MOJ
eISSN: 2374-6939


Research Article Volume 1 Issue 3
Department of Surgery, Pakistan
Correspondence: Muhammad Ali, Department of Surgery, Agha Khan University, Block-I, House no -4 shahruknealam colony Multan, Karachi, Pakistan, Tel 923215470768
Received: September 29, 2014 | Published: November 9, 2014
Citation: Ali M, Wajid MA. Early results of three and four part proximal humerus fractures treated with PHILOS (Proximal Humerus Interlocking System) plate. MOJ Orthop Rheumatol. 2014;1(3):58-61. DOI: 10.15406/mojor.2014.01.00016
Achieving stable fixation has been a challenge in proximal humerus fractures. PHILOS (Proximal Humerus internal locking system) is the latest generation of locking compression plate system for such fractures. The aim of the current study was to assess the clinical and functional outcome of proximal humeral fractures (3-part and 4-part) treated with the PHILOS plate. This was a retrospective review of first ten cases operated at our centre by a single surgeon. The patients were followed in out-patient clinics till fracture union. Fracture healing was assessed by clinical and radiological criteria, and shoulder function was evaluated using Constant and Murley score. Average follow-up was 23±3 weeks. Eight (80%) patients had fracture healing at an average of 11.6±0.8 weeks post-operatively, and gained moderate range of motion. Two (20%) patients had complications, i.e. one had deep infection and another had screw pull-out.
Conclusion: Open reduction and internal fixation with PHILOS plate showed acceptable functional outcome. Apart from the one case with screw-pull-out, our early results using this plate are encouraging, with no other implant-related complications and good early healing.
Keywords: Proximal humerus fractures, internal fixation, locking compression plate, PHILOS Plate
PHILOS, Proximal Humerus Interlocking System
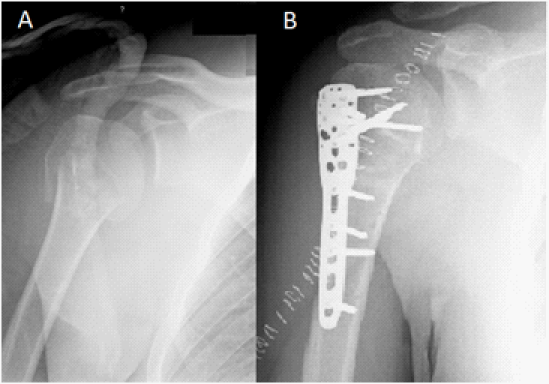
Fractures of the proximal humerus account for 4% to 5% of all fractures.1–3 In patients over 65 years of age, they are the second most common upper-extremity fracture and the third most common fracture after hip fractures and distal radial fractures.1,4,5 Although most such fractures can be managed non-operatively, operative intervention is generally recommended when any of the major fracture fragments is displaced more than one centimeter or angulated more than 45°.1,3,6 Open reduction and internal fixation for multi-fragmented proximal humerus fractures in adults with good quality bone are not usually a problem.7–9 However in osteoporotic bones, these injuries present a real challenge.7,10 The main issue is stability of the construct; due to poor anchorage of screws in humeral head, there is a high risk of screw pullout.11 Angular stable devices such as the Proximal Humerus Interlocking System (PHILOS; Synthes, Oberdorf, Switzerland) were developed by the AO Foundation (Figure 1) provide better anchorage and superior stability.5,12 In the Aga Khan University, PHILOS was introduced into clinical practice in April 2007. In this study we present our early experience of the use of this system for 3-part and 4-part fractures of the proximal humerus.
Patients with three and four part fractures of the proximal humerus who were treated surgically between April and November 2012 using PHILOS were included in the study. Ten such cases, all presenting after acute injuries and operated by a single surgeon, were identified through the hospital medical record system and chart review. A data collection form was used to record information regarding patient demography, mechanism of injury, fracture classification, technical details of surgical procedure, post-operative rehabilitation protocol and follow-up assessments.
Follow-up clinical examination in the outpatient department entailed assessment of wound healing, fracture union, shoulder function and pain. Clinical fracture union was defined as fracture site becoming painless, non- tender and stable. Shoulder function was assessed using Constant and Murley scoring system.13 This score assigns points for pain, muscle strength, activities of daily life and range of motion, and is graded as poor (score 0-55), moderate (56 to 70), good (71-85) and excellent (86-100). Follow-up radiographic evaluation entailed assessment of adequacy of fixation, status of the plate and screws, and radiological fracture union in terms of bridging of fracture gap and external callus. All fractures were classified according to AO classification.2 Surgery was performed under general anesthesia with the patient in beach chair position. An image intensifier was used for dynamic fluoroscopic monitoring of the operation. Deltopectoral surgical approach14,15 was used, taking care to protect the axillary nerve and the periosteal/muscular attachments to the bone fragments. The supraspinatus tendon was tagged with multiple #2 braided non absorbable sutures. These tagging sutures were used to bring the tuberosity fragments to the lateral cortex of shaft fragments, thereby indirectly reducing the head fragments to the shaft. In fractures where the medial hinge was disrupted (Figure 2), attempt at restoration of the medial hinge16 was done. If head fragments were impacted on the shaft, a periosteal elevator was used to dis-impact the head and thus restore the medial portion of calcar. A minimum of four screws were placed in the proximal segment.
After reducing the fracture, the tagging sutures were passed through the suture hole of PHILOS. The plate was positioned directly on the middle of lateral cortex, and the proximal end was kept approximately 8 mm distal to the superior edge of the greater tuberosity. By using insertion guide and sleeve assembly, locked screws were placed in the humeral head. The plate was fixed to the shaft with a screw inserted in the neutral slot of the plate, and then subsequent screws were inserted in locking mode. Reproduced with permission from Sperling et al.17
Of the 10 patients, 3 were male and 7 were female. Majority of the patients were elderly or middle aged. The average duration of follow up was 23±3 (range 16-24) weeks. Eight patients had uneventful fracture union at an average of 11.6±0.8 weeks (Table 1). The operated shoulder demonstrated mean forward flexion of 100° and mean abduction of 90°, compared to 168° and 159° respectively in the contra lateral (normal) shoulder. Mean Constant score (Table 2) for the operated shoulder was 62.3 (moderate) as compared to 90.3 for the contra lateral shoulder. Radiographs demonstrated evidence of excellent healing and well positioned implants (Figure 3). None of the patients exhibited radiographic evidence of avascular necrosis at the final follow-up.
Uneventful healing |
8 patients |
Radiological healing time |
11.6±0.8 weeks |
Complication, Requiring hemi-arthroplasty |
2 patients |
Deep infection |
1 Patient |
Screw Cut-out |
1 Patient |
Table 1 Final outcome
According to Constant and Murley score |
|||
Component |
Max. Possible Score |
Patients’ Score |
Interpretation |
Pain Internal Rotation |
15 10 |
10.6±1.8 (10-15) 6.3±1.3 (4-8) |
Mild |
Total score |
100 |
62.3±6.1 (56-76) |
|
According to Fracture type, Operating time |
|||
|---|---|---|---|
Fracture type |
Number of patients |
Operating time (min)# |
Constant & Murley total score (mean+SD)* |
11-B2 |
2 |
65 ± 7 |
68±11 |
Table 2 Clinical and Functional Outcome. #Increasing time according to complexity of fracture, significant (p=0.021), ANOVA *Trend of decreasing score according to complexity of fracture, though not significant (p=0.206)
Two patients developed complications. One had deep infection which was treated by debridement, removal of hardware and subsequent shoulder hemi-arthroplasty. The other patient had cutout of screws on follow-up at 1st week. This patient was treated by removal of hardware and hemi-arthroplasty. These patients were not included in the follow up. No patient had nerve injury, impingement or plate failure. Operating time varied according to the type of fracture. Thus, for 11-B2 fractures, mean operating time was 65±7 min, for 11-B3 it was 88±9 min and for 11-C2 it was 95±9 min. This variation was statistically significant (p=0.021, ANOVA).
Rehabilitation and follow-up
We started early passive range of motion exercises followed by active exercises at 6 weeks. Resistive exercises were started at 10 weeks.
The use of locked plating in the treatment of displaced proximal humerus fractures is becoming more wide spread. Precise knowledge of and experience with the surgical technique is required to maximize clinical outcomes, including appropriate preoperative and postoperative management. While this emerging technique has shown promise to date, surgeons should be aware of complications that can arise. Overall complication rates have been reported as high as 81% in the literature, depending on the definitions used, but significant variability has been present across studies.10–13,15
In general, non-operative treatment of displaced three- and four-part fractures of the proximal humerus, which form 13%-16% of proximal humeral fractures, leads to poor outcome due to intra-articular nature of injury and inherent instability of the fragments.3,5 A careful assessment of the patient in terms of age, activity level, bone quality, fracture pattern, degree of comminution and vascular status of the fracture fragments is required before committing to the type of treatment to be used in a particular patient.7,8 Operative treatment is challenging in terms of fixation and stability of construct in comminuted fractures and osteoporotic bone.3,7 This is a fairly common scenario in elderly patients, in whom osteoporosis leads to comminuted fractures of the neck and head of humerus. Conventional plating in such fractures leads to unacceptably high incidence of screw pullout.5 From historical comparisons and biomechanical evaluation of locked internal fixator we know that pull out strength of locked head screws is better than conventional screws due to the axial and angular-stability of screws.11,12 The PHILOS, and modified cloverleaf plate with locking head screws are examples of new implants analogous to locked internal fixators.4,5,12 The combination of locking head screws with three dimensional positioning of the screws within the humeral head leads to improved stability. Fractures of the AO-type 11-A3, 11-B2, 11-B3, 11-C2 and reconstructable 11-C3 fractures have been the most frequent indications for fixation with this new system.2 Although PHILOS has superior stability compared to conventional plate in fractures in the elderly with osteoporosis, in cases with severely osteoporotic and multi-fragmented fractures, the screws may cut out of the bone despite the locking heads.7 The insertion of this new device is technically demanding; in particular the insertion of the proximal screws entails the risk of perforation of the sub-chondral bone by the screw tip. This is because of the sphericity of the humeral head and misleading assessment of the length of screw under fluoroscopy.14,15 Reconstruction of the medial buttress in the metaphyseal area of humerus is a key point in fixation of proximal humerus with proximal humerus interlocking system.16 If the medial buttress can be restored by indirect technique, this leads to a very stable fixation and allows early range of motion. If there is medial comminution or bone defect, the medial buttress can be restored by impacting the shaft in to head and fixing it in the position with proximal humerus interlocking system.14–16
Open reduction technique and internal fixation with the conventional T- plate requires exact preparation of the fracture fragments in order to seat the plates on to the bone, causing additional damage to the already compromised blood supply and leading to a high rate of avascular necrosis of the humeral head.3,5 The rate of avascular necrosis has been reduced by using minimally invasive approach, indirect reduction techniques and minimal soft tissue disruption.5,18 Anatomically pre-shaped19 implants like the PHILOS generally don’t require contouring and do not need to be seated on the bone, thus eliminating the need for muscular/periosteal disruption. Avascular necrosis may be predicted on the initial fracture radiographs using the Hertel18 radiographic criteria for perfusion of humeral head. According to this criteria, metaphyseal extension of humeral head of <8mm and disruption of medial hinge of >2mm are good predictors of ischemia. These, along with anatomical neck fracture pattern, have a 97% of positive predictive value for humeral head ischemia. Such fractures are better treated using hemi-arthroplasty instead of internal fixation.3,5
Koukakis et al.20 described their experience using the proximal humeral internal locked system (PHILOS) plate in the operative management of proximal humerus fractures. Over a 3-year period, 20 patients with a mean age of 62 years had their fractures treated with this locked plate construct. The authors reported a 100% rate of fracture union. These results are comparable to our study. Apart from the two cases one with screw pull-out and other with deep infection, our results showed that fracture union was achieved in all cases, and none developed avascular necrosis. Moreover, shoulder pain was mild and function was moderate at the final follow-up. The main reason for the “moderate” instead of “good” outcome were the low activity level and inability to achieve abduction and flexion beyond 120°. These could be attributed to the sedentary lifestyle of the patient population who were mostly elderly/middle aged people with low functional demands. In appropriately selected cases, PHILOS appears to provide adequate stability of the fracture fragments and acceptable functional outcome. The limitation in our study was absence of control group of patients treated conservatively or with an alternative device. Secondly, absolute confirmation of screw placement is not possible with biplanar fluoroscopy.
The use of locked plating in the treatment of displaced proximal humerus fractures is becoming more prevalent. The primary goal of surgery should be to create a construct stable enough to allow early ROM of the shoulder. Precise knowledge of and experience with the surgical technique is required to maximize clinical outcomes, including appropriate preoperative and postoperative management. While this emerging technique has shown promise to date, surgeons should be aware of complications that can arise. Our early results on the use of this plate are encouraging, and it appears that use of PHILOS in three and four part humerus fractures, particularly in osteopenic bone, provides acceptable results.
None.
The author declares that there is no conflict of interest.

©2014 Ali, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.