MOJ
eISSN: 2374-6939


Case Report Volume 7 Issue 1
Department of Orthopaedics, Amphia Hospital, Netherlands
Correspondence: LJ de Haan, MD, Department of Orthopaedics, Amphia Hospital, Postbus 90158, 4800RK, Breda, Netherlands
Received: July 24, 2016 | Published: January 3, 2017
Citation: Haan LD, Somford MP, Borne MP (2017) Surgical Treatment of Scapular Osteochondroma. MOJ Orthop Rheumatol 7(1): 00255. DOI: 10.15406/mojor.2017.07.00255
Scapula, Osteochondroma, Exostoses, Shoulder
Osteochondromas are most commonly (90%) distributed at the metaphysic of the long bones. However, many other locations have also been described.1-3 Cases of osetochondromas at the scapula, also known as exostoses of the scapula, have been described previously in the literature.1 Clement et al showed an incidence of 3.2% of scapula exotoses in a series of 5361 palpable exotoses. In case of a scapula exostosis there is a higher need for surgical excision (odds ratio 3.7) relative to all other exostoses, this because the location gives rise to mechanical complaints.2 Usually osteochondromas occur on the ventral surface of the scapula and are painless, but mass effect might cause pain, limited range of motion, nerve impingement syndromes, subacromial impingement syndrome and static winging of the scapula.2,4-6 Osteochondroma is the most common benign tumor of the scapula and increases in size as the skeleton grows, but normally does not grow anymore after skeletal maturity.7 If an osteochondroma becomes symptomatic due to growth after skeletal maturity, there is a reason for concern. Such growth can be caused by malignant transformation.8 Benign bone tumors are known to have a cartilage cap of <2 cm. If a magnetic resonance imaging (MRI) shows a cap of >2 cm in thickness raises concern for malignant transformation.8 Lifetime risk of malignant change of osteochondromas in general is 2-4%.2 Only few studies of the surgical treatment, open or arthroscopic, of ventral scapular lesions exist, and the optimal operative approach has yet to be determined. We describe the case of a 33-year-old man with a symptomatic scapular osteochondroma who underwent successful surgical excision with minimal damage to the surrounding muscular structures.
In our outpatient department a 33-year-old male presented with complaints of continuous pain around his right shoulder and scapula. The pain developed gradually over the last 2 years, making it impossible to sleep on his right shoulder and he had complaints of pain during daily labour. When moving his right shoulder, crepitation was noted by the patient around the right scapula. Family history was not contributory and there was no history of trauma. A clinical examination showed an asymmetry of his scapulae with a wing-like prominence of his right scapula (Figure 1). Scapulothoracic crepitus was noted when abducting his right shoulder. A full range of motion was found in both shoulders. Radiographic evaluation showed an irregular bony structure extruding from the scapula (Figure 2). Computed tomography (CT) revealed an osteochondroma along the medial border on the ventral surface of the right scapula (Figure 3). In addition a magnetic resonance imaging (MRI) was performed, showing a bone lesion originating from the anterior side of the scapula with slight bursa formation, most likely to be an osteochondroma (Figure 4). There were no signs of malignant transformation. Since the lesion prevented the patient from performing his job and the complaints of his shoulder worsened over time, surgical resection was proposed.



Figure 1 Clinical photographs with
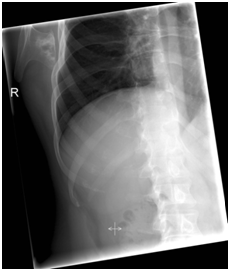
Figure 2 Pre-operative radiograph of the right shoulder, showing bony mass arising from the infro medial region of the scapula.

Figure 3 CT-scan of the right shoulder showing a osteochondroma of the scapula arising from the anterior surface of the scapula.

Figure 4 MRI of the right shoulder showing a osteochondroma of the scapula with a small cartilage cap.
Surgical procedure
Under general anaesthesia, the patient was placed in a left lateral decubitus position with a full range of motion of the right shoulder (Figure 5). A parascapular incision was made alongside the medial border of the right scapula. Sharp dissection was carried out down to the level of the fascia of the trapezius muscle. After opening the fascia the trapezius muscle was retracted cranially. The exostosis was palpable through the rhomboid muscles. The rhomboid was split bluntly in line with the fibers. Subperiosteal dissection allowed full exposure of the exotosis (Figure 5), which was excised at the base with an osteotome from the ventral surface of the scapula. The specimen measured 45 x 54 x 14 mm (Figure 5). When palpating the ventral side of the scapula a small pedicel was felt and removed. Rhomboid fibers fell back against each other after removal of the exostosis. After closure of the trapezius fascia, the wound was closed in layers. Histologic examination confirmed that the specimen was an osteochondroma with no signs of malignant transformation. A sling was applied for one week. Above shoulder exercises was restricted for 6 weeks postoperatively. The shoulder was mobilized as was tolerated with guidance of a physiotherapist. After 6 weeks the range of motion was expanded. Almost immediately after surgery the patient experienced improvement of the pre-operative pain and after two weeks the pain was completely gone. Clinical examination at 6 weeks showed a full range of motion. At 3 months, postoperative the patients were back at work without any symptoms or restrictions of his shoulder. At 6 months follow up the patient was still without any symptoms.
Comprising 35.8% of all benign bone tumors, osteochondroma is the most common benign tumor of the bone.8,9 90% occur in tibia, humerus and distal femur.8-10 The scapula is involved in 3.0-6.4% of all cases. The osteochondroma usually arises on the anterior surface of the scapula.2,7,9,11-13 The osteochondroma of the scapula causes pain and a grating sound during movement of the scapula. Symptoms result from mechanical irritation of muscle, tendon or soft tissue, formation of a pseudo aneurysm or bursa, fracture, or malignant transformation.6,8,9 These symptoms can be a scapula alata, scapular dyskinesia and/or a reduced range of motion of the shoulder.5,9 If a patient is symptomatic surgical remove is an excellent treatment. There are different operative techniques. They can be divided in 3 major groups: muscle detaching, muscle saving and endoscopically assisted techniques. In our case we used a muscle saving technique, without detaching any of the muscles from their origin to ensure a better postoperative recovery. Forst et al.7 & Sivananda et al.10 both described to either elevate to and Chillemi et al.14 chose to detach the rhomboid and/or trapezius muscle from their insertion and re-attach them later. No attachment techniques were described in their papers. In the recent literature there is no consensus about the postoperative rehabilitation. Protocols range from starting full range of motion one day after surgery to immobilization of the shoulder for 3 weeks with only pendulum exercises and then starting with mobilization of the shoulder. All cases show a good to excellent result after 6 to 24 months. In our case the surgical removal of an osteochondroma of the scapula showed excellent result while using a muscle saving operation technique. In our opinion in case of an osteochondroma of the scapula there should always be made an MRI pre-operatively to evaluate the size of the cartilage cap to assess possible malignant transformation. CT scan can be helpful in preoperative planning. After resection a quick start of functional rehabilitation seems to be well tolerated and will contribute to quick and good functional results.15,16
The diagnosis osteochondroma of the scapula should be considered in any patient with scapular pseudowinging, crepitus and pain of shoulder region. In adult cases a MRI of the scapula is recommended, to assess possible malignant transformation. Good clinical outcome can be expected using muscle-sparing technique with a quick functional rehabilitation of patients with a symptomatic osteochondromas.
None.
None.

©2017 Haan, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.