Journal of
eISSN: 2379-6359


Research Article Volume 4 Issue 6
1Department of Speech Pathologist and Audiology, Fluminense Federal University, Brazil
2Department of Otorhinolaryngology and Head and Neck Surgery, Maastricht University Medical Center, Netherlands
Correspondence: Lilian Felipe, Department of Speech Pathologist and Audiology, Federal Fluminense University, Health Institute from Nova Friburgo, Doutor Sílvio Henrique Braune, Centro, Nova Friburgo-RJ, Zip code: 28625650, Brazil
Received: June 20, 2016 | Published: November 2, 2016
Citation: Felipe L, Kingma H (2016) Vibrotactile Biofeedback System and Bilateral Vestibular Loss: Pilot Study. J Otolaryngol ENT Res 4(6): 00124. DOI: 10.15406/joentr.2016.04.00124
Bilateral Vestibular Loss (BVL) main complaints are oscillopsy and imbalance. BVL has a strong negative impact on physical function and social interaction, decreasing quality of life. Vestibular Rehabilitation therapy is currently the mainstay in the treatment for these patients. However, rehabilitation therapy has shown to be less effective with patients with bilateral vestibular loss. There is no evidence of an effective treatment for patients with bilateral vestibulopathy. There is a clear need for a therapeutic solution. In this pilot study, subjects with BVL used the Vibrotactile Biofeedback System (VBS). A significant improvement in quality of life of these subjects was observed. Efforts toward the development of VBS were justified. This method could be crucial for some patients’ quality of life.
Keywords: rehabilitation, postural balance, feedback, sensory
BVL, bilateral vestibular loss; VBS, vibrotactile biofeedback system; BVH, bilateral vestibular hypo function; VBF, vibrotactile bio feedback; DHI, dizziness handicap inventory; BA, bilateral areflexia; BH, bilateral hypo function; AH, asymmetric hypo function
Corporal balance is a complex process involving coordinated activities of multiple sensory and motor components mainly from visual, vestibular and proprioceptive systems.1 The vestibular system’s function is to transduce head acceleration to the brain. This information matches with other sensory inputs for gaze stabilization on the retina and posture control. Vestibular disorders can cause posture and movement impairment.2
Bilateral vestibular loss can be extremely disabling and cause significant limitation for daily living activities. The literature shows a variation from 28 to 81 per 100,000 people3 prevalence rates, and the percentage of bilateral loss in patients who underwent electronystagmography varies from 0.6 to 13.6%.4,5 It means the number of persons with vestibular loss is higher then expected by a simple battery test evaluation.
Bilateral Vestibular Hypofunction (BVH) and Bilateral Vestibular Loss (BVL) are characterized by reduced or absent, respectively, function of both vestibular systems,6 causing an impairment or loss of: gaze stabilization, balance maintenance, postural control and spatial orientation.7 Adults with BVL can be dramatically affected by chronic imbalance, oscillopsy (illusory visual field movement during head movements), postural instability and impaired spatial orientation.1,6
Nowadays it represents a functional heterogeneous disorder with combined or isolated deficits of the semicircular canals and/or otolith organs.7 However, etiology still remains unclear in approximately 50% of all cases.8 Vestibular rehabilitation strategies have been applied successfully over the last few decades to initiate central compensation of the tonus imbalance and to facilitate substitution in different types of peripheral vestibular dysfunction.9 While some individuals with residual sensation often compensate through rehabilitation exercises, others who failed treatment have no other proper treatment options.9,10 A potent aid for these patients might be an artificial labyrinth to restore the feedback of linear and angular accelerations of the head or body to the brain. Several researchers are currently engaged with the development of such a device.
Visual, auditory, vibrotactile, and electrotactile feedback have been used to provide real-time feedback of body or head movement during quiet and perturbed stance and some locomotor activities.10‒12 In this pilot study, we tested the Vibrotactile Biofeedback System (VBS) in subjects with severe bilateral vestibular deficit to investigate VBS efficiency for balance activities.
The Vibrotactile Biofeedback (VBF) System (Figure 1) consists of four major components:
One actuator is activated in the direction of a patient’s body tilt if it exceeds a tilt magnitude of 2o. In this way, the VBF system can code body tilt in any direction and the actuator, which is activated above 2o of tilt, indicates the tilt direction. When the subject correctly responds to the actuator, it will be deactivated when the tilt magnitude drops below 1.5o. The range between 1.5o and 2o was chosen to avoid abrupt changes in switching on and off a specific actuator (in other words, hysteresis is induced). Thus, the dead zone has a size of 2o.
When the subject corrects his body tilt back to below 1.5o, all 12 actuators are deactivated. The goal of VBS is to provide additional feedback, enabling user to preserve the balance during everyday tasks. In another view, the VBS (Figure 2) consists of a sensor unit, a processor and vibrating elements. The VBS was wrapped tightly around the subject’s torso. The actuators were affixed inside the belt around the positions of the navel, spine, and right and left sides of the torso (Figure 3).
The evaluation of the VBS was divided into two parts: Patients with vestibular disorders were selected to participate the test. All patients were selected after ENT evaluation and recommendation. Subjects on wheelchair or with additional neurological deficits were excluded from the study. Study protocol was approved by the Hospital Ethics Committee and informed consent was signed by all subjects, followed by clinical ENT examination and a complete and thorough neuro-otological and vestibular examination at Balance Disorders Laboratory-Maastricht University. In addition, the Dizziness Handicap Inventory (DHI) was added to test protocol. In order to be included in this study, subjects should have DHI scores higher than 60.
Part 1
For the first section of this experiment, the Vibrotactile Biofeedback System was tested on subjects with diverse vestibular diagnosis. The main idea was to verify which group could be more favorable and show positive results. Each subject could test the VBS at the hospital area during three hours.
Part 2
For the second section, only subjects with BVL and BVH were selected. They could use VBS for a period of three weeks for daily activities. After the test with the VBS, all subjects answered a simple questionnaire about different situations: sitting, standing and walking and the impact of VBS in general quality of life. It was possible to verify in each question how much (from 0% to 100%), could VBS contribute for balance improvement.
Part 1
Twelve patients (five women and seven men) with an average age of 63.3 years (40-75years) were recruited through Maastricht University Vestibular Disorders Laboratory-ENT Department. Subjects with diverse vestibular diagnosis were evaluated. The main thrust was to verify the possibility of having a group which could have more benefits from the VBS. Twelve subjects was evaluated for the first part of the study. 2 subjects (17%) with Bilateral Areflexia (BA), 3 (25%) with Bilateral Hypofunction (BH), 05 (41%) with Asymmetric Hypofunction (AH) and 2 (17%) with Central Vestibular Disorder.
All subjects had three hours to test the VBS. After the test, they answered if they had any balance improvement while using the equipment in different situation: sitting, standing, walking, and also related about general quality of life. The mean percentage of positive gain for each situation versus the vestibular diagnosis was represented on Figure 4. The global score percentage about all questions together was represented on Figure 5.
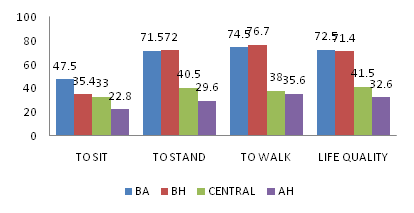
Figure 4 Mean percentage of positive gain from each vestibular pathology group after three hours testing the VBS. Maastricht University, 2015. N=12.
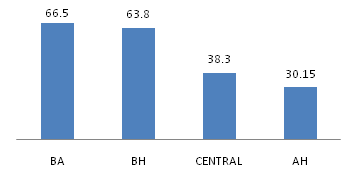
Figure 5 General Mean Percentage Score according groups after three hours testing the VBS. Maastricht University. 2015. N=12.
Statistical analysis presented a significant value difference between bilateral hypofunction and bilateral vestibular loss compared with other groups (p<0.005). The second part consisted of checking balance improvement from both groups with better percentages during three weeks.
Part 2
A previous list of patients from the Maastricht University Vestibular Disorders Laboratory-ENT Department had all subjects with BVH and BVL. From 32 patients selected to test VBS during three weeks, 10 of them were not evaluated for many reasons such as: health problems (3), refusing to go to the hospital because they did not have company (2), absence for the appointment (1) or no reply after the contact (4). Twenty two patients (12 women and 10 men) with an average age of 64years (52-84years) attended after the letter contact. 11 subjects (5 women 6 men) with BVL and 11 BVH (7 women and 4 men) were evaluated. The mean scores (percentage) for each situation according the diagnosis was presented in Figure 6. The global mean score percentage according all the four questions was higher than 85 for both groups, which had almost the same behavior according the statistical analysis (p>0.005).
Subjects with Bilateral Vestibular Loss or Hypofunction perceive lower quality of life when compared to the general population.2,5 They feel limited when carrying out physical activities, working or doing daily living activities.2‒4 Moreover, they have difficulties in social activities as a result of emotional problems such as anxiety and depression.13s
Intensive physical rehabilitation and compensation mechanisms can help some patients to keep balance and posture control. However, the treatment for these patients is difficult and may not be possible in some cases.14 They can keep on showing significant physical impairments, disability, which increases the risk of falling.15 That is because the bilateral vestibular loss disables the vestibule-ocular and vestibule-spinal reflexes that maintain stable gaze and posture.16 Affected individuals experience oscillopsy, chronic imbalance, and postural instability that interfere in daily activities such as walking or driving.4,8,9
The present pilot study results seems to indicate that specific proprioceptive feedback equipment could significantly improve the postural control in the majority of patients with vestibular disorders (all subjects had a positive percentage for all questions from this study). Moreover, the improvement was significantly higher in patients with bilateral vestibular loss or hypofunction (p>0.005). It was also noticed that time of experience using VBS influenced the scores, even at the same group. Subjects with longer time using VBS showed higher scores. Probably, because longer experience could provoke training regimen.17,16
Thus, the perception of dizziness and balance of the patient were improved, as well as in gait and balance measurement results, confirming the effectiveness of VBS and that device could be a sensory substitution. Sensory substitution studies were initiated as models of brain plasticity, which was defined as the adaptive capacity of the central nervous system, and its ability to modify its own structural organization and functioning.18
The results of this study suggest that Vibrotactile Biofeedback System device was able to improve the body balance of patients. Previous studies suggested that the brain could interpret information from a sensory substitution device. With training, the brain learns to appropriately interpret the information from the device and works as it would with normal natural sense.19,20,17 Despite of being conducted with a small number of patients, this study could already show unquestionably the vibrotactile biofeedback as a sensory substitution to the vestibular system and as a useful tool for patients with limitations in postural recovery with conventional vestibular rehabilitation protocols.
These preliminary results demonstrate the Vibrotactile Biofeedback System as an effective way to improve postural stability, especially in vestibular bilateral loss disorders. In our opinion, this device deserves more clinical evaluation and comparative studies.
None.
Author declares there are no conflicts of interest.
None.

©2016 Felipe, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.