Journal of
eISSN: 2379-6359


Research Article Volume 15 Issue 3
Department of ENT and Head-Neck Surgery, Sri Guru Ram Rai Institute of Medical and Health Sciences, India
Correspondence: Dr. Apoorva Kumar Pandey, MS (ENT), Professor & Head Department of ENT and Head-Neck Surgery, Sri Guru Ram Rai Institute of Medical and Health Sciences, Patel Nagar, Dehradun- 248001,Uttarakhand, India, Tel 9411324477
Received: August 02, 2023 | Published: September 26, 2023
Citation: Mogla S, Pandey AK, Dewan B, et al. “Swinging door” technique of tympanomeatal flap incision-elevation in type I tympanoplasty: observations, outcomes and the outlook. J Otolaryngol ENT Res. 2023;15(2):93-95. DOI: 10.15406/joentr.2023.15.00535
Tympanoplasty Type 1 is a surgical procedure aimed at repairing tympanic membrane perforations. The swinging door technique for raising the tympanomeatal flap has gained popularity due to its potential advantages, including reduced trauma to the ear canal and improved postoperative outcomes. This paper presents a retrospective analysis of 25 patients who underwent Type 1 Tympanoplasty using the swinging door technique with a single 9 o'clock /3 o’clock incision. The study evaluates the surgical success rates, audiological outcomes, and complications associated with this modified approach.
Keywords: swing door, tympanomeatal flaps, tympanoplasty, over-underlay
Tympanoplasty is a surgical intervention conducted to repair a perforated tympanic membrane (TM), with or without ossicular reconstruction, with the primary objective of preventing reinfection and restoring hearing capacity.1 The origins of tympanoplasty can be traced back to the 1950s when Wullstein and Zollner introduced the technique of utilizing an overlay graft for the reconstruction of the perforated tympanic membrane, aiming to restore the sound conduction mechanism of the middle ear.2 Type-1 Tympanoplasty is performed when there is tympanic membrane perforation without any ossicular damage.3 It is considered to be the "gold standard" surgical procedure for repairing tympanic membrane perforations, having an impressive success rate of over 90% in primary cases.
Various grafting materials have been employed in the closure of tympanic membrane perforations, including temporalis fascia, perichondrium, cartilage, periosteum, vein, dura mater, fat, and scar tissue.4 Over the years, the classical techniques of tympanoplasty, including the underlay and overlay approaches, have undergone various modifications and refinements to enhance their efficacy and outcomes.5 Each technique has its own advantages and disadvantages.
Among the available techniques, underlay Tympanoplasty stands as the most commonly employed approach, involving the placement of the graft medially to the remaining tympanic membrane or malleus. On the other hand, the overlay technique, considered more challenging, is typically reserved for anterior and total perforations or instances where underlay surgery has not succeeded. In the overlay technique, the graft is placed medially to the malleus handle and laterally to the tympanic membrane remnant after removing the squamous layer.6 In this study, instead of the classical underlay technique, we used a modified over-underlay technique of tympanoplasty using the swinging door flap technique for tympanomeatal flap elevation, introduced by Palva in the early 1960s.7,8 The objective of this study was to provide a comprehensive description of our swing-door over-underlay tympanoplasty technique and to present its surgical and functional outcomes.
This retrospective study was carried out on 25 patients of dry central perforation (small-large, subtotal) who underwent the swing-door over-underlay tympanoplasty at our institution, between January 2022 to December 2022. Postoperatively, the patients were followed up for a minimum duration of 6 months. Exclusion criteria encompassed patients who underwent ossiculoplasty or revision tympanoplasty and those with profound hearing loss. Surgical outcomes were evaluated based on graft uptake and complication rates. The graft uptake was considered successful when there was complete closure of the defect without graft lateralization or anterior angle blunting. To assess functional outcomes, pre- and postoperative audiograms were compared. Air conduction (AC) and bone conduction (BC) pure-tone averages (PTAs) were calculated using thresholds at 0.5, 1, and 2 kHz. Pre-operative and post-operative Air-bone gap were calculated and compared.
For the comparison of pre- and postoperative audiometric data, paired t-test was used and p value <0.05 was considered statistically significant (SPSS ver. 18.0).
All surgical procedures were done under general anesthesia. A post-auricular approach was utilized in all patients and the temporalis fascia was used for grafting. Margins of perforation were freshened. Subsequently, a tympanomeatal flap was elevated from the posterior canal wall down to the annulus, preserving the fibrous annulus at its bony sulcus. This technique involves the division of the tympanomeatal flap by a single incision over the 9 o'clock position ( for right ears) and 3 o’clock position ( for left ears) and then splitting of the annulus, resulting in two canal-drum skin flaps referred to as "swinging doors." Superiorly and inferiorly-based swing-door flaps were then rotated anteriorly, allowing for a better view of the entire surgical field and facilitating the removal of any pathological tissues in the middle ear (Figure 1).
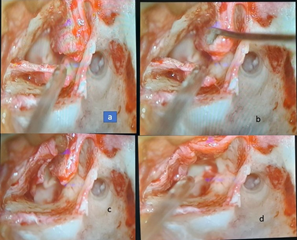
Figure 1 (a,b) Showing incision at 3 o’ clock for creation of “swinging door flaps”. (c,d) Showing superior and inferior flaps pushed anteriorly.
A fascia graft was then positioned medial to the anterior tympanic remnant and over the malleus handle before being draped onto the posterior canal wall (Figure 2).
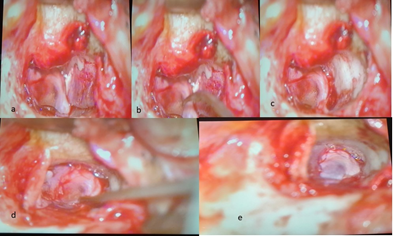
Figure 2 (a-c) Insertion of temporalis fascia along with elevated superior and inferior tympanomeatal flaps. (d-e) both flaps repositioned over the meatal wall, showing the defect covered adequately with graft.
Finally, the swinging door flaps were rotated onto the fascia graft to ensure its secure positioning and placement (Figure 3).
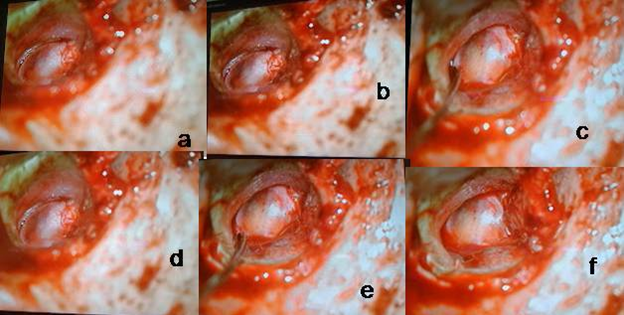
Figure 3 (a,b,d) Fascia graft tucked under TM flap. (c,e) Checking of graft tucking under inferior tympanomeatal flap. (f) Final stage after checking all quadrants of graft placement with visible single 3 o’clock incision in the left ear.
To further ensure fixation, the medial surface of the anterior tympanic remnant was made raw using a circular knife and the middle ear was initially packed with several small pieces of antibiotic-impregnated gel foam anteriorly in the protympanum area. Finally, the antibiotic-soaked pack was placed over gel foam pieces in the external auditory canal and the postaural wound was sutured back in layers.
The study enrolled a total of 25 eligible patients (8 males and 17 females) who underwent swing-door over-underlay tympanoplasty, with a mean age of 38 years (range 5 to 80 years). Out of the 25 patients, 24 achieved complete closure of the defect without lateralization or anterior angle blunting, resulting in a high graft success rate of 96%. Only 1 case experienced reperforation post-operatively, while no instances of anterior blunting, lateralization, worsening of hearing, postoperative otorrhoea, or epithelial pearls were observed. Regarding hearing improvement, the pre-and postoperative pure-tone average air–bone gaps (PTA-ABG) were obtained from three frequencies (500, 1000 and 2000 Hz) i.e. 18.4±7.3 dB and 12.7±4.9 dB respectively, indicating a significant enhancement after the surgery (P <0.05). Prior to the surgery, 12 patients (48%) had an ABG of >20 dB, but postoperatively, 24 out of 25 patients (96%) achieved an ABG of ≤20 dB, indicating an evident improvement in the distribution of ABG after the surgery.
Palva described the swing-door technique comprising a radial incision at the 9”0” clock position and thus elevating large superior and inferior tympanomeatal flaps providing good exposure of the anterior tympanic cavity and anterior fibrous annulus.7,8 Swinging door technique has been described as a popular method for the repair of posterior, inferior, and even total perforation also.9 The swing-door technique proves to be a reliable and popular approach to entering the tympanic cavity, adopted in transmeatal, endaural, and retro auricular approaches to the middle ear cavity.10 The use of the swing-door technique has also been extended in cases where ossiculoplasty (Kurz Titanium columella between footplate and eardrum) and attic reconstruction (with cartilage strips) were performed.11 This technique has been also mentioned with onlay tympanoplasty surgery. Anterior swing door incision with the elevation of a superior and inferior skin flap along with surrounding epithelium is performed in an onlay manner while closing anterior perforation with cartilage strips.12
It is important for the surgeon to carefully assess each patient's ear anatomy and condition to determine the most appropriate surgical approach. In our study, we achieved a success rate of 96% which is in accordance with the study done by Sheehy and Anderson13 in which they achieved a 97% success rate.
Similarly in studies done by Albera, et al14 and Ryan and Briggs15 achieved success rate of 93% and 98.7% respectively using the classical overlay technique. Barake et al.16 achieved a 99.3% graft uptake rate using loop underlay tympanoplasty, and Shim et al.17 achieved a 93.2% graft uptake rate using three-point fix tympanoplasty.
The postoperative complication rate was very less in our study i.e. 4% (reperforation in 1 case). There was no case of anterior blunting, lateralization of graft, worsening of hearing, postoperative otorrhoea or epithelial pearls. In this study, a postoperative air-bone gap of less than 20dB was achieved in 96% of cases. Similarly, Ryan and Briggs15 and Shim et al.,17 achieved a postoperative air-bone gap (ABG) of less than 20 dB in 82.5% and 76.4% of cases respectively. In our study, we have achieved a high graft uptake rate and significant air-bone gap closure, thus proving the effectiveness of the swinging door technique in repairing tympanic membrane perforations and improving hearing outcomes.
The swinging door technique for raising the tympanomeatal flap in tympanoplasty is a promising innovation in the field of otology. Single-incision at the 9 o’clock / 3o’clock position offers advantages such as reduced ear canal trauma, good exposure of the anterior tympanic cavity, and improved cosmetic outcomes. Existing literature suggests favorable surgical success rates and audiological outcomes with this technique. However, further prospective studies with larger sample sizes and longer follow-up periods are warranted to confirm its long-term efficacy and safety.
None.
The authors declare that there are no conflicts of interest.

©2023 Mogla, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.