MOJ
eISSN: 2374-6939


Case Report Volume 4 Issue 6
1Department of Orthopedics, Queen's University, Canada
2Department of Orthopedics, King Fahad Specialist Hospital, Dammam, Saudi Arabia
Correspondence: Hamad Alshahrani, Queen's University, Canada, 76 Stuart Sreet, Kingston, K7L 2V7, Canada, Tel 647-997-7720
Received: February 24, 2016 | Published: May 5, 2016
Citation: Alshahrani H, Wood GCA (2016) Treatment of Avascular Necrosis of the Femoral Head with Bone Graft and Interference Screw. MOJ Orthop Rheumatol 4(6): 00159. DOI: 10.15406/mojor.2016.04.00159
Osteonecrosis, also known as avascular necrosis or ischemic necrosis of the femoral head, is a severe deficiency of blood supply to the femoral head and can lead to collapse and joint destruction.1,2 Osteonecrosis is a disease arising from impaired osseous blood flow which can follow traumatic or non-traumatic conditions. Originally it was thought to be secondary to infection, but negative bacteriological studies led to the use of the term aseptic necrosis. Further studies showed that the necrotic bone was not only sterile but also avascular, hence the terms ischaemic necrosis, avascular necrosis, and bone infarction.
Many factors with strong associations have been identified, including long term or high dose steroid use, moderate to heavy alcohol consumption, trauma, blood clotting disorders, and so on.
Osteonecrosis of the femoral head occurs predominantly in younger patients, and without treatment most of them suffer from collapse of the femoral head and painful arthritis of the hip joint within several years. The ideal goal of early treatment is to delay or arrest the progression of the disease before articular collapse occurs. It has been well documented that without specific treatment approximately 70% to 80% of hips with clinically established avascular necrosis have radiologic and clinical progression, which leads to collapse of the femoral head.3-5
Many factors affect treatment decisions, i.e. disease stage, the presence of collapse, acetabular involvement, size and site of the lesion. Pre-collapse disease has a better prognosis and may require less invasive intervention, but once collapse has occurred treatment options become more limited and invasive intervention becomes more likely.
A variety of surgical therapies have been investigated in an attempt to halt the progression of the disease. Surgical therapies include core decompression6,7 to relieve compression caused by interstitial edema and improve vascularity . Core decompression procedures have been performed alone, or with various forms of vascularized bone grafting, electrical stimulation, and other adjuvant therapies. The rate of clinical success of these combined surgical procedures has ranged from 33% to 95%.5
We present a case of early osteonecrosis of the hip (Ficat stage II) treated by core decompression and followed up for close to 12 months. To prevent the mechanical failure of the subchondral bone and articular collapse, we used cancellous allograft soaked in patients own blood impacted up the core decompressing channel and utilized an absorbable Interference Screw to hold the graft in place. Theory being to strengthen structural mechanics of the femoral head, provide structural support of articular cartilage bring in osteoblasts and cell mediators whilst decompressing or coring out the devitalized bone and encourage new bone formation.
A 45-year old female was admitted with symptoms of joint pain of 1 year duration in both hips. The left was involved more than the right. The hip pain was so intense the patient could not carry on her routine duties. Her past medical history revealed a long history of Bronchial Asthma attacks requiring high dose of prednisone. Clinical evaluation minimal restriction of hip joint movement especially internal rotation. Plain radiographs of the pelvis were normal with Bilateral femoral head avascular necrosis is present with no collapse on the left hip (Figure 1), whereas an MRI scan revealed the avascular necrosis involves an area measuring 3.9 cm mediolateral x 3.8 cm AP. There is mild edema in the left femoral head and neck. No subchondral bone depression identified overlying the avascular necrosis at the left hip.
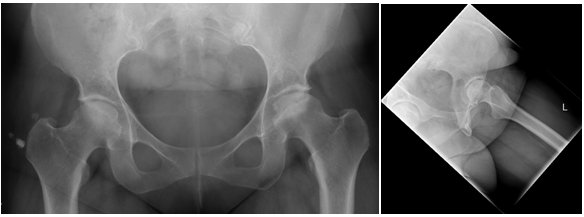
Figure 1 Preoperative AP of both hips and Lateral radiograph of left avascular necrosis changes with a sclerotic rim and no femoral head flattening.
Patient was thereafter counseled and prepared for surgery. 3.2mm guide pin was inserted through the lateral cortex into the centre of the osteonecrotic portion of the femoral head. DHS core reamer was placed over the guide pin and this was drilled to within 5 mm of subchondral bone. Bone graft was inserted into the defect just lateral to the sclerotic bone defect visualized on fluoroscopy. Then we inserted a 9 x 25 mm bio absorbable interference screw into the neck containing the bone graft (Figure 2).
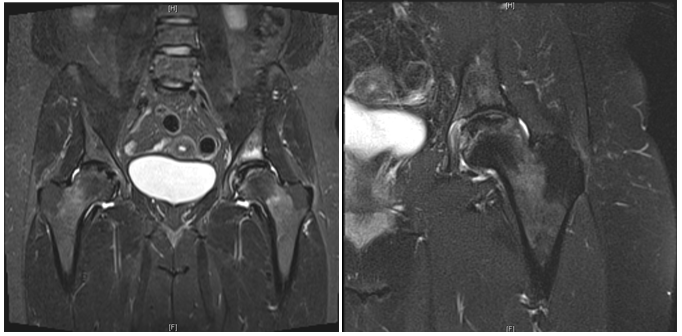
Figure 2 Preoperative MRI with left hip avascular necrosis .There is mild edema in the left femoral head and neck. No subchondral bone depression identified.
Immediate postoperative period was uneventful and the patient was mobilized non -weight bearing and was discharged on crutches. Subsequent follow up over the twelve month has been uneventful Figure 3.
She reported a marked improvement in her pain and function. In her clinic fellow up, x-ray (Figure 4) showed a slight deterioration from before, but there seems to be some consolidation and there has been no further collapse in view of her clinical presentation [Figure 5,6].
She did well for almost 18 months then she start to have pain in her left hip with limited activity. She underwent total hip replacement after 2 years from core decompression. Intra operative finding showed mild flattening of femoral head at weight bearing area without significant collapse [Figure 7,8].
Core decompression was described by Arlet and Ficat in 1964.8 By 1980, they had performed more than 800 cases.2,9 In 1985, Ficat 4 reported on 133 hips with Stages I and II disease treated by core decompression. He reported “good to very good results” in 90% of these hips on clinical evaluation and in 79% on radiographic evaluation.
Originally it was used to obtain histological samples to aid diagnosis of patients with hip pain. The procedure involved removing a central core of 8-10 mm with a hollow biopsy trephine followed by venography to confirm an abnormal pattern of blood flow within the femoral head. Bone marrow pressure was measured and found to be consistently elevated in patients with osteonecrosis. The procedure also gave pain relief which was what lead to its use therapeutically rather than purely a diagnostic procedure.
Bone grafting procedures offer many advantages for the treatment of pre-collapse lesions and early post collapse osteonecrosis of the femoral head, when the articular cartilage is not damaged. It allows decompression and removal of necrotic bone, can provide structural support, act as scaffolding for repair and allow remodeling of subchondral bone.
This case report attempted to integrate several treatment principles in avascular necrosis. We used interference screw loaded with DBM to treat the early-stage of femoral head osteonecrosis. The goal is to tip the balance of the creeping substitution process by accelerating bone healing while providing enough structural support to the articular cartilage. The rationale for the procedure is based on the following hypotheses:
There have been many studies looking at whether core decompression alters the natural history of osteonecrosis.
In a retrospective literature review encompassing 42 reports with 2025 patients, Mont et al.4 found satisfactory clinical results in only 22.7% of the patients treated conservatively but in 63.5% of those treated with core decompression.4 The rate of progression to a total hip replacement ranges from 31% to 57%. Vascularized bone grafts have been shown to incorporate more rapidly and predictably than non-vascularized grafts.10
Steinberg11 is applying his classification retrospectively, assessed 297 hips in 205 patients who had received core decompression and cancellous bone grafting into the core tract followed for two years. He felt that the site and stage of the lesion influenced the results of core decompression. Total hip arthroplasty was required in 22% of the stage I and II hips with small area of involvement (stage IA and IIA, less than 15% head involvement). In contrast 39% of the stage-I hips and 40% of the stage-II hips with involvement of _15% of the head (stage IB, IIB and IIC) eventually required total hip arthroplasty.
In the past several authors have attempted to augment a standard core decompression procedure. Soucacos et al.12 tried to update core decompression with homogenous variant bone grafting for structural support of the femoral head.12 Then Berend et al.13 improved this technique. They utilized the core decompression channel for autogenous or homogenous fibular or iliac grafting. Though the short term result was excellent, in the long-term the survival rate of the femoral head was low. Recently, Plakseychuk et al.14 retrospectively compared the results for 50 hips treated with a free vascularized fibular graft performed at the University of Pittsburg Medical Center, and 50 hips treated with a non-vascularized fibular graft performed at the Kyungpook University Hospital in Korea.14 After an average follow up of 5 years the mean Harris hip score had improved in 70% and 36% of hips respectively.
Leali15 reported a modified core decompression procedure combined with the insertion of two interference screws into the subchondral plate to provide structural support and the use of osteoinductive material (i.e., demineralized bone matrix) in an effort to accelerate the bone healing process, but the document was only a case report without follow-up of the patient .
The elevated intra osseous pressure is relieved with a standard core decompression which also improves vascularity and relieves pain. The structural deficit is addressed with the use of bone graft and interference screws. The bone healing process is accelerated with the incorporation of osteo inductive material into the drilled tracks in the depth of the subchondral bone. The goal is to tip the balance of the creeping substitution process by accelerating bone healing while providing enough structural support to the articular cartilage. The advantage of this technique allows us to follow principles of grafting with core decompression without the co-morbidity of vascularized graft and easy conversion to THA with simple neck cut as compared to other methods. Neck cut and finding the IM canal in femur can be difficult and misdirect broaches when fibular struts or other such large bone incorporating devices are used. E.g. tantalum
None.
None.

©2016 Alshahrani, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.