MOJ
eISSN: 2374-6939


Case Report Volume 1 Issue 1
Department of Orthopaedics, Lincoln County Hospital, UK
Correspondence: Fahad Attar, Department of Orthopaedics, Lincoln County Hospital, Lincoln, LN2 5QY, UK, Tel 44-0-1522573151, Fax 44-0-1522573830
Received: May 20, 2014 | Published: May 27, 2014
Citation: Attar F. Radiological outcome of patients with splay foot following 1st and 5th metatarsal osteotomies performed simultaneously on the same foot. MOJ Orthop Rheumatol. 2014;1(1):6-8. DOI: 10.15406/mojor.2014.01.00002
Introduction: There have been many operations documented for the treatment of hallux valgus and 5th metatarsal bunionette deformities in splay foot patients done separately with variable success rates. Our aim was to radiologically assess outcome following both chevrons osteotomy to the 1st and reverse chevrons osteotomy to the 5th metatarsals in symptomatic patients with splay foot. To our knowledge, this procedure has not been described in the literature.
Materials and Methods: 9 symptomatic patients (12 feet) were included in the study. The pre-operative and post-operative angles were assessed on weight bearing X-rays for statistical significance using non-parametric paired T tests.
Results: Hallux valgus angles, intermetatarsal angles, 1st and 5th metatarsal head widths, and maximum distance between 1st and 5th metatarsals head all have significantly decreased post-operatively (p< 0.05).
Conclusion: The results suggest a very good radiological outcome in symptomatic patients following simultaneous 1st and 5th metatarsal osteotomies. All the angles measured except for the DMAA showed a statistically significant reduction post-operatively.
Keywords: Hallux valgus, Osteotomy, Radiography, Tailor's bunion
HVA, Hallux Valgus Angles; IMA, Intermetatarsal Angles; DMAA, Distal Metatarsal Articular Angles
The term “splayfoot” connotes an abnormal widening of the forefoot in relation to the heel. Clinically, the splayfoot is characterized by valgus of the great toe with bunion formation in association with a relative varus position of the first metatarsal. On the lateral part of the forefoot, there is varus of the fifth toe with a relative valgus position of the fifth metatarsal and resultant bunionette formation. This deformity is often associated with metatarsalgia under the second metatarsal head because of its relative elongation in relation to the first metatarsal. Radiologically, splayfoot is characterized by an intermetatarsal angle between the first and second rays of greater than 12°, and an intermetatrsal angle between the fourth and fifth of greater than 8°, the slant of the distal articular surface of the medial cuneiform is more than 105°.1
The hallux valgus deformity in splayfeet is a complex deformity of the first ray that is frequently accompanied by deformity and symptoms in the lesser toes. The angle between the first and second metatarsals is usually more than 8 to 9 degrees. The valgus angle of the first metatarsophalangeal joint is also more than 15 to 20 degrees. Tailor's bunion or bunionette is a term applied to an enlargement of the lateral aspect of the fifth metatarsal head that produces various degrees of pain, swelling, and tenderness. The deformity is located at the dorsolateral or lateral aspect of the fifth metatarsophalangeal joint. Commonly, a splayfoot deformity is associated with a Tailor's bunion deformity.2 In our study, we present the radiological outcome in 9 patients (12 feet) who underwent simultaneous 1st and 5th metatarsal osteotomies, chevron for the 1st metatarsal and a reverse chevron for the 5th metatarsal, to correct the combined hallux valgus and tailor bunion deformities respectively in splayfoot patients. This method of combined treatment has not been previously described in the literature.
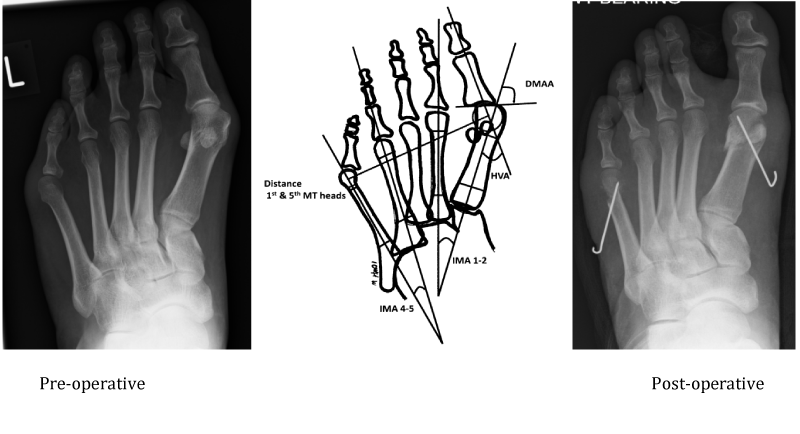
This series study included 9 symptomatic patients (12 feet) with splayfoot deformities. The patient's pre-operative and post-operative weight bearing X-rays (Figure 1) were independently assessed by senior orthopaedic registrars FA and SR. The hallux valgus angles (HVA), 1st and 2nd intermetatarsal angles (IMA 1-2), distal metatarsal articular angles (DMAA), 4th and 5th intermetatarsal angles (IMA 4-5), maximum widths of the 1st and 5th metatarsal heads and the maximum distance between the centers of the 1st and 5th metatarsals were calculated. The change in the angles and distances post-operatively were then assessed for statistical significance using non-parametric paired t-tests. Patients were followed up and assessed at 6 months and at 48 months post-operatively. The operative procedure was carried out by the senior author.
Operative technique: The procedure was carried out under general anesthesia with an ankle tourniquet, 1st metatarsal osteotomy was performed first using a medial incision through the skin and capsule. Dorsal and plantar capsular stripping was kept to a minimum. A medial exostectomy followed by a standard chevron osteotomy was performed. The head was displaced between one third and half the width, depending on the extent of the deformity. The osteotomy was held using a 1.25 mm Kirschner wire. The foot was then placed in a standard hallux bandage.
Similarly lateral longitudinal incision through the skin and capsule for fifth metatarsal head and neck was carried out. Lateral exostectomy followed by chevron osteotomy through the neck of fifth metatarsal was performed. The head displaced to the required extent and held with 1.25 mm Kirschner wire. The foot was then placed in a standard hallux bandage. Post operatively heel weight bearing was allowed in a forefoot protecting surgical shoe. At 4 weeks post operatively, the K wire was removed and full weight bearing allowed. Overall follow up with weight bearing x-rays was at 6 months and then again at 48 months.
The results of the pre-operative and post-operative angles are summarized in the table with the p values, showing their statistical significance (Table 1). Hallux valgus angles, intermetatarsal angles, 1st and 5th metatarsal head widths and maximum distance between 1st and 5th metatarsals had all significantly decreased post-operatively (p<0.05). Although DMAA had improved post-operatively, these changes were not statistically significant. All the patients were asymptomatic at their follow up visits at 6 and at 48 months.
Angles |
Pre-operative (degrees) |
Post-operative (degrees) |
P-value |
HVA |
28.17 Range (20-40) |
16.33 Range (4-30) |
(p<0.05) |
IMA 1-2 |
14 Range (9-20) |
9.29 Range (4-14) |
(p<0.05) |
DMAA |
12.58 Range (5-21) |
9.83 Range (1-30) |
(p>0.05) |
IMA 4-5 |
11.35 Range (9-14) |
8.17 Range (4-10.5) |
(p<0.05) |
Width of 1st MT head |
2.27 cm |
1.87 cm |
(p<0.05) |
Width of 5th MT head |
1.27 cm |
1.09 cm |
(p<0.05) |
Distance between 1st and 5th MT Heads |
8.05 cm Range (7.4-9.1) |
7.15 cm Range (6.8-7.7) |
(p<0.05) |
Table 1 Pre-operative and post-operative angle values with statistical significance
When addressing the deformities in splay foot, one must examine each deformity separately. The hallux valgus deformity may result from a variety of contributing factors. The biomechanical etiology of hallux valgus can have its origin in the rear foot. The sequence of events usually commences when the calcaneus everts beyond the vertical in an excessively pronated foot. At the same time, the soft tissue musculature positions around the rear foot and first ray become altered in the pronated foot. With the advent of biomechanics and a more detailed radiographic evaluation of the deformity, the etiology in hallux valgus deformity has become more refined and may be categorized as follows: Hypermobility of the first ray, instability of the midtarsal joint, calcaneal eversion beyond vertical, instability of the peroneus longus.3 The hallux valgus angle is formed by the intersection of a line drawn through the long axis of the first metatarsal and the long axis of the proximal phalanx. A normal hallux valgus angle is one that measures less than 16°. Mild deformity is present when this angle measures between 17° and 25°. A subluxed joint is usually apparent when this relationship measures more than 35°.4 Distal metatarsal osteotomies are frequently used to correct hallux valgus deformity in adults.5 The common procedures to treat hallux valgus deformity (Mitchell, McBride, and Chevron) are effective in correcting most of the deformity. Both the technique and the results of Chevron osteotomy procedure have been reviewed extensively.4,6,7 A V-shaped distal metatarsal osteotomy is used for the correction of mild to moderate hallux valgus.8
Tailor's bunion may present as a hypertrophy of soft tissue overlying the fifth metatarsal; commonly, tailors, sitting with their legs crossed, put pressure on the outer borders of their feet, causing a hypertrophic skin callosity over the fifth metatarsal head.9 Other presentations include a congenitally enlarged or dumbbell-shaped fifth metatarsal head, an abnormal lateral angulation of the fifth metatarsal shaft, or a combination of these conditions. The most commonly used measurements in evaluation of Tailor's bunions include the fourth-fifth intermetatarsal and the lateral deviation angles. Another measure of deviation is the fifth metatarsophalangeal angle, which indicates the magnitude of medial deviation of the fifth toe in relation to the axis of the fifth metatarsal shaft. Also the diameter of the 5th metatarsal head is measured for assessment of Tailor's bunion. Tailor's Bunion management involves identifying the cause, thorough clinical and radiographic evaluation of the deformity, and deciding the best surgical procedure to obtain optimal results.9 No state-of-the-art procedure can be presented for the correction of this fifth ray deformity.10 Treatment of a Tailor's bunion is usually conservative. Surgery is indicated when non-operative treatment can no longer control symptoms. The aim of surgery is to decrease the width of the foot and the prominence of the lateral eminence. Numerous osteotomies have been described to treat this condition; most of the distal osteotomies were originally described for hallux valgus but then later incorporated for the tailor's bunion. The chevron osteotomy is technically demanding when employed for a Tailor's bunion because of the small bony contact area. It is a useful procedure that not only narrows the forefoot slightly to relieve lateral pressure, but can also reduce plantar pressures in the presence of a symptomatic plantar callus.9
There is very little in the English literature about combined 1st and 5th osteotomies for splayfoot deformity and the outcome measures. This study is the first that has looked at the radiological outcome of this procedure and we have had very good and encouraging results so far. Our post operative radiological outcome measures show statistically significant improvement in nearly all the parameters measured. In our study, none of our patients were symptomatic during the follow up assessment, but this was not formally assessed using a scoring system or a patient satisfaction questionnaire. As the outcomes we have shown following the combined osteotomy procedures are good, surgeons should evaluate and consider the 5th metatarsal osteotomy with the 1st metatarsal osteotomy when indicated. These considerations would be to routinely evaluate the 4th and 5th inter-metatarsal angles and the 5th metatarsal head width and if abnormal, to then consider the combined osteotomy procedure.
Our study does have its limitations as we need more patients with longer follow up. We only looked at radiological outcome and we need to further correlate our results with patient satisfaction questionnaires and scoring outcome measures. The early radiological outcome results are encouraging and it demonstrates that simultaneous osteotomy for the splay foot is a pertinent technique.
None.
The author declares that there is no conflict of interest.

©2014 Attar. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.