MOJ
eISSN: 2574-9722


Research Article Volume 1 Issue 3
1Department of Medical Laboratory Science, University of Nigeria, Nigeria
2Department of Health Services, University of Benin, Nigeria
Correspondence: Nosa Terry Omorodion, Department of Health Services, University of Benin, Nigeria, Tel 081 3674 2270
Received: June 15, 2017 | Published: June 29, 2017
Citation: Asimiyu OS, Achukwu PU, Omorodion NT, et al. Expression of Er, Pr, Ki-67and Her-2 in breast cancer diagnosis using archival tissue block from Olabisi Onabanjo teaching hospital Shagamu and institute of advance medical research training Ibadan. MOJ Biol Med. 2017;1(3):82–86. DOI: 10.15406/mojbm.2017.01.00017
Immunohisto chemistry is used to characterize various surface and intracellular proteins from cells of all tissues. Individual markers and more often panels of various marker proteins can be used to distinguish carcinoma from sarcoma or lymphoma, mesothelioma or melanoma, characterize various tumor subtypes, confirm tissue of origin, help distinguish metastatic from primary tumor and provide additional information about tumors, which may be important for staging, prognosis, predicting response to therapy or evaluating for residual tumor post treatment. The most common panel is one used for breast cancer patients to determine hormone receptor expression and other markers that predict response to certain therapies and determine risk of recurrence to assist in treatment decisions such as surgery, radiation therapy and chemotherapy. Common breast cancer prognostic and therapeutic markers used include: ER, HER2, Ki-67 and PR. Aim of the study is to demonstrate immunohistochemistry markers on samples. Objective: To confirm the superiority of IHC over conventional H$E. The trend shows that 58.5% of the patients were HER-2 and Ki-67 negative. This is an indication that there is likelihood for the patient to survive through effective treatment. The analysis indicated that 1(2.4%) patients were (ER, PR) positive and Ki-67 negative. It also shows that 10(24.3%) patients were (ER, PR) negative and Ki-67 positive. Findings also show that 2(4.9%) patients were (ER, PR) positive and Ki-67 positive. Finally, it shows that 19(46.3%) patients were (ER, PR) negative and Ki-67 negative.
Keywords: immunohisto chemistry, carcinoma, metastasis, therapeutic markers, colloid
Immunohistochemistry is used to characterize various surface and intracellular proteins from cells of all tissues. Individual markers and more often panels of various marker proteins can be used to distinguish carcinoma from sarcoma or lymphoma, mesothelioma or melanoma, characterize various tumor subtypes, confirm tissue of origin, help distinguish metastatic from primary tumor and provide additional information about tumors, which may be important for staging, prognosis, predicting response to therapy or evaluating for residual tumor post treatment.1,2 The most common panel is one used for breast cancer patients to determine hormone receptor expression and other markers that predict response to certain therapies and determine risk of recurrence to assist in treatment decisions such as surgery, radiation therapy and chemotherapy. Common breast cancer prognostic and therapeutic markers used include: ER, HER2, Ki-67 and PR.2 Aim of the study is to demonstrate immunohistochemistry markers on samples. Objective: To confirm the superiority of IHC over conventional H$E. Common breast cancer prognostic and therapeutic markers used include: ER HER2 Ki-67 PR.2 The antibody-defined markers in breast cancer can be employed in two different ways: as prognostic markers (those that can independently forecast clinical outcome) and as predictive markers (those that can independently predict response to a particular therapy).Estrogen and progesterone receptors are weak prognostic markers of outcome and strong predictive markers of response to endocrine, for example, tamoxifen-based, therapy, and are the only immunohistochemistry (IHC)-based breast markers to have received the imprimatur of a consensus committee of the College of American Pathologists.3,4 Estrogen receptors (ERs) expression has long been considered to be present in two-thirds of breast cancers, but more recent studies suggest that its incidence may be closer to 70%. ER status is strongly influenced by tumor grade and histology; as demonstrated by in a study of almost 6000 tumors, virtually all grade I tumors are ER positive, as are pure tubular, colloid, and classic lobular carcinoma.5 As with all IHC studies of therapeutic targets, accurate and perhaps quantitative analysis of the results are critical. There are several major factors that can dramatically affect the apparent ER and PR status of a breast cancer as determined by IHC, including tissue fixation, choice of anti-ER or anti-PR antibody, and determination of thresholds for reporting positive results (Allen M Gown). There is wide variation in the reporting of results of estrogen and PR status, and all of these factors contribute to this. The human epidermal receptor protein-2 (c-erbB-2; HER2) oncogene protein is a transmembrane glycoprotein in the epidermal growth factor receptor family. It is expressed at low levels in a variety of normal epithelia, including breast duct epithelium, but amplification of the HER2 gene and concomitant protein overexpression are present in 10–20% of primary breast cancers determination of HER2 status in breast cancer is important, as it has been determined that it is a prognostic as well as a predictive marker (Allen M Gown). HER2 overexpression and/or gene amplification is an independent prognostic marker of clinical outcome, in both node-negative and node-positive patients. The major utility of HER2, however, is as a predictive marker Breast.6 As a predictive marker, HER2 status has been shown to predict sensitivity to anthracycline-based chemotherapy regimens. In addition, amplification of the HER2 gene and/or overexpression of the HER2 protein confer relative resistance to cytoxan-based regimens and tamoxifen-based therapies in the setting of ER-positive breast cancers. Perhaps most importantly, breast cancers with HER2 alterations are targets for treatment with trastuzumab, a humanized monoclonal antibody, which has been shown to markedly improve response rate and survival when added to chemotherapy or used as a monotherapy.7 Recent studies have demonstrated that adjuvant trastuzumab can reduce the risk of recurrence by one half, and mortality rate by one third, in early-stage breast cancer patients. Other agents, targeting the HER2 gene product, have also demonstrated clinical utility, and several more are in development. Trastuzumab is one of the first successful therapies that have been custom-designed to identify a tumor-associated molecule. This work is aim at demonstrate relationship between KI-67 and other markers in breast cancer to confirm diagnosis and occurrence.8
Total number of 46 archival tissue blocks of breast cancer patients was collected and each block was sectioned in duplicate for staining (haematoxylin and eosin staining techniques) and immunohistochemical technique to express estrogen receptor, prosterone receptors, human epidermal 2(HER-2) and KI -67. Rotary microtome was used to cut the serial sections of 5 microns each. Then, the section was put in 20% alcohol on a slide before being transferred to the water bath. This made the section to be spread properly without any folding while anther slide was used to pick the section by placing it vertically into the water in the water bath. It was placed on the hot plate in order to remove wax and to fix the section onto the slide. Now the sections were arranged, and they are now ready for staining. Haematoxylin and eosin staining techniques was used to stain the section, in order to achieve good nuclei and cytoplasm staining section. Haematoxylin was dissolved in the alcohol before the addition of the other constituent. The stain was ripened by addition of Sodium iodate. The haematoxylin solution turned reddish violet in colouur, is ready for immediate use. Procedure of staining Dewaxed and Hydrated, in solution 1 for 10 to20minutes, Wash thoroughly in running tap water, Deffrentiated in solution 2 until only the cell nucleus retained the stain, Blue in running tap water for 5-10minute, Counter stained in solutions 4 for 1 to 2minutes, Washed in running water excess eosin is removed, Dehydrated in ascend ing grade of alcohol. Clear in two changes of xylene Mount in DPX Results: nuclei: blue, connective tissue and cytoplasm show pink. Immunohistochemical procedure include; Deparaffinize slides and hydrate to distilled water, Block endogenous peroxidase activity in hydrogen peroxide methanol solution for 30minutes, Rinse in 2 changes of distilled water, 1 minute each, Place in phosphate- buffered saline solution, Optional: Digest slides in freshly prepared trypsin solution at 37oc for 3 to 10minutes, Rinse well with phosphate- buffered solution, Place in normal serum from the same spacies in which the bridge antibody is produced for 30minutes; drain, but do not rinse the slides, Place in primary anti body for 30minutes, Rinse well with phosphate-bufferred saline solution, Place in secondary antibody for 30minutes, Rinse well with phosphate-bufferred saline solution, Place in peroxidise antiperoxidise (PAP) complex solution for 30minutes, Rinse well with phosphate-bufferred saline solution, Place in diaminobenzidine (DAB) substrate solution, followed by a rinse with distilled water, Counterstain with Mayer`s haematoxylin solution 5 minutes.Wash in tepid water for ten minutes.Dehydrate and clear through 95% ethyl alcohol, absolute ethyl alcohol, and xylene, 2 changes each for 2minutes each. Mount with resinous medium.9
Frequency count: (Tables 1-13) and (Graphs 1-7).
Estrogen Receptor (ER) |
|||||
Valid |
Frequency |
Percent |
Valid Percent |
Cumulative Percent |
|
negative |
38 |
92.7 |
92.7 |
92.7 |
|
positive |
3 |
7.3 |
7.3 |
100 |
|
Total |
41 |
100 |
100 |
||
Table 1 Frequency count.
The result indicated that 38(92.7%) of the cancer patients were ER negative while the remaining 3(7.3%) were positive with mean and standard deviation 1.07±0.264.
Progesterone Receptor (PR) |
|||||
Valid |
Frequency |
Percent |
Valid Percent |
Cumulative Percent |
|
negative |
36 |
87.8 |
87.8 |
87.8 |
|
positive |
5 |
12.2 |
12.2 |
100 |
|
Total |
41 |
100 |
100 |
||
Table 2 The result indicated that 36(87.8%) of the cancer patients were PR negative while the remaining 5(12.2%) were PR positive with mean and standard deviation 1.12±0.331.
Human Epidermal 2 Receptor (HER-2) |
|||||
Valid |
Frequency |
Percent |
Valid Percent |
Cumulative Percent |
|
negative |
32 |
78 |
78 |
78 |
|
positive |
9 |
22 |
22 |
100 |
|
Total |
41 |
100 |
100 |
||
Table 3 The result indicated that 32(78.0%) of the cancer patients were HER-2 negative while the remaining 9(22.0%) were HER-2 positive with mean and standard deviation 1.22±0.419.
Ki67 |
|||||
Valid |
Frequency |
Percent |
Valid Percent |
Cumulative Percent |
|
negative |
29 |
70.7 |
70.7 |
70.7 |
|
positive |
12 |
29.3 |
29.3 |
100 |
|
Total |
41 |
100 |
100 |
||
Table 4 The result indicated that 29(70.7%) of the cancer patients were Ki67 negative while the remaining 12(29.3%) were Ki67 positive with mean and standard deviation 1.29±0.461.
Crosstab |
||||
Count |
||||
Ki67 |
Estrogen Receptor (ER) |
Total |
||
negative |
positive |
|||
Negative |
28 |
1 |
29 |
|
Positive |
10 |
2 |
12 |
|
Total |
38 |
3 |
41 |
|
Table 5 Comparison of the Markers.
The result indicated that 29(70.7%) of the cancer patients were Ki67 negative while the remaining 12(29.3%) were Ki67 positive with mean and standard deviation 1.29±0.461.
Variables |
ER |
χ2 |
p-value |
|
Ki67 |
Negative |
Positive |
||
Negative |
2.187 |
0.139 |
||
Positive |
28(68.3%) |
1(2.4%) |
||
10(24.4%) |
2(4.9%) |
|||
Table 6 Chi-square analysis.
The analysis indicated that 28 cancer patients were Ki67 negative while 28 were ER negative. It also showed that 10 cancer patients were Ki67 positive while 28 were ER negative. It also shows that 10 cancer patients were Ki67 positive while only 2 were ER positive. The result also shows that 28 cancer patients were Ki67 negative while just 1 was ER positive. Finally, it indicated that 4 patients were Ki67 and ER positive respectively.
Crosstab |
||||
Count |
||||
Progesterone Receptor (PR) |
Total |
|||
negative |
positive |
|||
Ki67 |
negative |
26 |
3 |
29 |
positive |
10 |
2 |
12 |
|
Total |
36 |
5 |
41 |
|
Table 7 The analysis indicated that 28 cancer patients were Ki67 negative while 28 were ER negative. It also showed that 10 cancer patients were Ki67 positive while 28 were ER negative. It also shows that 10 cancer patients were Ki67 positive while only 2 were ER positive. The result also shows that 28 cancer patients were Ki67 negative while just 1 was ER positive. Finally, it indicated that 4 patients were Ki67 and ER positive respectively.
Variables |
ER |
|
p-value |
|
Ki-67 |
Negative |
Positive |
||
Negative |
0.317 |
0.574 |
||
Positive |
26(63.4%) |
3(7.3%) |
||
10(24.4%) |
2(4.9%) |
Table 8 The Chi-square result indicated that the relationship between Ki67 and ER is not statistically significant at p≥0.05. This implies that they are independent, which means that for ER to be positive does not directly imply that Ki67 to be positive or vise-verse.
Statistics |
||
Markers |
||
N |
Valid |
41 |
Missing |
0 |
|
Mean |
2.83 |
|
Std. Deviation |
1.843 |
|
Table 9 Statistics.
The analysis indicated that 26 cancer patients were Ki67 negative while 26 were PR negative. 26 patients were Ki67 negative while 3 were PR positive. It also shows that 10 patients were Ki67 positive while only 2 were PR positive. The result also shows that 10 patients were Ki-67 positive while 26 were ER negative. Finally, it indicated that 2 patients were Ki67 and PR positive respectively.
Markers |
|||||
Frequency |
Percent |
Valid Percent |
Cumulative Percent |
||
Valid |
All negative |
19 |
46.3 |
46.3 |
46.3 |
All positive |
1 |
2.4 |
2.4 |
48.8 |
|
1 negative, 3 positives |
3 |
7.3 |
7.3 |
56.1 |
|
2 negatives, 2 positives |
4 |
9.8 |
9.8 |
65.9 |
|
3 negatives, 1 positive |
14 |
34.1 |
34.1 |
100 |
|
Total |
41 |
100 |
100 |
||
Table 10 The Chi-square result indicated that the relationship between Ki-67 and PR is not statistically significant at p≥0.05. This implies that they are independent, which means that for PR to be positive does not directly imply that Ki-67 to be positive or vice-versa.
Counts |
Variables |
|||
(HER-2, Ki-67) Negative |
(HER-2, Ki-67) Positive |
HER-2 Negative, Ki-67 Positive |
HER-2 Positive, Ki-67 negative |
|
Frequency |
24 |
4 |
8 |
5 |
Percentage |
58.5 |
9.8 |
19.5 |
12.2 |
Table 11 Cross tabulation of her-2 and ki-67.
The analysis indicated that 24(58.5%) patients were HER-2 negative and Ki-67 negative. It also shows that 4(9.8%) patients were HER-2 positive and Ki-67 positive. Findings also show that 8(19.5%) patients were HER-2 negative and Ki-67 positive while 5(12.2%) patients were HER-2 positive and Ki-67 negative.
Counts |
Variables |
||
(ER, PR, HER-2 and Ki-67) Negative |
(ER, PR, HER-2) Negative and Ki-67 Positive |
(ER, PR, HER-2 and Ki-67) Positive |
|
Frequency |
19 |
7 |
1 |
Percentage |
46.3 |
17.1 |
2.4 |
Table 12 Crosstabulation of Er, Pr, Her-2 and Ki-67.
The analysis indicated that 19(46.3%) patients were ER, PR, HER-2 negative (triple negative) and Ki-67 negative. It also shows that 7(17.1%) patients were ER, PR, HER-2 negative and Ki-67 positive. Findings also show that 1(2.4%) patients were ER, PR, HER-2 and Ki-67 positive.
Counts |
Variables |
|||
(ER, PR) Positive & Ki-67 Negative |
(ER, PR) Negative & Ki-67 Positive |
(ER, PR) Positive and Ki-67) Positive |
(ER, PR) and Ki-67) Negative |
|
Frequency |
1 |
10 |
2 |
19 |
Percentage |
2.4 |
24.3 |
4.9 |
46.3 |
Table 13 Cross tabulation of (Er, Pr) and Ki-67.
The analysis indicated that 1(2.4%) patients were (ER, PR) positive and Ki-67 negative. It also shows that 10(24.3%) patients were (ER, PR) negative and Ki-67 positive. Findings also show that 2(4.9%) patients were (ER, PR) positive and Ki-67 positive. Finally, it shows that 19(46.3%) patients were (ER, PR) negative and Ki-67 negative.
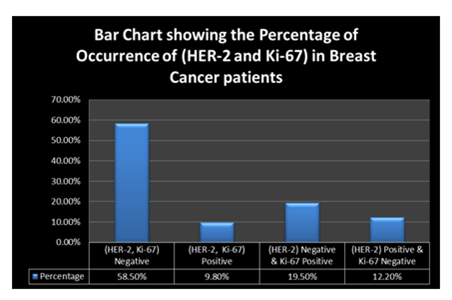
Graph 1 This bar chart shows that 58.5% of the patients were HER-2 and Ki-67 negative. This is an indication that there is likelihood for the patient to survive through effective treatment.
ER, PR, HER-2and Ki-67 has served as a prognostic. The trend shows that 58.5% of the patients were HER-2 and Ki-67 negative. This is an indication that there is likelihood for the patient to survive through effective treatment.
Immunohistochemical techniques and Haemotoxylin and Eosin should be used in the analysis of breast cancer.
None.
The author declares no conflict of interest.

©2017 Asimiyu, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.