MOJ
eISSN: 2574-9722


Case Report Volume 9 Issue 4
1Department of General Surgery, King Fahad General Hospital, Jeddah, Consultant in General Surgery and Intensive Care Unit, Saudi Arabia
2Department of General Surgery, King Fahad General Hospital, Jeddah, Consultant in General Surgery, Saudi Arabia
3Department of General Surgery, King Fahad General Hospital, Jeddah, Consultant in General Surgery and Hepatobiliary, Saudi Arabia
Correspondence: Christian Janikow, Department of General Surgery, King Fahad General Hospital, Jeddah, and Consultant in General Surgery and Intensive Care Unit, Saudi Arabia
Received: December 20, 2024 | Published: December 31, 2024
Citation: AlIkhwan M, Chapra S, Janikow C. Primary retroperitoneal mucinous cystadenoma: laparoscopic resection and literature update. MOJ Biol Med. 2024;9(4):143‒144. DOI: 10.15406/mojbm.2024.09.00231
Primary retroperitoneal mucinous cystadenoma (PRMC) is a rare pathology. Until our last update literature review there is 49 cases published. We present the case number 50 to the scientific literature. A 42-years-old female that presented to our clinic with abdominal pain was diagnosed as retroperitoneal cystic lesion by computed tomography scan. She underwent laparoscopic resection with no complications. The histopathology reveled a PRMC with no malignancy futures. These rare cystic lesions should be included as differential diagnosis at the preoperative stage. The best management option is the complete surgical excision with no intraoperative spillage.
Keywords: primary retroperitoneal mucinous cystadenoma, retroperitoneum neoplasm, laparoscopic resection
Between 1980 and 2017 there was 37 cases reported in the literature of Primary Retroperitoneal Mucinous Cystadenoma (PRMC).1 Until December 19, 2024, there were 49 cases of PRMC published.2 The natural history of this rare entity is known to start as a benign tumor, going through a borderline malignant neoplasm and ending in a cystadenocarcinoma.3 This extremely rare pathology, usually presented in females with unclear preoperative manifestations and challenging diagnosis with a few numbers of reported cases,4 makes it interesting for the scientific community. We report the case number 50 of benign PRMC diagnosed in a 43-year-old woman, which was treated by laparoscopic excision.
A 43-year-old Caucasian female with past medical history of Diabetes treated with oral medication. Gynecologic history of 5 deliveries with no complications, last one 6 months prior to the consultation. She presented to our clinic with a chief complain of left upper abdominal quadrant pain, moderate and intermittent that started around 2 years and worsened during her last pregnancy. Initial examination revealed mild tenderness at the left upper quadrant and flank, palpable mass that was round with smooth surface, slightly compressible, fixed after deep inspiration and expiration without following respiratory movements (Minkowsky sign: negative). An abdominal contrast-enhanced computed tomography scan showed at the left flank a large retroperitoneal rounded unilocular cystic lesion with thin enhancing walls, measuring 8.5 x 7.4 x 10.2 cm, abutting and displacing the descending colon anteriorly and displacing medially the left kidney, no internal septations, calcification or fat-soft tissue on its interior (Figure 1).
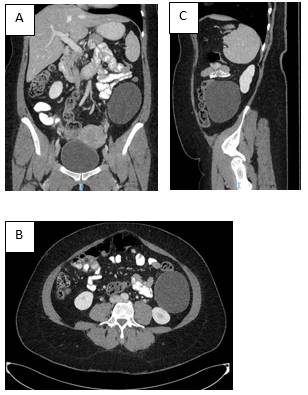
Figure 1 A) Contrast-enhanced computed tomography scan of the abdomen in the coronal plane shows a left retroperitoneal cystic lesion.
B) Contrast-enhanced computed tomography scan of the abdomen in the sagittal plane showing the cystic lesion with no communication to the kidney.
C) Contrast-enhanced computed tomography scan of the abdomen in the axial plane showing the cystic lesion displacing the colon.a .
Her laboratory work up was normal except slight elevation of Hba1C (6.4%). She underwent laparoscopic resection of the cystic lesion without intraoperative complications (Figure 2). Position of the patient was supine with her left side elevated up to 30 degrees. Three ports were placed, one 11mm and two 5mm in size, the left colon was mobilized to medial, and the mass was exposed and detached from the retroperitoneum wall without opening the cyst. The specimen was removed with a bag through and Pfannenstiel incision and analyzed by histopathology. Histopathology reported a PRMC with no futures of malignancy. The patient had a smooth recovery and was discharged 24hs after procedure. The 6 months follow up showed no recurrence of the lesion.
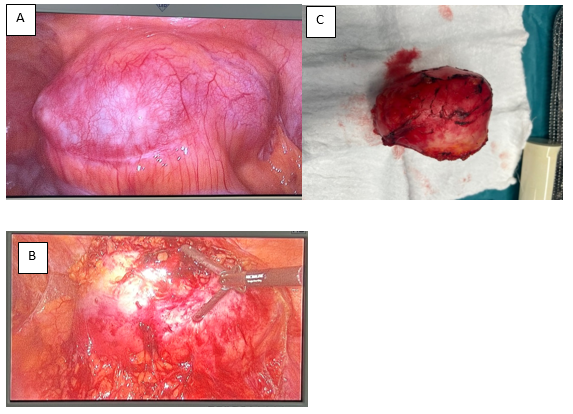
Figure 2 A) Laparoscopic excision, left flank with colon displaced to medial and mass rising from retroperitoneum.
B) Laparoscopic excision, dissection of attachments from the cystic mass.
C) Laparoscopic excision, specimen removed intact.
Cystic lesions in the retroperitoneum can be classified into neoplastic cyst and nonneoplastic cyst. The first group includes cystic lymphangioma, cystic cystadenoma, cystic mesothelioma, cystic teratoma, epidermoid cyst, Müllerian cyst, bronchogenic cyst, tailgut cyst, pseudomyxoma retroperinonei, cystic changes in solid neoplasms, and perianal mucinous carcinoma. Nonneoplastic cyst includes pancreatic pseudocyst, nonpancreatic pseudocyst, lymphocele, urinoma, and hematoma.5 Retroperitoneum mucinous cystic lesions can be considered as a spectrum of lesion starting from benign cystadenoma characterized by large, single, or multiple cysts that can transform in to focus of proliferative columnar epithelium with atypia without invading the lamina mucosae, these types of cystadenomas are borderline tumors with potential into cancer transformation. The last stage of the spectrum is the cystadenocarcinoma with clear malignant transformation and metastatic power.6
Clinically PRMC doesn’t develop specific symptoms, they are more common in woman with a median age of 42.4. Only 4 cases were reported in males.7 The most frequent symptoms include abdominal pain, abdominal distention and palpable mass. The images can clearly define the retroperitoneal location of a cystic lesion but there is no clear radiological sign for its diagnosis. Tumor markers and cytologic analysis can’t clarify the etiology of most of these cystic lesions. Postoperative histological analysis ends leading the diagnosis. It's unclear the origin of these PRMC, they are thought to originate from ovarian tissue due to the similitude to ovarian mucinous cyst adenomas, but immunohistochemical of histological samples shows negative estrogen and progesterone receptors what leads into a second theory of its origin, these is that they may rise from an invagination of the peritoneal mesothelium causing entrapment, mucinous metaplasia and cystic transformation.8
PRMC is more frequent in females and there is no specific clinical futures or images signs to arrive a preoperative diagnosis. It should be considered as differential diagnosis in any retroperitoneum cystic lesion. The surgical excision without spillage of its content should be the gold standard because the final diagnosis of malignancy or not will be with the histopathological sample.
I hereby confirm that we have obtained written, informed consent from the patient for using her clinical findings for publication purpose as case report. Ethical approval was obtained under registration number KACST: KSA: H-02-J-002, IRB approval number: A01952.
None.
The authors declare that there are no conflicts of interest.

©2024 AlIkhwan, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.