Journal of
eISSN: 2379-6359


Research Article Volume 5 Issue 2
1Department of Otolaryngology Menoufia University, Egypt
2Department of Otolaryngology Tanta University, Egypt
3Department of Radiodiagnosis Menoufia University, Egypt
Correspondence: Heba Abdel Rahem Abo El Naga Otolaryngology department Faculty of Medicine Menoufia University Egypt 4 Borsa St Al Saa square Tanta Gharbia, Egypt, Tel 002-0100-7217285
Received: October 29, 2016 | Published: December 21, 2016
Citation: El-Naga HAA, El-Rasheedy AI, Abdelaziz M, Shawky M (2016) The Role of Multidetector CT Virtual Bronchoscopy in Assessment of Patients with Laryngotracheal Stenosis. J Otolaryngol ENT Res 5(2): 00135. DOI: 10.15406/joentr.2016.05.00135
Background: Proper assessment of the site, degree and length of laryngotracheal stenosis is essential for proper selection of the procedure and helps in anticipating future prognosis. Virtual bronchoscopy (VB) is a novel CT-based imaging technique that allows a three-dimensional (3D) evaluation of the airway.
Objective: Is to assess the utility of CT virtual bronchoscopy in assessment of laryngotracheal stenosis.
Patients and methods: A case series study was conducted on 26 patients diagnosed as laryngotracheal stenosis with age more than 3years old. All patients were assessed by history, general examination and routine ear, nose and throat examination. Laryngeal examination was performed using flexible naso-pharyngo-laryngoscopy under local anesthesia. Computed tomography scanning with axial, mutiplanner reconstruction and virtual bronchoscopy images was performed for all patients using multidetector scanners to define the site, grade and length of stenotic segment. All patients were assessed by rigid bronchoscopy under general anesthesia to confirm the results of virtual bronchoscopy regarding site, grade and length of stenotic segment. Sensitivity, specificity and diagnostic accuracy were calculated for virtual bronchoscopy.
Results: The sensitivity, specificity and diagnostic accuracy of virtual bronchoscopy in localizing the site of stenosis were 100% for all. The sensitivity, specificity and diagnostic accuracy of virtual bronchoscopy in grading the stenosis were 85.3%, 94.5% and 92% respectively. The sensitivity, specificity and diagnostic accuracy of virtual bronchoscopy in measuring the length of stenosis were 92.3%, 94.3% and 92% respectively.
Conclusion : CT Virtual endoscopy is a highly accurate method in detection of the presence of laryngotracheal stenosis. However, it needs confirmation by rigid bronchoscopy for measurement of the grade and length of stenosis.
Keywords: laryngotracheal stenosis, virtual bronchoscopy, ct imaging, endotracheal intubation, rigid bronchoscopy, tracheostomy, etiology
VB, virtual bronchoscopy; 3D, three-dimensional; MDCT, multi-detector computed tomography; MPR, multi-planar reconstructions; VE, virtual endoscopy; RB, rigid bronchoscopy; FT, flexible tracheobronchoscopy; IO, intra-operative
The Incidence of laryngotracheal stenosis is increasing nowadays due to increasing incidence of prolonged endotracheal intubations with increasing incidence of polytrauma, neurovascular accidents, and complex surgical procedures with subsequent intensive care units admission, intubation with or without ventilation. Improvement in the protocols of intensive care increased the numbers of patients discharged who then suffer from the development of tracheal stenosis which is an inevitable result of prolonged endotracheal intubation especially with high pressure cuffs.1
Various factors other than prolonged endotracheal intubation are responsible for laryngotracheal stenosis including high tracheostomies, tracheostomy with excessive cartilage removal, infection following tracheostomy, use of improper size of tracheostomy tube and granulomatous diseases of the laryngotracheal tract (like scleroma or Wagner's granulomatosis). Although rare, congenital subglottic stenosis remains an important etiological factor, which needs proper planning and decision-making. Several surgical procedures have been used to treat laryngotracheal stenosis. Choice of procedure depends upon age of patient, site of stenosis, nature of stenosis, etiology and general condition of patient.2
Proper assessment of the site, degree and length of laryngotracheal stenosis is essential for proper selection of the procedure and helps in anticipating future prognosis. Imaging can provide a simple, noninvasive and readily available tool for such assessment. Recent advances in computed tomography technology offered 3D multiplanner reconstruction with the introduction of virtual bronchoscopy as an imaging software with much data. Virtual bronchoscopy (VB) is a novel CT-based imaging technique that allows a three-dimensional (3D) evaluation of the interior and peripheral wall of the airway down to the seventh division of the laryngobronchial trees.3 Such technique can provide generous information regarding cases of laryngotracheal stenosis. The aim of this study is to assess the utility of virtual bronchoscopy in assessment of laryngotracheal stenosis as compared to rigid bronchoscopy as reference.
The current study is a case series study conducted on 26 patients retrieved from the outpatient clinics of Otorhinolaryngology departments of Menoufia and Tanta universities spanning the period from January 2014 to December 2015.
The study included patients diagnosed as laryngotracheal stenosis regardless of the etiology with age more than 3years old. Any patient with hypersensitivity to contrast materials or any cause for unfitness for general anesthesia were excluded from the study.
All the patients were assessed by history taking to define the etiology (inflammatory, traumatic, post intubation) along with onset, course and duration of the disease. General examination was conducted for all patients to exclude any associated comorbidities with contraindication to general anesthesia.
All patients were subjected to routine ear, nose and throat examination to define the etiological factors like scleroma with the common association of nasal manifestations (granulations, atrophic changes or fibrosis) or any other granulomatous diseases. Laryngeal examination was performed using flexible naso-pharyngo-laryngoscopy under local anesthesia for initial assessment of the level, degree of stenosis in the laryngotracheal tract.
CT imaging (Figures 1-3)
Multidetector CT studies were done for patients without sedation using a 16-detector CT scanner (16-multidetector CT scanner, Toshiba Alexion-Japan). Patients were examined in the supine position, head first, with extended head, elevated arms and were scanned from caudal to cranial. Scanning parameters were: slice width, 1.25mm; slice collimation ; 4X1feed-rotation, 4mm; rotation time, 0.5s; pitch, 4; and 80kVp. Acquisition time was roughly 20s to complete the acquisition in single breath-hold. The reconstruction intervals and slice thickness were 2mm. A frontal scout view from the level of the larynx to the dome of the diaphragm was obtained first. A dose of 80-100mL Iohexol (Omnipaque) 300mg iodine/mL was administered at a rate of 3.5mL/s through a 18-gauge IV catheter in the antecubital vein.
Image processing
The axial source images were created, and transferred to a Vitrea Workstation. For each scan, postprocessing images included multiplanar reformations (sagittal and coronal views), three dimensional and virtual bronchoscopy (VB). The latter was placed in the proximal part of the trachea and evaluated using a fly-through mode. Each virtual bronchoscopy image simulated a coned-down view, with a cone angle adjusted to 45. Post processing time ranged between 25 and 35min for each study. All images for each patient were saved as digital files and evaluated together.
Image analysis
All CT studies are reviewed by a radiologist and analysis of axial, multiplanar reformations, and VB images was done. The axial CT images were interpreted first, then the coronal and sagittal reformatted images and finally, virtual bronchoscopy. The axial and multiplanar reformatted images were viewed with standard lung window settings (level, 450H; width, 1850H) and standard soft-tissue window settings (level, 50H; width, 450H). (Figures 1-3) A diagnostic judgment was expressed on any tracheal stenotic segment based on the following parameters:
Site: The method proposed in the current study defines three possible locations within the central airways: laryngeal (mainly subglottic); tracheal (cervical trachea); and multiple sites (laryngeal and tracheal).
Grading: To calculate the grade of stenosis, a program ruler for comparing the diameter of the maximal tracheal luminal narrowing to the diameter of the normal trachea. The Myer-Cotton grading system4 which divided into four grades; grade 1 (luminal narrowing <50%), grade 2 (luminal narrowing >50% but <70%), grade 3 (luminal narrowing >70%) and grade IV, no lumen detected.
Length of stenotic segment: We used the same methods proposed by Kamal et al.,5 who used the program ruler for measuring the maximal projectional length of the tracheal luminal narrowing.
Bronchoscopic assessment
All patients were assessed by rigid bronchoscopy under general anesthesia to confirm the results of virtual bronchoscopy regarding site, grade and length of stenotic segment (Figure 1-D).
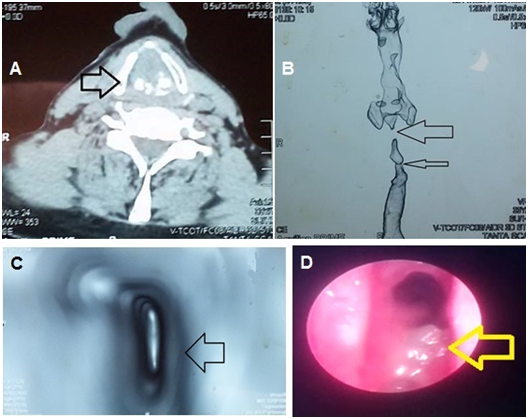
Figure 1 Male patient 45 years old post neck burn: A: High resolution CT neck with contrast/Axial cut showing severe subglottic stenosis. B: 3D reconstruction of the laryngotracheal area showing severe subglottic stenosis. C: Virtual Bronchoscopy image showing subglottic stenosis. D: Bronchoscopic view of the patient showing oedema and secretions of the subglottic area rather than true stenosis.
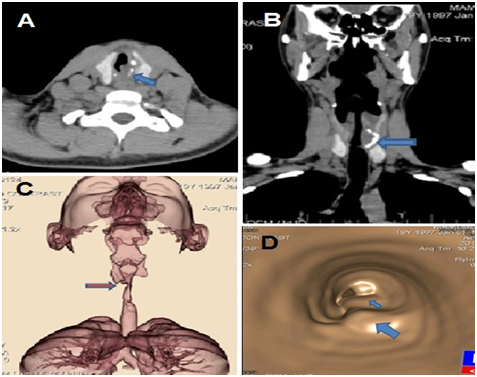
Figure 2 Male patient 24 years old post prolonged intubation: A: High resolution CT neck with contrast/Axial cut showing moderate subglottic stenosis. B: Coronal reconstruction of the laryngotracheal area showing moderate subglottic stenosis. C: 3D reconstruction of the laryngotracheal area showing moderate subglottic stenosis. D: Virtual Bronchoscopy image showing subglottic stenosis.
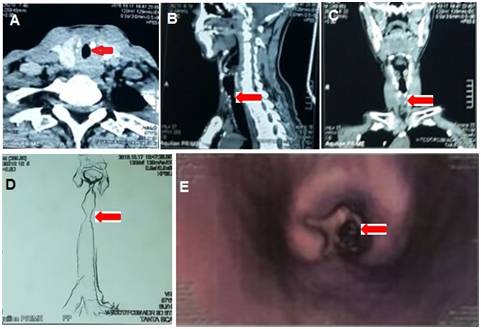
Figure 3 Male patient 54 years old post prolonged intubation: A: High resolution CT neck with contrast/Axial cut showing mild cervical tracheal stenosis. B: Sagittal reconstruction of the laryngotracheal area showing mild cervical tracheal stenosis. C: Coronal reconstruction of the laryngotracheal area showing mild cervical tracheal stenosis. D: 3D reconstruction of the laryngotracheal area showing mild cervical tracheal stenosis. E: Virtual Bronchoscopy image showing cervical tracheal stenosis.
Outcome
The tracheal stenotic segment was analyzed concerning its grade, length, length from the vocal cord and length of planned resection segment as follows:
Statistical analysis
Statistical analyses were performed with SPSS (Statistical Package for Social Science, version 16 Inc., Chicago, IL) program soft ware package for Windows. Sensitivity, Specificity and accuracy for VB for the evaluation of the included stenotic tracheal segments were determined using the intraoperative findings as the gold standard of reference.
The current study included 26 patients diagnosed as laryngotracheal stenosis with mean age 23.2 years ±11.7 SD. The patients included 19 males and 7 females (Table 1). The etiology of stenosis included 5 congenital cases, 12 traumatic and 9 inflammatory cases (Table 2).
Gender |
Congenital |
Traumatic |
Inflammatory |
Total |
|
|||
N=5 |
% |
N=12 |
% |
N=9 |
% |
26 |
% |
|
Male |
4 |
80 |
12 |
100 |
3 |
33.3 |
19 |
73.1 |
Female |
1 |
20 |
0 |
0 |
6 |
66.7 |
7 |
26.9 |
Table 1 Distribution of gender among study patients
Etiology |
No. |
% |
Congenital |
5 |
19.2 |
Traumatic |
12 |
46.2 |
Inflammatory |
9 |
34.6 |
Total |
26 |
100 |
Table 2 Etiology of laryngotracheal stenosis
In the current study, the sensitivity, specificity and diagnostic accuracy of virtual bronchoscopy in localizing the site of stenosis were 100% for all (Table 3). In the current study, the sensitivity, specificity and diagnostic accuracy of virtual bronchoscopy in grading the stenosis were 85.3%, 94.5% and 92% respectively (Table 4).
|
|
Bronchoscope |
|
Total |
Sens |
Spec |
Acc |
|
Laryngeal |
Tracheal |
Multiple |
||||||
VB |
laryngeal |
5 |
0 |
0 |
5 |
100% |
100% |
100% |
Tracheal |
0 |
12 |
0 |
12 |
||||
Multiple |
0 |
0 |
9 |
9 |
||||
Total |
|
5 |
12 |
9 |
26 |
|
|
|
Table 3 Evaluation of site of laryngotracheal stenosis by virtual bronchoscopy compared to rigid bronchoscopy
|
|
Bronchoscope |
|
|
Total |
Sens |
Spec |
Acc |
|
|
Grade 1 |
Grade 2 |
Grade 3 |
Grade 4 |
|
|
|
|
|
VB |
Grade 1 |
3 |
0 |
0 |
0 |
3 |
85.30% |
94.50% |
92% |
Grade 2 |
1 |
8 |
0 |
0 |
9 |
||||
Grade 3 |
0 |
2 |
6 |
0 |
8 |
||||
Grade 4 |
0 |
0 |
1 |
5 |
6 |
||||
Total |
|
4 |
10 |
7 |
5 |
26 |
|
|
|
Table 4 Evaluation of grade of laryngotracheal stenosis by virtual bronchoscopy compared to rigid bronchoscopy
In the current study, the sensitivity, specificity and diagnostic accuracy of virtual bronchoscopy in measuring the length of stenosis were 92.3%, 94.3% and 92% respectively (Table 5).
|
|
Bronchoscope |
|
Total |
Sens |
Spec |
Acc |
|
|
|
<1cm |
1-2cm |
>2cm |
|
|
|
|
VB |
<1cm |
12 |
0 |
0 |
12 |
92.30% |
94.30% |
92% |
1-2cm |
2 |
10 |
0 |
12 |
||||
>2cm |
0 |
1 |
1 |
2 |
||||
Total |
|
14 |
11 |
1 |
26 |
|
|
|
Table 5 Evaluation of length of laryngotracheal stenosis by virtual bronchoscopy compared to rigid bronchoscopy
Management of laryngotracheal stenosis aims at establishing a long standing patent lumen which resists collapse without additional trauma to the tracheal wall.6 When planning for resection anastomosis, it is essential to accurately measure the length of stenotic and healthy segments to determine the feasibility of adequate anastomosis with good blood supply and no closure under tension. This also needs adequate awareness of the anatomy with meticulous dissection along with collaboration between the surgeon, radiologist and anesthetist to reach a satisfactory primary outcome.7
Virtual bronchoscopy has offered a non invasive, but expensive tool for assessment of both upper and lower airways. Rigid bronchoscopy remains the basic assessment tool for evaluating the site, grade and length of laryngotracheal stenosis. Hence, the exposure to the risks of anesthesia alleviates the need for non invasive methods like CT scanning with its new technical advances in the form of virtual bronchoscopy.
Multi-Detector Computed Tomography (MDCT) has offered the advantages of speed, thin sections and 3D reconstruction. Modern MDCT scanners (16 slices onwards) enable post-processing multi-planar reconstructions (MPR) in orthogonal and non-orthogonal planes including curved planes, with near isotropic resolution. Radiologists have been able to post process data provided by MDCT through several software’s and workstations especially designed to allow 3D/volume reconstruction with much more diagnostic accuracy.8
Virtual bronchoscopy (VB) is a post processing technique, which provides us with three-dimensional images simulating the interior of the tracheobronchial tree with any associated pathology as seen by flexible or rigid bronchoscopy. It is a simple add on technique, which has gained popularity in the recent years with increasing fields of use.9 However, VB remains a recent technique, which should be properly assessed to recognize its advantages and drawbacks trying to achieve the optimum benefit from its use. The aim of the current study is to assess the utility of virtual bronchoscopy in preoperative mapping of laryngotracheal stenosis taking conventional rigid bronchoscopy as our reference for evaluation.
Rigid bronchoscopy is an invasive procedure, which needs general anesthesia and certain level of experience with risk of complications. Here comes the role of virtual bronchoscopy as an alternative which provides us with information about the site and extent of laryngotracheal stenosis or any endotracheal or endobronchial mass.9 VB in association with axial and MPR images allow us to assess regions of the tracheobronchial tree which cannot be reached by rigid bronchoscopy due to the presence of significant stenosis or an obstructing pathology. They also give us an idea about the surrounding wall of the lesion, which cannot be assessed by rigid bronchoscopy.10
Virtual Bronchoscopy has certain limitations making it not suitable for choice as the sole investigative tool for laryngotracheal stenosis. Proper interpretation of VB images needs to be supported by axial and MPR CT images. VB images may be not accurate enough to define endotracheal or endobronchial pathology because it may not be able to detect mild mucosal abnormalities including abnormal color, vascularity or mobility of the mucosa. On the other hand, VB may overestimate tracheobronchial lesions by viewing mucous plug adherent to the wall as mass lesion or stenosis. This makes virtual bronchoscopy in need to be supplemented with rigid bronchoscopy, which also offers an approach for therapeutic intervention.10
In the current study, the sensitivity, specificity and diagnostic accuracy of virtual bronchoscopy in localizing the site of stenosis were 100% for all. This finding matches the finding of Taha et al.,11 who studied fourteen post tracheostomy patients who were scheduled for surgical treatment of post intubation stenosis of the air way were subjected to spiral CT scan with multiplanar reformatting (MPR) and virtual endoscopy(VE) followed by conventional rigid bronchoscopy(RB). They found that the sensitivity and specificity of CT in evaluation of the involvement of the subglottic larynx were 100% each.11 Also, Shweel & Shaaban12 evaluated the diagnostic utility of virtual bronchoscopy in preoperative assessment of twenty-four patients with post-traumatic tracheal stenosis who underwent tracheal resection anastomosis. They found that VB findings showed 100% sensitivity and 100% accuracy in detection of the site of stenosis.12
However, our finding was near the finding of Morshed et al.,13 who evaluated and compared various helical CT display modes virtual endoscopy (VE) and multiplanar reformations (MPR), conventional flexible tracheobronchoscopy (FT) and intra-operative (IO) findings in 37 patients with tracheal stenosis. The sensitivity of VE was 94-97%, specificity was 100% with comparison to IO findings.13 All these results support the usefulness of virtual endoscopy as a primary tool for assessment of the presence of stenosis whether laryngeal or tracheal.
On the other hand, Hoppe et al.,14 conducted a blinded controlled trial, multirow detector CT virtual bronchoscopy and flexible bronchoscopy were used to search for and grade airway stenosis in 20 patients. They stated that virtual bronchoscopy had detected 32 cases of stenosis in the central airways with a sensitivity of 90%, a specificity of 96.6% and an accuracy of 95.5%. The lower values in these studies can be explained by the use of flexible bronchoscopy as the gold standard for assessment of the airway despite the known fallacies of virtual bronchoscopy compared to rigid bronchoscopy.14
In the current study, the sensitivity, specificity and diagnostic accuracy of virtual bronchoscopy in grading the stenosis were 85.3%, 94.5% and 92% respectively. Shweel & Shaaban12 reported 96% sensitivity and 88.8% accuracy of virtual endoscopy regarding stenotic grading. Also,Morshed et al.,13 found that the sensitivity of virtual endoscopy in stenosis grading was 94%, specificity was 100% and accuracy was 95%. We attributed the lower sensitivity of virtual endoscopy in assessment of stenosis grade to the inability of virtual endoscopy to discriminate between the actual stenosis and commonly accompanying edema with resultant false higher grading of laryngotracheal stenosis.
In the current study, the sensitivity, specificity and diagnostic accuracy of virtual bronchoscopy in measuring the length of stenosis were 92.3%, 94.3% and 92% respectively. Our findings are close to the results of Shweel & Shaaban12 who reported 92.3% sensitivity and 96% accuracy in measurement of stenotic length, and length of segment planned for resection.13 But our results are somehow lower than the results of Morshed et al.,13 who showed that the sensitivity of virtual endoscopy in assessment of stenosis length was 97%, specificity was 100% and accuracy was 97%.14
Virtual endoscopy is a highly accurate method in detection of the presence of laryngotracheal stenosis. However, it needs confirmation by rigid bronchoscopy for measurement of the grade and length of stenosis in order to provide precise data preoperatively.
None.
Author declares there are no conflicts of interest.
None.

©2016 El-Naga, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.