Journal of
eISSN: 2379-6359


Case Report Volume 8 Issue 5
Department of otorhinolaryngology Head and Neck Surgery King Abdulaziz Medical City, Saudi Arabia
Correspondence: Ohoud Salem Alanizi Department of otorhinolaryngology Head and Neck Surgery King Abdulaziz Medical City Riyadh, Saudi Arabia, Tel 966553444503
Received: August 26, 2017 | Published: September 20, 2017
Citation: Alanizi OS (2017) Mucoepidermoid Cancer of the Tongue Base: Case Report. J Otolaryngol ENT Res 8(5): 00260. DOI: 10.15406/joentr.2017.08.00260
We report a 45years old female with mucoepidermoid carcinoma (MEC) of the tongue base, which presented as change of voice and feeling of lump with swallowing. Up to date no clear guidelines for treatment of tongue base (MEC) and to our knowledge, this is one of few cases reported as tongue base (MEC). Although immunohistochemical studies have revolutionized understanding of the disease, little else is known of the natural history of MEC. The majority of MEC is considered low-grade, with an indolent course without recurrence or metastasis. Nonetheless, MEC requires surgical management, postoperative radiotherapy and close long-term follow-up.1
Keywords: carcinoma, salivary gland, tongue base, bronchial asthma, laryngoscope
All areas of oral cavity mucosa contain minor salivary gland except anterior part of hard palate and gingiva. Frequency of malignant tumor in salivary gland is high, however it constitute a small proportion of al head and neck malignancies Mucoepidermoid carcinoma is usually found in minor salivary gland. Tongue base MEC is rare.2,3
We present a case of MEC of the tongue base and discuss its management. We review available literature and compare management of this rare carcinoma with previously-reported cases.
A 45years old lady, known to have bronchial asthma, 1year before presentation she noticed change in her voice "hot potato voice" & feeling of throat lump, this complain was same during that period without any progression, no history of difficulty in swallowing or breathing, no bleeding or weight loss. She is non-smoker.
Physical examination
Endoscopy showed base of tongue mass, mainly in left side, smooth surface. Head and neck MRI showed moderately large mass 4×4×3cm seen in the left tonsillar\pyriform fossa regions pushing into the vallecula and extending through the tongue base posteriorly. PET CT showed prominent FDG focus localized to the BOT on the left side extending through hypopharynx on the left (SUV max 5.5) chest abdomen & pelvis was negative (Figure 1).
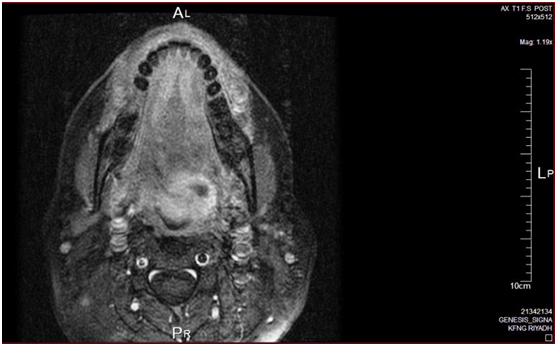
Figure 1 MRI T1 with contrast showing soft tissue mass on the left side of tongue base with irregular margins (2×3cm).
Surgical intervention
The operative note indicated that laryngoscope was performed initially to evaluate oropharynx & larynx & to determine the extent of the lesion. Transoral Exesional biopsy of tongue base tumor & selective neck dissection was performed; pathology reported a myoepithelial lesion and all lymph nodes were negative. Specimen sent to myoclinic for further investigation on March 2012 the result was favoring low grade mucoepidermoid cancer with clear cell differentiation intermediate grade. A positive immunochemistry marker was: AE1\1E3, CK5\6, 346E12, DSG3. P63 (strong, diffuse), S-100 (focal), P16 (patchy), CAM 5.2 (focal), CALPONIN & SMA, -VE: PAS, PHS-D, mucicarmine, tumor cells about the mucosal surface. Three months later Left tongue base tumor excision done by median pharyngotomy approach & neck dissection no radiation or chemotherapy was used.
Follow up
Patient seen in our clinic regularly up to two years no recurrence happened, the outcome was good; she is still under our surveillance.
MEC of tongue base is rare clinical entity; however, it is the most common malignancy of the tongue base the first case was reported in 1973.4 Over 30-year period, retrospective study of tongue base tumors conducted, total 22 cases were malignant 45% of them diagnosed as MEC.5 Gold blatt & Ellis6 found that 85% of their study cohort involving the tongue base was malignant in nature. Of these, MEC accounted for 52%, followed by adenocarcinoma (20%). MEC of the tongue presented in fifth decade and it is more common in females.6
The etiology of MEC is unknown and no sufficient studies to test the role of alcohol and tobacco smoking in its pathology, investigators have suggested trisomy 5 as a possible precursor event in MEC pathogenesis based on cytogenic studies.7 MEC has no typical cytological characteristic it contain mucin producing cells and epidermoid. The epidermoid grew in island or sheets. MEC classified in high and low grad the high grad contain epidermoid cells predominantly and looks like squamous cell carcinoma, the low grad MEC contain mucin cell more within cystic architecture and it is similar to metastatic clear renal cell carcinoma and bronchogenic carcinoma.8
Hence, appropriate work-up of the patient must also include imaging of the lungs and kidneys. One of the most important criteria for measuring the biological behavior and aggressiveness of MEC is cell proliferation. The proliferating cell nuclear antigen expression increases with the grade of malignancy.9 The risk of recurrence increased with insufficient excision and the overall prognosis is affected inversely by high grade pathology, rapid clinical presentation, old age and location.10
The local multidisplinary team discussions revealed tow different approaches either wide local excision and selective neck dissection or mandibulotomy glossectomy, free flap reconstruction and bilateral neck dissections to ensure complete tumor excision and lymph node clearance .This rationale has been supported by several other authors who have advocated wide tumor margins as intraoral MEC tends to be more aggressive, with recurrence rate of up to 30%-40% with high-grade lesions.4,11,12
Agreement reached to do middle pharyngeal excision and selective neck dissection Still the published information about the disease is scanty and according to the available data MEC is unique and has divers presentation from indolent tumors that cured by surgical extension only to more aggressive tumor that can invade and metastasis and because of this fact patients should be followed up regularly for life.13
MEC is commonest salivary gland tumor & it can present at any site in oral cavity, however MEC of tongue base is a rare entity but it accounts for 45% of tongue base malignancy and due to its rarity insufficient guidelines available for its diagnosis and management.
The authors declare no conflict of interest.
The authors declare no acknowledgement.
None.

©2017 Alanizi. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.