MOJ
eISSN: 2641-9297


Research Article Volume 1 Issue 4
1Department of Pediatric Pulmonologist, Lakeside Centre for Health Promotion / Lakeside Education Trust, India
2Department of Physician, Lakeside Centre for Health Promotion / Lakeside Education Trust, India
Correspondence: Paramesh H, Department of Pediatric Pulmonologist, Environmentalist, Lakeside Centre for Health Promotion / Lakeside Education Trust, Bangalore, India
Received: May 28, 2018 | Published: July 6, 2018
Citation: Paramesh H, Paramesh RC. Overview in the management of persistent cough in paediatric practice. MOJ Curr Res & Rev. 2018;1(4):154-157. DOI: 10.15406/mojcrr.2018.01.00024
Persistent (Chronic) cough is a major psychosocial economic health burden showing increased prevalence in the past18 years from 8% to 21.25% between 1999 to 2017.1–3 We aimed at highlighting the burden on society and effecting the quality of life. We prepared recommendations based on expert opinion using few parameters like
We kept social determinants, public education and cost containment in mind while preparing the recommendations.1
Keywords: chronic cough, cough medicines, environment cough, allergic cough
Cough is a protective reflex reaction to mechanical, inflammatory or chemical irritation of respiratory tract and a social signal as well. Cough receptors also present in nose, paranasal sinuses external ear, parental plural, oesophagus, stomach, diaphragm, and pericardium. Normally one can expect cough 10-11 episode per day and it can range up to 34 times. Most of them are dry cough which does not disturb sleep. After a bout of viral upper respiratory infection (URI) the cough receptors are hypersensitive for 21 days where innocuous stimulus can trigger cough which reaches its peak in 10days and later reducing to baseline by 21 days where only noxious stimuli will trigger cough.1
When do we call persistent cough?
The classification of cough as persistent (Chronic) is based on duration of symptoms and varies in different countries, between 2 weeks to 8 weeks. For example it is 8 weeks for British thoracic society, 4 weeks for American College of Chest physicians, Australia and New Zealand, 3 weeks in Belgium, 2 weeks for American academy of allergy asthma and immunology, Indian academy of paediatrics, Paediatric association of India and Nation tuberculosis association India. We considered any cough more than 2 weeks duration as persistent (Chronic Cough).
What is the burden of Persistent Cough? 1
Persistent cough has a great impact on psycho-socio-economic burden on child and health care providers as shown in Table 1
The prevalence of persistent cough is observed 8% in 1999 and increased to 21.25% in 2017 in 18yrs.
Traffic police personnel suffer more than non-traffic police personnel 27% to 14.7% respectively
How to evaluate?
Detail clinical history and examination is paramount importance in the evaluation which includes evaluation of symptoms and signs suggestive of underlying respiratory or systemic diseases for specific pointers. The following pointers like type of cough, (dry or wet), type of sputum, timing of cough, onset and progression family history, socio environmental history and ask question for comorbidities like – snoring, mouth breathing, hyperhyidrosis, grinding of teeth (bruxism) and relation to emotional stress like crying, laughing, shouting and physical exercise. Where it tickles before coughing. What medicine he is taking. Feeling of tickling sensation for cough at glottic and supra glottic area is mainly from upper airway pathology and infraglottic and supra sternal area is mainly from lower airway pathology. The physical examination should be thorough from head to toe. For early clubbing, ear, nose throat, neck, chest, and growth pattern. If there are any red flag signs we can subject the patient for investigation as listed in Table 2.
How to evaluate?
The algorithm will guide when to investigate and what are the usual investigations and special investigation is our area Figure 1. Only 8% of the children needed special specific investigations.
The causes of persistent cough
In our study it was Lower airway allergy, asthma in 1999 but it is allergic rhinisinsities (ARS) in 2017.3,4 the details are shown in Table 3. I need to mention about psychogenic cough (somatic cough) the prevalence somatic cough was 1.05% in 1999 and it has increased to 2.8% in 2017 in our practice. The American College of Chest physicians CHEST-2015.5 Recommended that the word psychogenic coughs should be changed to somatic cough from July 2018. The new terms somatic (psychogenic), Tic (Habit) cough we do accept while keeping the time tested clinical clues in the diagnosis. The Tussiphonography shows specific single diamond with absent second diamond as reflects with other cough is shown in Figure 2 & Figure 3 clinically suspect and give supportive, behaviour modification before submitting for detail investigation for cost containment. We believe evidence based medicine is always a complimentary to experience and expertise. Art of practice of medicine cannot be replaced by alter of technology.
Does Children need cough suppressents? If so what to use
Most of the expert panel guidelines recommend not being use cough suppressants, especially in wet cough, the central antitussives are recommended only in early onset pertussis, in hemoptysis, post-surgery, dry cough with sleep disturbance, painful cough. Time has come to change our opinion to suit the burden and comorbidities involving persistent cough. This helps minimise the sleep disturbance and discomfort in the child. If child sleeps, parents can rest, grand parents can relax and primary physician can put at ease. So cough suppressants are needed while waiting for the diagnosis just like using antipyretics in febrile illness.
The pertinent choice of antitussives available 1
The most promising peripheral antitussive drug is Levodropropizine a levoisomer of Dropopazine. It is a non-opioid antitussive, works at C fibre receptors on the surface of the epithelium, inhibits the release of neuropeptides and reduces the intensity frequency and night awakenings
Please note recently some anaphylactic reaction is observed for levodropropzine in Korea.6
Non Pharmacological recommendation are1
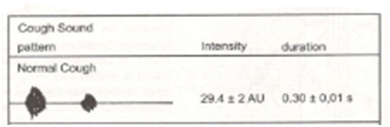
Figure 2 Tussiphonography of normal cough showing 1st diamond for opening of the glottis and 2nd diamond closing of the glottis.
Impact on Child |
Parents |
Insomnia |
Frustration |
Exhaustion |
Sleepless nigh |
School absenteeism |
Upset |
Nausen vomiting |
Stress |
Rectal prolapse |
Helplessness |
Faecal soiling |
Feeling sorry |
Sub conjunctive haemorrhage |
Frequent visit to doctors |
Hernia |
Financial burden |
Cerebral hypoxic encephalopathy |
Quality of life |
Cough syncope |
|
Quality of life |
|
Table 1 Health care provider
Neonatal onset cough |
Wet cough with focal signs in chest |
Family history lung disease |
Clubbing |
Sudden onset of cough |
Abnormal voice or crying |
Hemoptysis |
Stridor |
Cough while feeding with dysphagia and vomiting |
Wheeze |
Night sweats |
|
Poor weight gain |
|
Table 2 Red flag signs for investigation
1999(no: 381) |
2017(no:153) |
||
Astama |
79.21% |
Astama |
45.28% |
ARS |
10.52% |
ARS |
70.25% |
Pneumonia |
2.09% |
Asthama+ARS |
12.27% |
Pertussis Syndrome |
2.09% |
Pertussis Syndrome |
2.80% |
Bronchiectesis |
1.05% |
Bronchiectesis |
2.80% |
Stomach cough(Psychogenic) |
1.05% |
Stomach cough(Psychogenic) |
2.80% |
Foreign body |
0.53% |
PBB |
0.65% |
Hyper-eosinophilic Pulmonary |
0.26% |
|
|
Syndrome Bronchogenic Ca |
0.26% |
|
|
Impacted cerumen |
0.26% |
|
|
Tuberculosis |
0.26% |
|
|
Author declares that there is no conflict of interest.

©2018 Paramesh, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.