Journal of
eISSN: 2379-6359


Case Report Volume 15 Issue 1
Universitario de Poniente, Spain
Correspondence: Marcelo Dávila, Otolaryngologist at the Otolaryngology Unit of the Hospital Universitario de Poniente, Almería, Spain
Received: February 18, 2023 | Published: March 6, 2023
Citation: Dávila M, Villaroel PP, Coello JR, et al. Papillary carcinoma affecting a lateral thyroglossal cyst duct and thyroid: a case report.J Otolaryngol ENT Res. 2023;15(1):34-36. DOI: 10.15406/joentr.2023.15.00524
Thyroglossal duct cyst is the most common congenital benign cervical lesion in the population; the presence of thyroglossal duct cyst carcinoma is very rare; added to this, its association with papillary thyroid carcinoma is even more rare. Treatment is usually surgical and associated with a partial or total thyroidectomy according to each case.
Keywords: thyroglossal duct cyst carcinoma, thyroid papillary carcinoma, thyroglossal duct cyst and thyroid carcinoma
Thyroglossal duct cyst (TDC) is the most frequent congenital benign cervical lesion in the population with an incidence of 7%.1 It usually presents as a cervical lesion in the upper midline, between the hyoid bone and the thyroid gland.2 Its presentation in the lateral cervical region is very rare.3
The presence of thyroglossal duct cyst carcinoma (TDCCa) reaches 1% in TDC.4 Since its first publication in 1911 by Brentano et al., at least 300 cases of this pathology have been reported. TDCCa is usually asymptomatic at the beginning, and its definitive diagnosis is generally incidental after surgical excision and anatomopathological analysis.5–7 The most frequent histological type of TDCCa is papillary carcinoma (80%).1,2
The simultaneous presentation of papillary TDCCa with papillary thyroid carcinoma does not have a specific prevalence due to how infrequent it is in clinical practice.4,6
The treatment of papillary TDCCa is generally surgical, using the Sistrunk technique.6 Total or partial hyroidectomy is associated when the patients have associated risk factors such as age (over 45 years) and the size of the lesion, among others.8
The objective of this article is to present a case report of TDCa associated with papillary thyroid carcinoma, describe the diagnostic steps to decide the appropriate treatment, and discuss according to the actual published literature.
49-year-old male with morbid obesity and smoking habit with no other medical history of interest. He sought consultation for clinical history with a slow-growing and painless left laterocervical tumor within 1 year of evolution. On physical examination, a left cervical mass of approximately 2 x 3 cm with regular edges and no pain on palpation was found. The rest of the exploration went without significant findings.
A contrast-enhanced cervical CT study was performed that described a polylobulated lesion with a cystic component and punctate calcification measuring 28 x 33 mm located in the left laterocervical region (area IIB) associated with a 12 x 13 mm level III left cystic adenopathy (Figure 1).
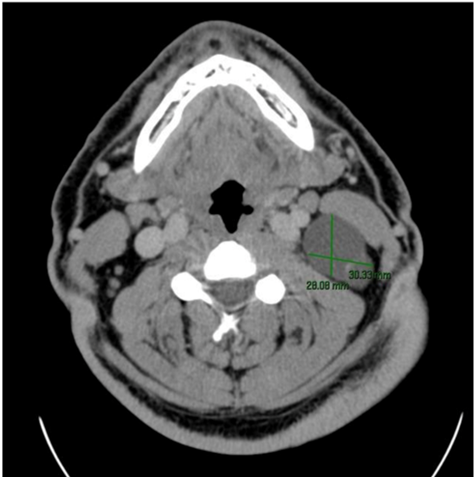
Figure 1 Neck CT scan with contrast: a polylobulated lesion with a cystic component and left punctate calcification is evident.
An ultrasound-guided fine needle aspiration (FNA) puncture was performed, where a laterocervical cystic lesion was described, probably related to a second branchial cleft cyst or a lateral thyroglossal duct cyst, with an acellular brownish discharge and negative for malignancy. There was no evidence of alteration at the level of the thyroid gland.
A surgical treatment was decided, in which a left lateral cervical approach was performed with the excision of a fatty block from area II left and adenopathy in area III. A macroscopically large cystic lesion with a brown color, elastic consistency, and serous-greenish content, measuring 3.7 x 3.2 x 2.8 cm (Figure 2), was extracted. The immediate postoperative course occurred without complications.
The anatomopathological result reported reactive left area III adenopathy and papillary thyroid carcinoma in the left lateral thyroglossal cyst duct with metastatic infiltration in two of the twelve adjacent lymph nodes.
After evaluation by our unit and the thyroid pathology surgical department, a study of the thyroid gland was completed, with normal thyroid axis hormone levels and a thyroid ultrasound finding a 3-mm colloid cyst in the right thyroid lobe (Figure 3). After these results, a second intervention was decided upon to perform a total thyroidectomy and central neck dissection. The histological result indicated papillary carcinoma in the left thyroid lobe measuring 5 mm. Having a final stage of papillary thyroid carcinoma (pT4pN2M0). Subsequently, adjuvant therapy with radioiodine was decided. Currently, the patient is under clinical follow-up by our department.
The thyroid gland begins its formation in the early embryonic period, around the third week of gestation; this occurs from endodermal tissue located between the first and second pharyngeal clefts.9
Subsequently, it begins its descent from the cecum foramen (base of the tongue), creating a thyroid diverticulum posterior and caudal to the hyoid bone, until it reaches its final location anterior to the trachea.9 In this way, it maintains its anchorage to the base of the tongue through the thyroglossal duct until the fifth week of gestation, when it begins to degenerate around the eighth week.
The TCD is considered the most frequent central cervical benign lesion; it is present in 7% of the population.1,3,6 Its origin lies in the cystic expansion of the remaining epithelium of the thyroglossal duct, with the possibility of associating ectopic thyroid tissue adhered to the cyst wall in up to 50% of cases.7 Cases of malignant degeneration into carcinomas have been reported in up to 1% of patients with TCD, with a greater tendency to affect women in the fourth decade of life.10 Its highest histological type is papillomatous (80%), followed by metastases (10–15%) and squamous cell carcinomas (5%). To this date, we are unaware of case reports of medullary thyroid carcinoma on a thyroglossal duct cyst, probably because these types of tumors arise from parafollicular cells that derive from a branchial body other than the thyroid primordium.5
There are several theories about the origin of TCDCa; the most widespread and accepted refers to metastasis of papillary carcinoma from the thyroid gland (secondary TCDCa); the possibility of having a direct "de novo" origin from the thyroid tissue itself present has also been proposed in said cyst (primary TCDCa), other possibilities contemplate a genetic predisposition of multifocal oncological origin.6
In 1974, Widstrom et al. proposed some diagnostic criteria to determine a thyroglossal cyst duct carcinoma as primary: evidence of carcinoma in the walls of the thyroglossal cyst, absence of local lymph node involvement, and absence of thyroid gland involvement; regarding this last criterion, there is controversy about the possibility of microcarcinomas present in the thyroid gland with normal preoperative studies, and that after performing a subsequent total thyroidectomy, variable results of papillary thyroid carcinoma were found. Between 25% and 56% of patients with TCDCa underwent total thyroidectomy due to risk factors.3,4
The surgical management of choice for TCDCa is Sistrunk surgery.5,8,11 The association of total thyroidectomy has been proposed when there are risk factors such as age over 45 years, lesion size in the thyroglossal duct greater than 1.5 cm, previous exposure to radiation, or associated adenopathies.6,7 This could determine this surgical-therapeutic option. Even so, a clear consensus has not been reached regarding this resolution.3,6,11
In our case, we present an infrequent presentation of a thyroglossal duct cyst both due to its location (laterality) and its content (papillary thyroid carcinoma), as well as the simultaneity with a similar lesion at the level of the thyroid gland. Our diagnosis and management are consistent with what is exposed in the current literature; even so, different possibilities could be raised regarding the primary origin of said lesion as well as the associated surgical management in the form of a protocol to be carried out in future cases.
Papillary carcinoma of a thyroglossal duct cyst is a rare entity; it is usually asymptomatic and an incidental finding. It is produced from a lesion considered benign; it requires an assessment of the risk factors for each particular case and a multidisciplinary evaluation, which leads us towards more complex solutions.
None.
Authors declare no conflict of interests.
None.

©2023 Dávila, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.