Journal of
eISSN: 2379-6359


Research Article Volume 4 Issue 6
Department of Otorhinolaryngology Head and Neck Surgery, Faculty of Medicine Universitas Gadjah Mada, Indonesia
Correspondence: Sagung Rai Indrasari, Department of Otorhinolaryngology Head and Neck Surgery, Faculty of Medicine, Universitas Gadjah Mada, Jl. Farmako, Sekip, Yogyakarta, Indonesia, Tel +628112503932
Received: September 05, 2016 | Published: October 14, 2016
Citation: Indrasari SR, Sastrowijoto S, Astuti I, Hariwiyanto B, Tan IB (2016) Clinical Study on Photodynamic Therapy (PDT) In Patients with Nasopharyngeal Carcinoma in Yogyakarta Review of Life Expectancy and Cytokine Level. J Otolaryngol ENT Res 4(6): 00120. DOI: 10.15406/joentr.2016.04.00120
Background: Nasopharyngeal carcinoma is a malignancy in nasopharynx cavity originated from mucosal epithelial cell of nasopharynx. In Indonesia, nasopharyngeal carcinoma is the most considerable malignancy in head and neck area with the highest mortality rate.
Objective: To perceive that photodynamic therapy in nasopharyngeal carcinoma either residual or recurrence patients after receiving radiation or in chemo radiation therapy will yield a well-responded therapy, better life expectancy compared to those who didn't receive PDT, and inducing systemic anti-tumor response which was marked by the increased level of immune-response cytokines.
Methods: This research took place in Department of Otorhinolaryngology Head and Neck Surgery Faculty of Medicine University of Gadjah Mada/Dr Sardjito General Hospital Yogyakarta, Indonesia using cohort retrospective design. The subjects of this research are patients with residual or recurrence nasopharyngeal carcinoma who had received photodynamic therapies between the years 2005-2011. Pre and posttest examination were used to test the hypothesis of the cytokines level difference before and after photodynamic therapies.
Results: As much as 58.1% patients were men, and 41.9% of patients were female. Most of the patients were above 40years of age. As much as 21 out of 31 patients (67.7%) were previously diagnosed as nasopharyngeal carcinomas in late stages, in this case the given treatment was chemo radiation. The 5 years life expectancy of residual or recurrence nasopharyngeal carcinoma is 60.7%. This number was preferable compared to the life expectancy of nasopharyngeal carcinoma patients who received standard therapy of either radiation or chemo radiation. Residual and recurrence nasopharyngeal carcinoma patients diagnosed between year 2009- 2013 without photodynamic therapy showed the 5year overall survival rate as much as 22.9% with the median 23.6 months. There was a significant difference of life expectancy either clinically or statistically in patients with residual of recurrence nasopharyngeal cancer who received PDT compared to those who did not (p=0.004).
Conclusion: In long-term observation, it was reported that photodynamic therapy (PDT) increased the 5years survival rate in patients with residual or recurrence nasopharyngeal carcinoma. Patients who received PDT had life expectancy 5years longer than patients who did not receive PDT.
The result of prognostic factors analysis showed that gender and age <40years old each played a role as factors which affect the life expectancy.
Keywords: nasopharyngeal carcinoma, photodynamic therapy
NPC, nasopharyngeal carcinoma; PDT, photodynamic therapy; TAA, tumor associated antigen; IFNγ, interferon gamma; TNFα, tumor necrosing factor alpha
Nasopharyngeal carcinoma (NPC) is a malignancy in nasopharynx cavity that originates from mucosal epithelial cell of nasopharynx. Nasopharyngeal carcinoma has high mortality rate. Most incident were found in South of Asia, including Malaysia and Indonesia with an incident rate around 5-15 patients per 100.000 people each year.1 In Indonesia, nasopharyngeal carcinoma is the most common malignancy in head and neck area with the highest mortality rate. A survey held by Health Ministry of Indonesia in the year 1987 showed that the incidence rate of NPC is 4, 7 per 100.000 each year, with the ratio of 3, 5: 1, 2 between male and female.2 Few researches were held in some hospitals showed that NPC is the most common malignancy compared to other malignancy in head and neck area with the prevalence of 40-80%.3
The issue encountered while managing NPC is the availability of radiotherapy device in Indonesian which is not equivalent to the number of NPC patients who need treatments, therefore there’s tardiness in administrating standardized therapy. Among 50 patients diagnosed with NPC in the year 2009-2010 in Department of Otorhinolaryngology Head and Neck Surgery Dr. Sardjito Hospital, Yogyakarta, Indonesia, 37 of these patients (74%) had to wait for more than 2 months to receive radiotherapy, 10 of these patients had to wait until up to 6 months even longer. The procrastination of the therapy given to NPC has concequence of wretched theraupeutic outcome and may lead to considerable cases of residual and recurrence.
Photodynamic therapy (PDT) is a non-surgical therapy, which is minimally invasive, using source of light to activate photosensitizer drug. PDT has been used for additional therapy in many cancers including NPC. Generally, PDT can be given before or after chemotherapy, radiotherapy, or surgery without undermining the effectiveness of those modalities mentioned. In Yogyakarta, research about PDT for residual or recurrent NPC patients has been held since 2005, as much as 34 patients received PDT. Evaluation of the theraupetic response was done on twelve weeks after the administration using nasopharyngeal endoscopy, CT-scan, and nasopharyngeal biopsy. There were 25 patients who showed good results, 5 patients were still sustaining residue, 2 patients were unable to undergo the evaluation because they didn’t show up for the examination and 2 other patients were still waiting for the evaluation schedule.4
Previous researchers performed a study of PDT in 4 patients with recurrent NPC. It was reported that all patients were able to survive for up to 5years.5 Another research performed on PDT in 12 patients with recurrent NPC, a good theraupeutic result was proved by CT-Scan or MRI 6 months after receiving PDT.6
There was another clinical research on Foscan-mediated PDT of 20 patients with oral cavity malignancy. This research showed that PDT gave a pretty good result on therapy for squamous cell carcinoma of the oral cavity, also the ability to readminister the Foscan-mediated therapy to the same patient without any side effect.7 In accordance to previous research done by Koberlik et al (2008) did research on PDT from mices implanted with fibrosarcoma tumor cells. This research proves the existence of acute phase response after PDT administration.8
In addition, another researcher went over the systemic immune response in basal cell carcinoma patients. The research was applying the measurement of systemic immune response against Tumor Associated Antigen (TAA) from patients who receieved PDT compared to those who had surgery. The result of the research showed that PDT given locally to the patients was able to enhance the systemic immune response against tumor.9
This research was held in Department of Otorhinolaryngology Head and Neck Surgery Dr. Sardjito Hospital, it was differ from other previous researches for it was arranged as aresesarch to find out antitumor systemic immune response in NPC patients who received photodynamic therapy (PDT). In this research, there will be a few examination on some systemic immune response parameter in residual or recurrent NPC patients who receieved PDT.
This research is a clinical study on photodynamic therapy on NPC patients. The study was held in Department of Otorhinolaryngology Head and Neck Surgery in Dr. Sardjito Hospital using retrospective cohort design, the subjects were patients with residual or recurrent nasopharyngeal carcinoma who had received photodynamic therapy (PDT) during the year 2005-2011 who met the inclusion and exclusion criteria. The inclusion criteria of the subjects were patients with WHO type 2 or type 3 residual or recurrent nasopharyngeal carcinoma. Confirmed biopsy of nasopharynx who had receieved PDT with the dose of 0, 15mg/kg body weight and DLI for 4 days, there was no neck lymphnode metastasis, or with neck lymphnode metastasis in maximum N2 stage, and no distant metastasis. Whereas the exclusion criterias were patients with incomplete medical data, serum samples, and those who refused to participate in the research. Pre and post test analysis was appliedto test the hypothesis of the alteration of cytokine level before and after PDT.
There were 31 patients who met both inclusion and exclusion criterias which then registered as a research subjects to be analyzed in clinical parameter. The analysis of cytokines; Interleukin-12, Interleukin-18, Interleukin-2, and Interferon Gamma were applied to the serum samples of the patients where these serum samples were completed and stored in Laboratory of Biomolecular Faculty of Medicine Universitas Gadjah Mada.
To the residual or recurrent NPC patients who had received PDT at the Department of Otorhinolaryngology Head and Neck Surgery Dr. Sardjito Hospital during the period of 2005-2011, informed consent forms were given to ensure their willingness to participate inthis research. Patients who were willing to participate would undergo laboratory examination on the serum samples which had already taken before and after PDT administration, and during the follow up period, the serum samples then stored in the Laboratory of Biomolecular Faculty of Medicine Universitas Gadjah Mada. All clinical data of the patients were collected from medical records.
The clinical data collected were theraupetic response to PDT, recurrency (if existed), also an analysis for 5years life expectancy was performed. Determination of the theraupeutic response in NPC patients after PDT was performed in the same manner as NPC patients who receieved chemoradiation, which includes complete ear, nose, throat, head, and neck physical examination, nasopharynx endoscopy, nasopharynx CT-Scan, and nasopharynx biopsy guided by endoscopy. Distant metastasis was excluded by lung radiologic examination and abdominal USG. These data were recorded in patients’ medical records. Examination of Interleukin-12, Interleukin-18, Interleukin-2, and Interferon Gamma in qualified serum samples were performed by using ELISA method.
As comparations are the NPC patients who had gone through radiation or chemoradiation and were undergoing residue or recurrency but did not receive PDT. The clinical data of these patients were also recorded and analyzed for life expectancy. Statisctical analysis was executed using SPSS program. The characterisctic of the subjects were presented in a characterictic table. Results reported include therapeutic response in the form of nasopharynx appearance in biopsy. Five year life expectancy as an overall survival rate was analyzed, along with prognostic factors of PDT on NPC patients by comparing the life expectancy based on prognostic factors which were gender, age, biopsy results, and NPC stages.
Paired t-test was applied for comparative study for numeric non-parametris variables, Wilcoxon tes was applied to analyze the mean difference between the cytokine levels; IL-12, IL-18, IL-2 and IFNγ before and after PDT, follow up 1 and follow up 2. This research had already gained permission from Ethical Committee Faculty of Medicine Universitas Gadjah Mada by firstly submitting a proposal and presentation in the presence of Ethical Committee evaluation team.
The research was carried out on residual or recurrent nasopharyngeal carcinoma patients who had receieved PDT. As much as 31 patients fulfilled the inclusion and exclusion criterias therefore were registered as subjects of this research.
Life sustainability of residual or recurrent NPC patients (Table 1) & (Figure 1)
Five years life expectancy of residual or recurrent nasopharyngeal carcinoma patients who received PDT is 60, 7%.
|
PDT (n=31) |
Non PDT (n=53) |
p |
||
Variables |
Amount |
% |
Amount |
% |
|
Gender |
0.062 |
||||
Male |
18 |
58, 1 |
41 |
77, 4 |
|
Female |
13 |
41, 9 |
12 |
22, 6 |
|
Age |
0.125 |
||||
<40 years old |
9 |
29, 0 |
8 |
15, 1 |
|
≥40 years old |
22 |
71,0 |
45 |
84, 9 |
|
Stages on First Diagnosis |
0.399 |
||||
Stadium Awal |
10 |
32, 3 |
22 |
41, 5 |
|
Stadium Lanjut |
21 |
67, 7 |
31 |
58, 5 |
|
Treatment Before Receiving PDT |
<0.001 |
||||
RT |
10 |
32, 3 |
1 |
1, 9 |
|
CRT |
21 |
67, 7 |
52 |
98, 1 |
|
Biopsy Result Post PDT |
|||||
Tumor (+) |
5 |
16,1 |
|||
Tumor (-) |
26 |
83,9 |
|
|
|
Table 1 Description characteristics of research subjects
Nasopharyngeal carcinoma patients diagnosed between the year of 2009-2013 who had been undergoing residu or recurred and did not receive PDT showed 5years life expectancy or 5years overall survival rate of 22,9% with median of 23,6months. There’s a significant difference in life expectancy whether it’s clinically or statistically between residual or recurrent NPC patients with PDT compared to without PDT (p=0,004) (Figure 2).
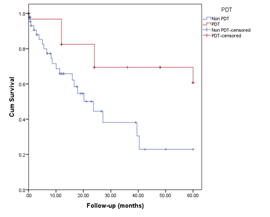
Figure 2 Five years life expectancy of residual and recurrent NPC patients with PDT compared to without PDT.
The analysis of prognostic factors affecting residual or recurrent NPC patients with PDT was performed, the factors analyzed were gender, age, nasopharynx biopsy result post PDT, also the clinical stages when the diagnosis of NPC was first made. The evaluation of five years life expectancy was based on those prognostic factors. Based on gender, it was found that the five years life expectancy of male patients are higher (73, 5%) compared to females (42, 2%) where this difference is statistically mattered (p=0.045). Mean overall survival on males is 72%, whereas female patients is 45, 257%, it can be concluded that male patients have higher five years life expectancy than female patients (Figure 3).
In this research, the analysis of 5 years life expectancy based on age showed that patients ≤40 years old have higher life expectancy (76, 2%) compared to those who are >40years old (53%), even though it is not statistically significant (p=0,417). Younger age NPC patients (≤40years old) commonly have better health status, therefore 5years life expectancy are higher compared to those who are over 40 years old. Mean overall survival on patients age ≤40 years old are 68,381, whereas patients >40years old are 57,591. Although it is not statistically significant, it can be concluded that residual or recurrent NPC patients who were ≤40years old have higher life expectancy (Figure 4).
The nasopharynx biopsy result post PDT showed 26 out of 31 (83, 9%) patients are negative, there are no malignancy in nasopharynx cavity, while 5 (16, 1%) patients still have positive result, some malignancy are still found in nasopharynx cavity. Local response rate 83, 9% proves that photodynamic therapy is an effective therapy to control local tumors in residual or recurrent NPC patients (Figure 5).
In analysis of life expectancy based on nasopharynx biopsy result post PDT, it was found that some patients who still have tumors in nasopharynx have higher life expectancy (80%) compared to patients who have negative biopsy result (57, 8%). This result is not statistically significant (p=0,638). These results possibly caused by the amount of positive result patients are only 5 compared to negative result patient, which are 26. Mean overall survival on negative result patients is 59,637 meanwhile patients with positive result are 50,400 (Figure 6).
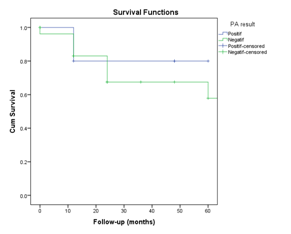
Figure 6 Kaplan Meier graphic of 5 years life expectancy on NPC patients post PDT based on biopsy result.
In analysis of life expectancy based on stages on firstly diagnosed post PDT, it was found that patient with early stage have lower life expectancy (53, 3%) compared to late stages (62, 1%) even so it is not statistically significant (p=0,521) (Figure 7).
The analysis of factors affecting life ability of NPC patients who receive PDT, which are gender, age, biopsy result, and clinical stages, using cox-regression analysis with backward method. In this method, all prognostic factors were entered into multivariate analysis. Periodically, variable that had no effect will be cut off of the analysis. The process will stop if there’s no more variable being cut off of the analysis. Gender was found to be the factor that remained still in the analysis. Male gender as prognostic factor on life ability of the NPC patient post PDT even though it is not statistically significant with OR 0,280 (p=0,073) (Table 2).
|
|
|
|
|
|
|
|
95,0% CI for Exp(B) |
|
|
|
B |
SE |
Wald |
df |
Sig. |
Exp(B) |
Lower |
Upper |
Step 1 |
Gender |
-1541 |
0,863 |
3,190 |
1 |
0,074 |
0,214 |
0,039 |
1,162 |
PA Results |
0,243 |
1,171 |
0,043 |
1 |
0,835 |
1,275 |
0,129 |
12,651 |
|
Age |
-0,836 |
0,829 |
1,017 |
1 |
0,313 |
0,434 |
0,085 |
2,201 |
|
Stages |
0,328 |
0,763 |
0,185 |
1 |
0,667 |
1,389 |
0,311 |
6,200 |
|
Step 2 |
Gender |
-1,472 |
0,789 |
3,483 |
1 |
0,062 |
0,229 |
0,049 |
1,077 |
Age |
-0,811 |
0,820 |
0,979 |
1 |
0,323 |
0,445 |
0,089 |
2,216 |
|
Stage |
0,296 |
0,750 |
0,155 |
1 |
0,694 |
1,344 |
0,309 |
5,851 |
|
Step 3 |
Gender |
-1,340 |
0,714 |
3,524 |
1 |
0,060 |
0,262 |
0,065 |
1,061 |
Age |
-0,754 |
0,806 |
0,874 |
1 |
0,350 |
0,471 |
0,097 |
2,285 |
|
Step 4 |
Gender |
-1,272 |
0,710 |
3,207 |
1 |
0,073 |
0,280 |
0,070 |
1,128 |
Table 2 Cox Regression Analysis on PDT Prognostic Factors
Changes in cytokines’ level
In this research, after the sample serum collection was done which had been stored in Laboratory of Bimolecular Faculty of Medicine Gadjah Mada University, some samples were found to be unqualified for analysis. This was caused by the lack of volume of the stored samples; therefore the examination of cytokine level could not be done. Some other samples are found to have incomplete clinical data of patients and also be unqualified for analysis. The final amounts of qualified samples were 14 patients. Ten out of fourteen patients were males (71, 43%) and the rest were females. Most patients are >40years old (71, 43%) with youngest of 18years old, and the oldest of 63years old. The average age for patients who received PDT was 43years old. Most patients (85, 71%) were on late stages when they were first diagnosed (Table 3).
Variables |
Amounts |
% |
Gender |
||
Male |
10 |
71,43 |
Female |
4 |
28,57 |
Age (year) |
||
<40 years old |
4 |
28,57 |
≥40 years old |
10 |
71,43 |
Minimum |
18 |
|
Maximum |
63 |
|
Average |
43 |
|
Stages on First Diagnosis |
||
Early Stage |
2 |
14,29 |
Late Stage |
12 |
85,71 |
PA Results Post PDT |
||
Tumor (+) |
2 |
14,29 |
Tumor (-) |
12 |
85,71 |
Table 3 Characteristics of the Subjects (n=14)
In pathology anatomy examination of nasopharynx biopsy post PDT, most patients (85, 71%) had no tumor (Figure 8).
Pre PDT samples were taken 3days before PDT administration; post PDT samples were taken 90days after PDT. Follow up 1 sample were taken 181days after PDT, and follow up 2 samples were taken 267days after PDT. All of these samples were recorded and analyzed. The interleukin level was defined in pg/ml.
Interleukin-12 levels
In interleukin-12 examination, the mean value of interleukin-12 levels before PDT was 16, 857 pg/ml. There was an elevation of IL-12 level post PDT and in follow up 1 and 2 (Table 4).
IL-12 |
Mean |
SD |
Pre PDT |
16,857 |
24,156 |
Post PDT |
21,071 |
32,226 |
Follow-up 1 |
26,929 |
35,343 |
Follow-up 2 |
27,429 |
30,744 |
Table 4 Average Level of Interleukin-12 pre and post PDT (pg/ml)
The graphic below describes changes in IL-12 levels in NPC patients who received PDT. The elevation can be observed in post PDT, follow up 1 and follow up 2 periods (Figure 9 & 10).
In pre post PDT analysis IL-12 levels post PDT compared to pre PDT, there was an elevation of 4,214 (24,9%) even though it’s clinically significant but statistically not significant (p=0,531) (Table 5) (Figure 11).
|
Mean |
Difference (s.b) |
CI95% |
P Value |
IL-12 Pre PDT |
16,857 |
4,214 (24,502) |
-9,933 - 18,361 |
0,531 |
IL-12 Post PDT |
21,071 |
|
|
|
Table 5 Paired T-test result on Interleukin-12 level
Pre and post analysis of Interleukin-12 level in follow up 1 period compared to pre PDT showed an elevation of 10,071 (59,7%), this elevation is not statistically significant (p=0,283). But, this nearly 60% elevation is clinically significant (Table 6).
|
Average |
Difference (s.b) |
CI95% |
P Value |
IL-12 pre PDT |
16,857 |
10,071 (33,628) |
-9,345 |
|
IL-12 Follow-up 1 |
26,929 |
|
-29,488 |
0,283 |
Table 6 Paired T-test result of Interleukin-12 level (n=14)
Changes in Interleukin-12 levels in NPC patients post PDT was also found in follow-up 2 period. There was an elevation of 10, 571 (62, 7%) showed in follow-up 2 period compared to pre PDT. This result is clinically significant (Figure 12).
Pre and post analysis of Interleukin-12 level in follow up 2 period compared to pre PDT showed an elevation of 10,571 (62, 7%), this elevation is not statistically significant (p=0, 200) (Table 7).
|
Average |
Difference (s.b) |
CI95% |
P Value |
IL-12 Pre PDT |
16,857 |
10,571 (29,330) |
-6,363 -27,506 |
0,200 |
IL-12 Follow-up 2 |
27,429 |
|
|
|
Table 7 Paired T-test result of Interleukin-12 level (n=14)
Interleukin-2 level
Interleukin-2 level in NPC patients who receives PDT also higher in follow-up 1 period compared to pre PDT. The level difference found was 3,686 (1, 9%) (Figure 13).
Pre and post analysis of Interleukin-2 level in follow up 1 period compared to pre PDT showed an elevation of 3,686 (1, 9%), this elevation is not statistically significant (p=0, 380) (Table 8).
|
Average |
Difference (s.b) |
CI95% |
P Value |
IL-2 pre PDT |
188,110 |
3,686 (15,164) |
5,069 -12,441 |
0,380 |
IL-2 Follow-up 1 |
191,796 |
|
|
|
Table 8 Paired T-test result of Interleukin-2 level (n=14)
The Interleukin-2 level in follow-up 2 periods was found to be 9,153 lower than pre PDT (Figure 14).
Pre and post analysis of Interleukin-2 level in follow up 2 period compared to pre PDT showed a difference, even though statistically this difference is not significant (p=0, 080) (Table 9).
|
Average |
Difference (s.b) |
CI95% |
P Value |
IL-2 pre PDT |
188,110 |
-9,153 (18,049) |
1,268 -19,575 |
0,080 |
IL-2 Follow-up 2 |
178,957 |
|
|
|
Table 9 Paired T-test result of Interleukin-2 level (n=14)
Interleukin-18 levels
The average level of Interleukin-18 in NPC patients’ pre PDT are 258, 500 pg/ml. There was an elevation of Interleukin-18 level in NPC patients post PDT. In follow-up 1 and follow-up 2 period, lower number of IL-18 was found compared to pre PDT (Table 10) (Figure 15).
IL-18 |
Mean |
S.D |
Pre PDT |
258,500 |
57,713 |
Post PDT |
277,071 |
43,120 |
Follow-up 1 |
244,571 |
53,284 |
Follow-up 2 |
226,714 |
54,934 |
Table 10 Average Level of Interleukin-18 pre and post PDT (pg/ml)
The graphic above showed changes in IL-18 level pre PDT, post PDT, follow-up 1 and follow-up 2 period. An elevation can be observed in post PDT compared to pre PDT. The IL-18 level then declined in follow-up1 and follow-up 2 periods. Analysis on IL-18 level showed elevation of 18,571 (7, 1%) in post PDT compared to pre PDT (Figure 16) (Table 11).
|
Average |
Difference (s.b) |
CI95% |
P value |
IL-18 Pre PDT |
258,500 |
18,571 (37,439) |
-3,045 - 40,188 |
0,086 |
IL-18 Post PDT |
277,071 |
|
|
|
Table 11 Paired T-test result of Interleukin-18 level (n=14)
Pre and post analysis of Interleukin-18 level in post PDT compared to pre PDT showed an elevation even though it is not statistically significant (p=0, 086) (Figure 17).
Analysis on IL-18 level showed a devaluation of 13,929 in follow-up 1 period compared to pre PDT (Table 12).
|
Average |
Difference (s.b) |
CI95% |
P Value |
IL-18 pre PDT |
258,500 |
-13,929 (33,119) |
-33,051 - 5,194 |
0,140 |
IL-18 Follow-up 1 |
244,571 |
|
|
|
Table 12 Paired T-test result of Interleukin-18 level (n=14)
Pre and post analysis of Interleukin-18 level in follow-up 1 period compared to pre PDT showed a difference even though it is not statistically significant (p=0,140). The Interleukin-18 level in follow-up 2 period were found to be 31,786 (12, 3%) lower compared to pre PDT (Figure 18).
Pre and post analysis of Interleukin-18 level in follow-up 2 period compared to pre PDT showed a difference even though it is not statistically significant (p=0, 085) (Table 13).
|
Average |
Difference (s.b) |
CI95% |
P Value |
IL-18 Pre PDT |
258,500 |
-31,786 (63,899) |
-68,680 -5,109 |
0,085 |
IL-18 Follow-up 2 |
226,714 |
|
|
|
Table 13 Paired T-test result of Interleukin-18 level (n=14)
IFNγ (Interferon Gamma) levels on NPC Patients who received PDT
The average level of IFNγ in NPC patients pre PDT are 45,643 pg/ml. There was a devaluation of IFNγ level in NPC patients post PDT also in follow-up 1 and follow-up 2 patients. Graphic below showed IFNγ level in NPC patient pre PDT, post PDT, follow-up 1 and follow-up 2 periods (Table 14).
IFNγ |
Mean |
S.D |
Pre PDT |
45,643 |
33,410 |
Post PDT |
34,571 |
25,779 |
Follow-up 1 |
21,643 |
22,697 |
Follow-up 2 |
14,714 |
19,839 |
Table 14 Average Level of IFNγ pre and post PDT (pg/ml)
Graphic below showed the changes of Interferon Gamma level in NPC patient pre PDT, post PDT, follow-up 1 and follow-up 2 periods. There was a linear devaluation of interferon gamma level in residual and recurrent NPC patients after PDT (Figure 19).
The interferon gamma levels in NPC patient’s pre PDT were 45,643. There was a devaluation of level post PDT as much as 11,071 or 24, 3% compared to pre PDT. This devaluation is clinically significant (Figure 20).
Pre and post analysis of interferon gamma level in post PDT compared to pre PDT showed a devaluation of 11,071 or 24, 3%, this number is statistically significant (p=0.026). In follow-up 1 period, there was a devaluation of 24,00 or 52, 6% compared to pre PDT. This result is very much clinically significant for the devaluation reach half of the amount pre PDT (Table 15) (Figure 21).
|
Average |
Difference (s.b) |
CI95% |
P Value |
IFN Gamma Pre PDT |
45,643 |
-11,071 (16,453) |
1,572 - 20,571 |
0,026 |
IFN Gamma Post PDT |
34,571 |
|
|
|
Table 15 Paired T-test result of IFNγ level (n=14)
Pre and post analysis of interferon gamma level in follow-up 1 period compared to pre PDT showed a devaluation of 24,00 or 52, 3%, there was a statistically significant difference (p=0,005) (Table 16).
|
Average |
Difference (s.b) |
CI95% |
P Value |
IFN gamma pre PDT |
45,643 |
-24,00 (26,349) |
8,786 - 39,314 |
0,005 |
IFN gamma Follow-up 1 |
21,643 |
|
|
|
Table 16 Paired T-test result of IFNγ level (n=14)
In follow-up 2 periods, there was a devaluation of interferon gamma level as much as 30,929 or 60, 79% compared to pre PDT. This devaluation was more than half the amount of interferon gamma pre PDT; therefore it is surely clinically significant (Figure 22).
Pre and post analysis of interferon gamma level in follow-up 2 period compared to pre PDT showed a devaluation of 30,929 or 67, 76% which is statistically significant (p=0,001) (Table 17).
|
Average |
Difference (s.b) |
CI95% |
P Value |
IFN gamma pre PDT |
45,643 |
-30,929 (25,527) |
16,189 - 45,667 |
0,001 |
IFN gamma Follow-up 1 |
14,714 |
|
|
|
Table 17 Paired T-test result of IFNγ level (n=14)
This research revealed that the residual or recurrent NPC patients who received PDT have higher life expectancy (60, 7%) compared to those who did not received PDT (22, 9%). It is important to note that the group of residual/recurrent NPC patients who received PDT had gone through a selection to fulfill the inclusion criteria for PDT, in which the tumor size in this group is less than one centimeter (<1cm) and if there is a lymph node metastasis. Therefore the clinical characteristics between PDT group and no PDT group might be slightly different. This difference could possibly affect the result of 5years life expectancy analysis on both groups. Even so, this research is managed to show that PDT could increase 5years life expectancy in residual or recurrent NPC patients.
The analysis result of prognostic factors affecting PDF success outcome showed that males have higher life expectancy (73, 5%) compared to the females (42, 2%). Residual or recurrent NPC patients who received PDT who are 40years old or younger (≤40 years old) has higher life expectancy (76, 2%) compared to those who are older than 40years old (53, 0%). From multivariate analysis on prognostic factors, it was discovered that male gender is one of the factors that takes effect in longer life expectancy of residual and recurrent NPC patients who received PDT.
There were elevation in cytokines’ levels; IL-12, IL-2, and IL-18, 90 days after PDT was administered in residual or recurrent NPC patients. Interleukin-12, which is a T-cell stimulating factor, was reported to be linearly raised after PDT administration until day 267 post administration. Interleukin-2 and interleukin-18 levels seemed to be declined after previously elevated on day 90th after PDT administration. IFNγ levels were found to come down in a linear pattern after administration of PDT until day 267th post PDT.
This research has a novelty aspect where it proves that PDT could enhance the life expectancy of residual or recurrent NPC patients, which is also attributed to the elevation of immune response proteins. This research also reports the pattern of immune response protein levels in period of 90 to 267days after PDT administration. Proven that 5years life expectancy of NPC patients who received PDT are higher than those who did not received PDT. A retrospective cohort method applied in this research provides an advantage in which the immune response proteins’ level could be observed from time to time. The weakness of this research is the execution of immune response proteins’ level measurement, which was done after the samples had been stored for quite a ling time in laboratory. Also, the absence of complete clinical data collection for NPC patients who received PDT causing the inability to analyze the clinical impact of the elevation or devaluation of immune response protein levels to the clinical manifestation of the patients.
This research completes previous other research done by Mroz et al.,10 reported that PDT which brought up a great inflammatory response were able to activate steady state DC that tolerates into immunogenic activated DC. The activation was marked by the elevation of MHC and costimulator molecules, or cytokine products level such as IL-12, IL-18, and interferon.10
Interleukin-12 is a cytokine produce by human dendrite cells, macrophages and lymphoblastoid B-cells. Interleukin-12 takes place in naïve T-cell differentiation into Th1 lymphocytes so then this cytokine is called as T-cell stimulating factor. Interleukin-12 also stimulates the production of IFNγ and Tumor Necrosing Factor Alpha (TNFα) by T-cells and NK cells. Interleukin-12 also plays an important role in T-cells and NK cells activity by increasing the cytotoxic ability, also has antiangiogenic activity through the elevation of IFNγ production.
Interleukin-18 also called Interferon-γ Inducing Factor. Interleukin-18 is a part of superfamily IL-1 and was produce by macrophages and some other cells. IL-18 works by bonding with IL-18 receptors and along with IL-12 induce cellular immunity (cell-mediated immunity) and activate T-cell proliferation. It is mentioned that IL-18 is capable of activating immune response without the help of IL-12, also induce NK cells proliferation, where specifically IL-12 will up regulates Perforin Mediated Cytotoxicity on NK cells.
Interferon Gamma (IFNγ) is a cytokine produced by lymphocyte, by some researchers it is classified as lymphokine. IFNγ classified in type II interferon or immune interferon. IFNγ is a cytokine that’s crucial for natural and adaptive immunity against viral infection, intracellular bacterial infection, and as a control against tumor. IFNγ works as macrophage activators, its importance in immune system mostly based on its ability to inhibit viral proliferation directly, also in immunostimulation and immunomodulation effects.11
This research is using retrospective cohort method where samples used for the immune response marker cytokines level measurement had been stored in laboratory for a relatively long period of time. Although the sample storage was done properly, most serum stored could not be measured for the lack of volume and the scattered sampling collection moments. As a consequence to this matter, only 14 samples out of 31 samples could be measured. This major limitation in serum samples is also one of the weaknesses of this research. It is suggested to do this research using prospective cohort method to collect more samples with less scattered sampling collection moments. Going forward, it is expected to be able to do a deeper and more specific research on systemic immune response of NPC patients who received PDT, also an analysis on clinical impact of the immune response level measurement needs to be done in the future.
The result of PDT on residual or recurrent NPC patients after radiotherapy of chemo radiation that was evaluated locally based on nasopharynx biopsy showed gratified result. This result is better compared to re-radiotherapy or even brachytherapy. After long period observation, it was reported that residual or recurrent NPC patients who received PDT have 5years life expectancy greater than those who did not receive PDT.
The analysis of prognostic factors in PDT that include gender, age, nasopharynx biopsy, and clinical stages were performed and revealed that male and age 40years old and younger each took effect in life expectancy result. Elevation of immune response cytokines of IL-12, IL-2, and IL-18 were found in residual and recurrent NPC patients who receive PDT 90days after the administration. Interleukin-12 was reported to elevate linearly after PDT administration until 267days later. IL-2 and IL-18 were seemed to devaluate after previously rising on 90days after PDT administration. Interferon-γ levels also devaluated after PDT administration until 267days later.
None.
Author declares there are no conflicts of interest.
None.

©2016 Indrasari, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.