Journal of
eISSN: 2379-6359


Case Report Volume 6 Issue 6
Medical Technologist Mention Otorhinolaryngology, Chile
Correspondence: Victor Mercado M, Medical Technologist Mention Otorhinolaryngology, Libertad # 1348, 6th floor, Chile
Received: August 19, 2016 | Published: April 17, 2017
Citation: Mercado VM, Fernández FA, Hernandez CB, Pino CU, Novoa IC, et al. (2017) Dehiscence Syndrome Superior Semicircular Canal: A Case of Dehiscence Syndrome of the Superior Semicircular. J Otolaryngol ENT Res 6(6): 00181. DOI: 10.15406/joentr.2017.06.00181
The superior semicircular dehiscence syndrome is a pathology Described in 1998 by Minor et al. Which presents several sound induced vertigo symptoms Included, hearing loss and autophony due to bone dehiscense de este semicircular canal. The diagnosis was based on clinical and confirmation is given by temporal bone CT the. Treatment is surgical repair of expectant or continuity if the clinic is disabling. In This paper we present a case of auditory and vestibular DCSS With symptoms in issuing the phoneme "mmm".
Keywords: superior semicircular canal, dehiscence, tullio phenomenon
Dehiscence syndrome superior semicircular canal (DCSS) is a condition described in 1998 by Minor et al, presents various symptoms including dizziness induced by sound, hearing loss and autophony by the lack of bone coverage on that channel. Diagnosis is based on clinical and confirmation is obtained by computed tomography crag. The treatment is expectant or surgical repair of continuity if the clinic is incapacitating. In this article a case of DCSS with hearing and vestibular issuing the phoneme "mmm" symptoms occur.
DCSS syndrome is the presence of a solution of continuity between the apex of the superior semicircular canal (CSS) and cerebral fossa media.1 Minor et al.,2 were the first to identify this syndrome in 1998, and is characterized by the presence of vertigo and nystagmus front sounds, pressure changes in the middle ear and / or intracranial pressure. In addition symptoms such as autophony, instability, oscilloscopy and hyperacusis they may occur. Minor argued that the failure of bone coverage or dehiscence act as a "third window" moving at the level of the inner ear in addition to the oval and round windows form, allowing the transmission of vibration to the vestibular apparatus, producing the sensation of vertigo.2 The mechanism involved in syndrome DCSS would movement blister channel due to increased endolymphatic complacency, dehiscencia3 generated by the system.
A study studying thousand prevalencia4 hue-sos temporary appreciated one DCSS in 0.5% of cases, the bony plate that covered the CSS was less than 0.1mm2 at 1.4%. No local changes were found in the temporal bone that give explain pu-bone erosion, and none of these patients had a prior history of head trauma. This dehiscence was bilateral in most patients, so it is suggested that some embryonic alteration might explain these hallaz-gos, and probably some later event, such as trauma or increased intracranial pressure, could accentuate this condition, de-finishing appearance síntomas.4
Initial experiments by Tullio5 and subsequently Huizinga & Euren6,7 Demostra-rum fenestration semicircular canals in pigeons, eye and head movements caused by sound evoked in the same plane channel, denominating Tullio phenomenon. Initial clinical studies identified this faith-phe- in patients with syphilis congenital.8 However, these findings were subsequently demonstrated in conditions such as deafness congé-nita 9 of Ménière10 syndrome, perilinfática11 fistula, trauma encefalocraneano12 of Lyme13 disease and chronic otitis media with cholesteatoma semicircular14 channel erosion.
In similar pathological conditions that can result Tullio phenomenon, the pressure in the ear canal (CAE) with the with-next movement of the tympanic membrane, produces symptoms and signs vestibulares.15 This phenomenon was demonstrated in a study carried-do with chinchillas by Hirvonen et al, who investigated the changes of discharge afferents vestibular in response to changes in the CAE before and after fenestration CSS, and post reparación.16 This relationship between the plane and the directional characteristics of the known eye movements evoked both the excitation or inhibition of CSS will help define the pathophysiological characteristics of patients. Then appears, a vér-tico-rotary nystagmus following the plane of the CSS affected, counterclockwise in the case of CSS right and clockwise in the CSS izquierdo.17 The con-confirmation by computed tomography (CT) crag high resolution should rea-Lizar with cuts of at least 0.5 mm and Recon-ing in the plane channel to minimize the number of false positives.18 Another useful supplementary examination for the diagnosis of this table is vestibular myogenic evoked potentials (VEMP). With an increase in amplitude and a lower threshold to evoke the potenciales.19 Halmagyi et al evaluated the OCU-lar movements in response to low-frequency clicks in patients and healthy control group DCSS. The carrier group had a ten times greater than that observed in healthy subjects answer, therefore present this technique as a valid alternative to DCSS research in patients with dizziness and/or disequilibrium.20
Male patient 33years old, administrative mining. Browse box two years of evolution characterized by hearing loss and tinnitus pulsatile autophony left ear. In the past eight months imbalance and vertigo goal by issuing the phoneme "mmm" is added. The review highlights otoscopia standard; Weber test lateralized to the left ear. Audiometry, hearing loss presents driving left ear upward curve and a gap of 40dB (125-250-500Hz), bone conduction -10dB (Figure 1). With clinical and audiological suspected DCSS VEMP is requested stimulus Burst 500 Hz, which has a threshold of p13 waves and n23 to 65 dB nHL and asymmetry in the amplitudes of the p13 waves and n23 to 90 dB NHL (Figure 2).

Figure 2 Asymmetry in the amplitude responses, response threshold abnormally reduced left ear. Compatible with left vestibular pathology.
The video presents ausen-cia oculonistagmografía spontaneous nystagmus. The patient is asked to perform phoneme "mmm" observed appearance of horizonto-rotary nystagmus in all positions look, clockwise (Figure 3). A significant caloric testing left vestibular hyperreflexia seen as parameter.
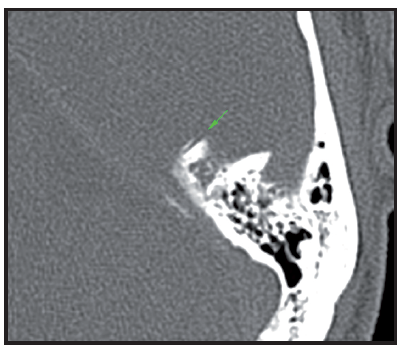
Figure 4a Reconstrucciónn MPR oblique parallel to the plane of the tympanic tegmen. Level window 600 and window width UH 2500 UH. The green arrow indicates the CSCS lacking its superior bony wall.

Figure 4b Rendering reconstruction volume highlighting the defect adjacent to the upper wall of CSCS, shown by arrows 4c rojas. Figure bone surface. MPR oblique parallel to the plane of the CSCS which highlights the ósea.VCL wall dehiscence. With the clinical suspicion of DCSS syndrome in left ear temporal bone CT is performed, with cuts of 0.5 mm, which confirms the clinical diagnosis.
The DCSS is a relatively new entity. Most publications give few details of symptoms, mainly mentioning imbalance, vertigo or oscilloscopy noise-induced pressure or maneuvers. In a series reported by Kaski,21 reports that 89% of patients had imbalance, oscilloscopy or dizziness in the presence of intense external sounds of sudden onset, such as telephone, traffic noise, cry baby, cry or dental strawberry, expanding clinical presentation of DCSS. A third of them had Tullio phenomenon with his own voice when speaking or making buzz. Changes in intracranial pressure by coughing, nose blowing, flying, causing symptoms in 25% of subjects. In addition, patients often reported hearing unusual phenomena related to body sounds as heard his footsteps, his muscles when chewing or eye movements. Pulsatile tinnitus was a frequent complaint. It is important to consider the vertigo that occurs in the dental office, and the differential diagnosis between benign paroxysmal positional vertigo (BPPV) and DCSS, as they will be triggered differently. The intensity of the sound generated by the turbine reaches the inner ear by bone conduction, it is transmitted by solid media, such as the skull, with enormous efficiency and maximum speed. However, when it reaches the ear of a patient with DCSS Tullio phenomenon it occurs because above 95 dB SPL to trigger a precise rotational vertigo. All these inconveniences previously mentioned are caused by low frequency sounds (0.5-2kHz). The patient reported, particularly referring symptoms when issuing the phoneme "mmm" which generates pressure changes as well as a retro reflected resonance, because the phonatory tube with a frequency of about 110Hz is partially occluded, but includes harmonics and other complex frequencies noise. Given the nature of the problem, look for abnormal eye movements against exposure to sound stimuli, inducing positive pressure and/or negative in the CAE during impedance or performing Valsalva maneuver against glottis open and closed glottis. Increased intracranial pressure with the Valsalva maneuver and closed glottis, is transmitted in the CSS, through the meninges and the perilymph of the aqueduct coclear,21 generating eye movements in the same plane but opposite direction (ampulípeta) to the observed during the loud noise. Pathophysiologically the "third window" causes a low-frequency conductive hearing loss is accompanied by thresholds via bone normal or even lower than 0 dB, with a normal acoustic reflex, allowing us to exclude the otosclerosis as a differential diagnosis. Bone conduction humans is less efficient than air conduction, however, the presence of a DCSS generate a vibration of the skull that may cause the oscillation of the dura over the defect, leading to the creation of standing waves and amplification sound, which is transmitted directly to the inner ear fluids with little attenuation, causing stimulation of hair cells in the cochlea at the appropriate frequencies. This explains the symptoms of tinnitus and pulsatile22 autophony.
The VEMP is an objective test that evaluates the generation disynaptic vestibulo-cervi-cal. This determines the function of the saccule, posterior labyrinth and inferior vestibular nerve principalmente.23,24 It is thought that the ori-page VEMP by stimulation saccule because the latter forms the vestibular organ terminal more sensitive to sound, to be close to the look-tana oval. The large intensity of motion of the perilymph produce greater stimulation of saccular receptors. Furthermore, most neurons sensitive vestibular nerve clicks, which would meet inclinations are in the saccular macula and there is diri-gene by afferents vestibular nerve to the lateral and inferior25 vestibular nucleus. Thus, an auditory stimulus type click brief high intensity will produce an ipsilateral inhibitory potential of high amplitude and short latency in the sternocleidomastoid muscle when it is find tonically contracted and exci-rio in the contralateral muscle. This muscle response will be represented as a wave with a positive peak at 13 ms after a negative and the 23ms after stimulation peak. In normal subjects the VEMPs has a threshold usually 90-95dB. In patients with DCSS, the threshold is about 20dB lower than the normal subjects and breadth usual level of stimulation of 100-105dB can be mind-abnormally high (> 300 microvolts). Patients with DCSS also have a lobby oculomotor reflex evoked by click abnormally intense and bajo26,27 threshold.
There is a notable difference between the impact-cia radiological and anatomical. While in post mortem studies in temporal bones an incidence of 0.5% 4 was found, in contrast with the results obtained by CT, ranging from 1% to 17%.28,29 This may be because the resolution of CT not sufficient for bone near deli-very fino;30 the orientation of the cuts can increase the number of false positives31 and positioning the patient's head varies with each study and therefore there is no standardized variable.
Cloutier32 proposed holding TC with re-construction in the plane of committed channel (Pöschl), reducing the prevalence of radiological DCSS 10% to 4% with coronal reconstructions. However even diagnosis is made on this box.
The initial treatment of this disease should be conservative, avoiding the patient, the actions that trigger the clínica.2 If this behavior is not sufficient or the symptoms are disabling it may refer the patient a resolution quirúrgica,3 consisting of closing the communication between the channel and the floor of the middle fossa, showing a clear improvement of vestibular symptoms and disappearance of Tullio phenom-enon. The routes proposed for the closure of the fistula are transmastoid or through middle cranial fossa. Once identified dehiscence, it is sealed with bone wax or a bone graft could be added temporal33 muscle fascia. Other alternatives such as fascia, fibrin glue, bone graft and hydroxyapatite cement have also been used in the repair of the defect, with 60. Dehiscence syndrome SEMICIRCULAR SUPERIOR CANAL. A CASE REPORT - V Market, F Fernandez Hernandez C, C Pino, I Novoa, P Herrera various results.1 There is initially described by Silverstein34 innovative approach, who sugi-gested that dampen the sensitivity of the inner ear by strengthening the oval and round window with fascia may relieve symptoms in some patients, reducing complications Aque-Llos more invasive approaches, via transcranial. twenty-four patients centers who opted for the minimally invasive approach by strengthening the oval window and / or round were studied. The analysis revealed a STAT-cally significant improvement in almost all symptoms except for hearing loss.
Finally, this clinical entity has a high rate of false positives and a variety of clinical presentations therefore we must consider in detail the diagnos-cos differential and supported by complementary examinations get raise this diagnosis with certainty and define the best patient treatment for those carriers DCSS.
None.
Author declares there are no conflicts of interest.
None.

©2017 Mercado, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.