98% after 8 years follow up.11 More studies are needed to state the topic of long term survival of the new productions of DMCs.
In the current study, the dislocation rate was nil. Accurate positioning of the components looks to be a major factor in preventing dislocation beside the intrinsic stability of these cups. I think the DMCs gave the early stability anticipated for this high-risk group of patients (muscle weakness, severe dementia, psychiatric disorders, and neuromuscular disorders). Nevertheless, the assessment of unstable hip prostheses is a difficult task and must comprise a detailed analysis of the patient and prosthesis. Factors such as interposition, local soft-tissue defects, or prosthesis malposition or improper sizing such as decreased offset, cup retroversion, or bad inclination must all be well thought-out and managed.
The minimal available diameter of DMCs is 42 mm. This must be considered when preparing to operate a patient with small acetabulum, for instance, dysplastic hip. In such case, DMCs should not be the accurate choice.
Alongside DMCs in managing early hip instability, other choices comprise large diameter femoral heads and constrained prostheses. Constrained prostheses are chiefly used as salvage operations for recurrent dislocation.19 Restriction of this choice is the narrow range of motion and a high rate of long term failure due to aseptic loosening.19 Prostheses with Large heads (36-40 mm) were used both in primary and revision surgery to achieve increased stability. Former studies have reported decreased dislocation rate in primary total hip arthroplasty in patients at risk but with an elevated risk in revision surgery compared to conventional implants.20,21 This might be explained by the release of polyethylene micro-particles off the liner, which finally leads to aseptic loosening.21 The dislocation rate reached 13.7% when using large heads in revision hip surgery due to recurrent dislocation.22
In the current study, all patients had prophylactic antibiotics both pre and postoperative; in spite of this, the rate of superficial and deep infections in the present study was elevated than the usual rate of 2-3%. Two patients (8.7%) were operated with debridement and suction-lavage irrigation system with antibiotics. The treatment was successful in all patients and no prosthesis revision was needed. The high infection rate in the current study could be attributed to the selection of patients with co-morbidities (mainly diabetes mellitus, psychiatric, and heart failure). This highlights the significance of perioperative care to improve the medical status preoperatively and wound healing postoperatively.
The final evaluations by Harris Hip Score in the current study were comparable with those reported by Gotze et al. after obtaining their results of revision hip arthroplasty with DMCs.23 Nevertheless, Liber Wackenheim et al.11 Guyen et al.24 presented better Harris Hip Score results than in current study.11,24 This could be explained by the high rate of postoperative infections in the current study.
The use of DMCs in patients at risk shows promising outcomes. The dual mobility cups could offer the desired early hip stability. This could be of interest to orthopaedic surgeons working with a comparable sized departments and caseloads as ours, even if previous studies have shown the importance of large caseload volume, which has been associated with a lowered risk for complications and mortality.25 Furthermore, postoperative complications such as superficial and deep infections are a concern in these patients and must be managed carefully.
None.
None.

©2017 Nabil. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.