Journal of
eISSN: 2379-6359


Mini Review Volume 8 Issue 6
1Otolaryngology Department Wigan and Leigh NHS Foundation Trust, UK
2Otolaryngology department Pennine Acute Hospitals NHS Trust, UK
Correspondence: Hay Mar Htun Otolaryngology Department Wigan and Leigh NHS Foundation Trust Health Education North West 8 Swaledale Galgate Lancaster LA2 0RL, UK, Tel +447807019331
Received: July 30, 2017 | Published: October 3, 2017
Citation: Htun HM, Lam M, Tse A, Kaimal K, Kumar BN (2017) Risk Stratification of Paediatric Obstructive Sleep Apnoea (OSA) for Adenotonsillectomy: How we do it at a UK District General Hospital. J Otolaryngol ENT Res 8(6): 00265. DOI: 10.15406/joentr.2017.08.00265
Obstructive Sleep Apnoea (OSA) in children is a common condition, diagnosed and managed by various medical professionals including general practitioners, paediatricians and general and paediatric otolaryngologists. If not investigated and treated early, it carries significant long-term consequences such as poor growth, failure to thrive, attention-deficit disorder, behavioural problems, poor academic performance and cardiopulmonary disease. The most common etiology is adenotonsillar hypertrophy, for which adenotonsillectomy is currently the mainstay of treatment. This article aims to raise awareness of the definition of OSA, presentation and methods of investigation of children with OSA and risk stratification in such children owing to high risk of perioperative and postoperative complications following adenotonsillectomy. We discuss current clinical guidelines including our own departmental guidelines, at a United Kingdom (UK) District General Hospital (DGH), as an example in risk stratification of children with OSA in view of adenotonsillectomy in order to improve service and optimise patient safety.
Keywords: osa, adenotonsillectomy, investigation and risk stratification of osa
OSA, obstructive sleep apnoea; SDB, sleep disordered breathing; DGH, district general hospital; PHDU, paediatric high dependency unit; PICU, paediatric intensive care unit; ODI, oxygen desaturation index
What is OSA?
Sleep Disordered Breathing (SDB) includes a spectrum of sleep related conditions: from simple snoring, which affects 3-12% of normal paediatric population to OSA affecting 2%.1 The most severe form, OSA, is due to recurrent partial (hypopnoea) or completes (apnoea) upper airway obstruction during sleep, resulting in disruption of normal ventilation and sleep pattern.2 The peak prevalence of OSA occurs in children between 2-6 years of age. At this age children have the greatest amount of lymphoid tissue in their upper airways relative to the dimensions of the airways. When the muscles of the pharynx relax during sleep, children with adenoid and tonsillar hypertrophy are at increased risk of upper airway obstruction. Obesity, craniofacial anomalies, neuromuscular disease and a variety of other disorders, such as cerebral palsy, further increase the risk for upper airway collapse due to narrowing of upper airway passages or poor muscle tone in the upper airway. It is intuitive to offer tonsillectomy, with or without adenoidectomy, to these children and is now the mainstay of treatment for SDB. In 1970 the percentage of children who underwent adenotonsillectomy for SDB was 12% compared to 77% in 2005.3 Moreover, since the first publication of Scottish Intercollegiate Guidelines Network (SIGN) guidelines for tonsillectomy in 1999, the trend in indication for tonsillectomy has gradually shifted from ‘recurrent tonsillitis’ to ‘Sleep Disordered Breathing (SDB)’. The recent Cochrane review by4 published in 2015 has shown the benefits of early surgical intervention (tonsillectomy or adenotonsillectomy) over non-surgical management in children with mild to moderate OSA without a syndrome; in terms of quality of life, symptoms and behaviour as reported by a caregiver.
Investigation of OSA
The diagnosis of OSA in children and its degree of severity may be based on the patient’s history, physical examination, and overnight pulse oximetry (or polysomnography (PSG)). In the UK, in everyday practice, the severity of OSA is usually assessed with a clinical history and examination, with the decision to operate, usually a clinical one.5 However, it is normal practice to attain an overnight sleep study pre-operatively in order to assess the degree of OSA.
History
The presence or absence of snoring neither includes nor excludes SDB, as not all children who snore have SDB, and caregivers may not observe intermittent snoring that occurs during the night.2 There are various studies in literature which have shown improvement in the quality of life (QoL) of both the child and the caregivers following adenotonsillectomy.6 Daytime sleepiness tends to be less of a problem in children than in adults; however, hyperactivity and inattention may be more characteristic features.
Physical examination
Tonsil size is readily identified using a tonsil grading scale, with tonsillar hypertrophy defined as grades 3+ or 4+. Approximately 60%-70% of children with significant tonsillar hypertrophy are likely to benefit from tonsillectomy for control of their SDB, however, only 10%-25% of obese children seem to have improvement of SDB following tonsillectomy.2
Pulse oximetry and Polysomnography (PSG)
Polysomnography (PSG) is a detailed sleep study where breathing patterns, oxygen saturation level in the blood, electroencephalography (EEG) and limb movements are monitored. Although PSG is the gold standard for diagnosing SDB in children,1 it is normally unnecessary to perform in every case and does not establish the effects of the sleep disorder on the child’s wellbeing. Furthermore, access may be limited by availability of sleep laboratories, resources and lack of consensus on interpretation of PSGs. The overnight pulse oximetry in place of formal PSG is not only cost effective, but also beneficial for identifying the so called ‘normal child with severe OSA’ who is otherwise difficult to identify with the history and examination alone.7 There are two parameters of interest that normally give an indication as to whether the child has OSA or not - the saturation nadir (min SpO2 dip) and the Oxygen Desaturation Index (ODI). The saturation nadir is the lowest oxygen desaturation over a specified period of time and <80% indicates ‘severe OSA’. The ODI is the number of times per hour of sleep that the blood's oxygen level drops by ³ 4% from baseline and an ODI of <4 is considered ‘not significant’, 4-10 ‘mild to moderate OSA’ and >10 ‘severe OSA’. In our department, children with suspected OSA are routinely sent for overnight pulse oximetry, following initial consultation and clinical assessment.
Risk stratification of children with OSA
Certain children with OSA undergoing surgery are at increased risk of perioperative and postoperative respiratory compromise, which can include laryngospasm, apnoea, pulmonary oedema, pulmonary hypertension, and pneumonia. This is due to prolonged hypoxemia and hypercarbia-induced respiratory acidosis seen in OSA, which causes pulmonary vasoconstriction leading to reversible and irreversible chronic changes in the pulmonary vasculature.8 The incidence of post-operative respiratory complications in children with OSA who undergo adenotonsillectomy has been reported to be as high as 20%, compared to <1% in children without OSA. This figure is further increased to 50% if the preoperative oxygen saturation nadir was 80% or less.7 The reasons are two-fold:
In 2009, the Royal College of Paediatric and Child Health (RCPCH) released a document on ‘Standards of Services for Children with Disorders of Sleep Physiology’ in which it is recommended that children with a saturation nadir <80%, or with any of the following factors: age <2years, severe heart or lung disease, neuromuscular disease, craniofacial abnormalities, severe neurodisability or severe obesity (BMI Standard Deviation Score >2.5), should only undergo surgery at a hospital where Paediatric Intensive Care Unit (PICU) facilities are available. In 2009, a more comprehensive criteria list for children with OSA who might require PICU facilities was published by Robb et al. 5 in collaboration with ENT-UK (Table 1). In general, availability of such facilities (paediatric high dependency unit (PHDU) or PICU) is limited to tertiary centres only and not all adeno-tonsillectomies can be performed exclusively at these tertiary centres. Many trusts now have their own protocols, with regards risk stratification of these children with OSA appropriately for adenotonsillectomy. This aims to reduce perioperative and postoperative comorbidities, whilst ensuring that resources can be utilised effectively.
Age < 3 Years old |
|||||||
Weight < 15 kg |
|||||||
Any of the following associated medical conditions |
|||||||
Severe OSA (oxygen desaturation index of >10 or min dip SpO2 <80%) |
|||||||
Obesity |
|||||||
Severe cranio-facial anomalies |
|||||||
Cerebral palsy |
|||||||
Hypotonia or neuromuscular disorders |
|||||||
Significant co-morbidities |
|||||||
Mucopolysaccharidosis and other syndromes associated with difficult airway |
|||||||
ECG and ECHO abnormalities |
|||||||
Table 1 Indications for referral to tertiary centre at Wrightington, Wigan and Leigh NHS Foundation Trust (Adapted from Robb et al.5
In our Department, children who have been referred to ENT with suspected OSA are seen in clinic to record their age and weight, history and examination findings, and are subsequently sent for overnight pulse oximetry (Figure 1). They are then followed up in clinic once they have undergone the overnight pulse oximetry. Depending on the pulse oximetry results and the risk factors (as described in Table 1), they are listed for adenotonsillectomy locally or referred to a tertiary centre. Those who underwent adenotonsillectomy locally and are known to have mild to moderate OSA (ODI of 4-10) are admitted overnight for monitoring with pulse oximetry. The recommended indications in referring children with OSA (Table 1), who might require PHDU or PICU facilities to tertiary centres, is readily available both
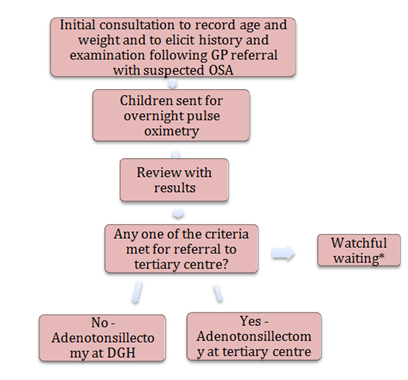
Figure 1 Algorithm in management of children with suspected OSA at Wrightington, Wigan and Leigh NHS Foundation Trust, UK.
*Watchful waiting can be adopted when there is little evidence of OSA on overnight pulse oximetry report, improvement of symptoms or caregiver’s choice.
In conclusion, OSA is a debilitating disease and carries significant morbidities if not treated early. Tonsillectomy with or without adenoidectomy is the treatment for this and carried out at both DGHs and tertiary centres. However, children with OSA are at increased risk of perioperative and postoperative respiratory compromise and should be observed on PHDU or PICU if need be. This should be monitored accordingly, with regards to their preoperative degree of severity of OSA; hence, the importance of risk stratification and optimisation of patient safety.
The procedure itself carries its own risks such as postoperative bleeding, infection, throat pain and reduced oral intake. Therefore, watchful waiting may be an alternative option for caregivers, who might be weary of both surgical and general anaesthetic risks associated with surgery, if there is little or no evidence of OSA on overnight pulse oximetry report and clinical improvement of symptoms over time. In children who are not candidates for surgery, non-surgical management such as lifestyle interventions (dietary advice, exercise programmes), medical management (intranasal and oral corticosteroids, leukotriene receptor antagonists) and mechanical interventions (continuous positive airway pressure) can be implemented.4 However, these interventions can be poorly tolerated in children.
In our Department, we continually audit our compliance with regards to appropriately risk stratifying children with OSA prior to listing for surgery - in a drive to improve service and patient safety. By identifying discrepancies and presenting the outcomes of these audits in our monthly departmental meetings, we are hoping to achieve better and more consistent standards of care for children with OSA.
None.
Author declares there are no conflicts of interest.
None.

©2017 Htun, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.