MOJ
eISSN: 2374-6939


Case Report Volume 3 Issue 6
Department of Orthopedic Surgery, Hospital Santarem, Portugal
Correspondence: Tiago Paiva Marques, Knee and Shoulder Surgery, Hospital Santarem, Portugal
Received: December 01, 2015 | Published: December 9, 2015
Citation: Marques TP, Moita MB, Babulal J, Mendes F (2015) Arthroscopic Patellar Plication: An Option for Patellar Instability with Femoral Trochlear Dysplasia. MOJ Orthop Rheumatol 3(6): 00114. DOI: 10.15406/mojor.2015.03.00114
There is no consensus on the optimal surgical technique for recurrent patellofemoral instability with femoral trochlear dysplasia. We report a case of a 28th years old female with history of nontraumatic patellar instability of right knee. The patient had major limitations in the activities of daily living - Lysholm score 28 and Subjective IKDC 33- and stopped sports. Clinically she had patella instability, pain and quadricipital atrophy. Image study showed femoral trochlear dysplasia, external translation of the patella and chondromalacia.
After failed conservative treatment she was submitted to an arthroscopic medial patellar plication. She is now 2 years post op, doing sports, and with high quality of life - Lysholm score of 90 and Subjective IKDC of 87. There are few reports on treating patella instability with underlying femoral trochlear dysplasia with arthroscopic soft tissue procedures. This case underlies this option as a good treatment choice to this problem.
Keywords: Patella instability; Patella placation; Arthroscopy; Femoral trochlea dysplasia
IKDC: International Knee Documentation Committee; MRI: Magnetic Resonance Imaging; CT: Computer Tomography; TT-TG: Tibia Tuberosity Trochlear Groove; NSAIDs: Non Steroid Anti-inflammatory Drugs
There is a paucity of data analyzing arthroscopic soft tissue procedures for stabilizing the patella in the context of instability and underlying femoral trochlear dysplasia; but the results seems to be good in low-grade dysplasia. We report this case as good example for using this straightforward, minimally invasive technique, to address a complex problem.
A 28-year-old female patient presented with history of pain, swollen knee and major limitations in the activities of daily living. She had pain for 8 to 10 years but was mild, and no limitations on regular or sportive activities. In the last months the pain and the limitations on regular activities escalade. In the physical examination the patient had quadricipital atrophy, more than 50% lateral patella translation, positive lateral tilt test, positive grind test and painful facet palpation. We evaluated the Lysholm and Subjective IKDC scores, and she had 28 and 33 points respectively.
Knee radiograph evaluation (Figure 1 & 2) demonstrated a trochlear groove angle > 145º and type III patella according to the Wiberg classification as well as a crossing sign; there were no arthritic changes and no patella alta or baja; CT scan (Figure 3) showed femoral trochlea dysplasia, normal TT-TG, patella external translation and patella chondromalacia; MRI had the same findings as the CT and reported normal menisci and ligaments.
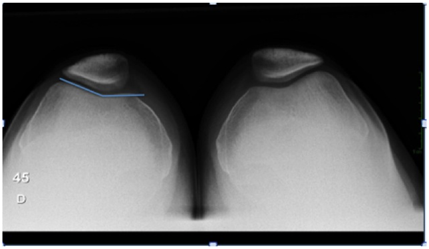
Figure 1 45º x-ray patellofemoral view (Merchant view) demonstrating trochlear groove angle > 145º and type III patella according to the Wiberg classification.

Figure 2 X-ray knee lateral view showing crossing sign (circle) and normal patella height by Insall-Salvati ratio (lines); no arthritic changes are seen.
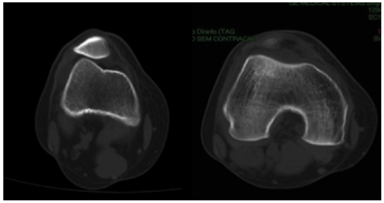
Figure 3 Knee axial CT scanning; Patella tilt and translation (left) and type a trochlear groove dysplasia (right).
The patient was diagnosed with patellar instability with external translation and trochlea dysplasia type A.
The patient underwent 5 months of physical therapy along with self-rehabilitation exercises, oral NSAIDs without any improvement.
After failed conservative treatment the patient was submitted to an arthroscopic all inside medial patellar plication (Figure 4 & 5). This technique was made with two standard lateral and medial portals and one accessory superolateral portal; we placed a working cannula in this portal. Standard diagnosis arthroscopy was made and then with leg in extension the patellofemoral compartment was approached. There was synovitis, type 2 patellar cartilage lesions and maltracking of the patella was observated. A partial synovectomy and debridment of cartilage lesions with shaver blade was made and then we did the arthroscopic medial plication with lateral retinaculum release. The medial retinaculum became tense and the patella was aligned in the trochlear groove, with lateral translation inferior to 50%.
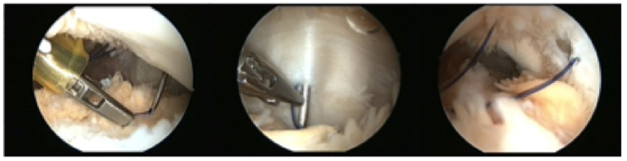
Figure 4 Intra operative arthroscopic images showing the suture limbs being passed in the medial retinaculum over the Tuohy needle, and the final aspect before knot tying, after the synovial abrasion between suture limbs
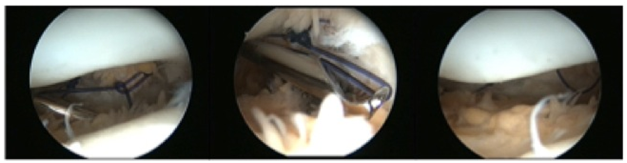
Figure 5 Intra operative arthroscopic images showing knot tying and the final image after the medial retinaculum plication.
The patient was discharged day after the surgery and initiated auto rehabilitation exercises and formal physical therapy rehabilitation. Returned to sports activities between the 3rd and the 4th post op month.
At 2 years follow-up the patient has just residual complaints in her activities of daily living, returned to sports with no major limitations or complaints. She had no episodes of significant pain and swollen knee. The physical examination repeated at follow-up consults showed no major instability, with less than 50% lateral translation, absent pain with patella manipulation and facet palpation. The Lysholm score was 90 and Subjective IKDC score was 87. Post operative CT scan showed aligned patella (Figure 6). The patient is very satisfied with the surgical outcome until this date.
This is a case of patellar instability with medial retinaculum insufficiency, a tight lateral retinaculum with a normal TT-TG and a trochlear dysplasia type A. We know from the literature that medial patellofemoral ligament is responsible for up to 60% of the patella lateral restraint.1,2 Fulkerson et al.3 reported that the medial patellofemoral ligament heals but sometimes elongated and the basis for the arthroscopic medial plication is based on the principle of the Bankart surgery for the shoulder.4 This technic was first described in 2001 by Hallbrecht.5 and his follow-up report in 2009 of those patients showed good results.5 Several reports comparing open plication.6,7 arthroscopic assisted .8,9 and arthroscopic plication.10 reported similar results between them. There are some references concerning the use of this technic in patients with trochlear dysplasia, like the study of Schottle et al.11 reporting similar results when comparing low grade dysplasia (Type A and B) and patients with no dysplasia. The advantages of arthroscopic technique are: avoid big incisions, protect VMO muscle, less post operative pain, visualize realignment, avoid overtightning, lower risk of complications, lower risk of stiffness and scar tissue, easier rehabilitation and more cosmetic.12 In our case, a good result was obtained with a low risk, aesthetically friendly and less invasive technic.
None.
None.

©2015 Marques, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.