Journal of
eISSN: 2379-6359


Case Report Volume 10 Issue 5
1Department of Otolaryngology–Head and Neck Surgery, University of Kansas Medical Center, USA
2Department of Otolaryngology, St. Luke’s Hospital, USA
Correspondence: Vusala Snyder MS, University of Kansas Medical Center 3901 Rainbow Blvd Mailstop #3010 Kansas City, KS 66160, USA, Tel 913-634-0825
Received: September 03, 2018 | Published: October 10, 2018
Citation: Snyder V, Le T, Wood V. Atypical presentation of pyomyositis in a young immunocompetent male with history of prior neck trauma: a case report. J Otolaryngol ENT Res. 2018;10(5):285-287. DOI: 10.15406/joentr.2018.10.00363
Background: The differential diagnosis for a neck mass in an adult can be broad. Often, we focus on the most obvious causes, including malignant or congenital causes. We present an unusual manifestation of neck swelling, specifically pyomyositis in an adult male with history of remote blunt neck trauma.
Case presentation: An otherwise healthy 22-year-old African American male presented with a 3-month history of progressive left-sided neck swelling and pain refractory to antibiotics and steroids. Aside from type B constitutional symptoms, he had sustained blunt trauma to the area 3 months prior. An extensive work up, including blood work, core needle biopsy, and imaging, was performed. Ultimately patient underwent an incisional biopsy, which demonstrated inflamed muscle and Staphylococcus epidermidis and Propionibacterium acnes on wound culture. Postoperatively his pain and swelling improved significantly and he has not had recurrence of symptoms.
Conclusion: Pyomyositis is a bacterial infection of skeletal muscle with unclear pathogenesis but can progress to affect large muscle groups. Commonly seen in tropical countries or in immunocompromised individuals, it is a relatively rare diagnosis in temperate countries like the United States. It is not usual for initial presentation to be in the purulent stage of the infection, which can persist for several months prior to forming an abscess.
This case demonstrates an atypical presentation of pyomyositis on many levels. The uncommon cervical musculature involvement, unusual bacteria cultures, competent immune system, and the involvement of prior neck trauma demonstrates the complexity in diagnosing and treating of this uncommon cause of a neck mass in an otherwise healthy adult male.
Keywords: pyomyositis, neck trauma, immunocompetent, neck infection, abscess
Pyomyositis (also known as pyogenic myositis, tropical myositis, etc.) is a primary skeletal muscle infection that was initially thought to be limited to tropical areas.1 Since the 1970s, an increasing number of cases have been described in temperate areas–the majority of them in association with immunosuppressed states such as HIV infection, organ transplantations, chemotherapies and rheumatologic diseases.2 Pyomyositis is a rare entity with cervical musculature involvement occurring 0.5-4% of the time, usually following dental or tonsillar trauma.3
A 22-year-old African American male with no pertinent past medical, surgical or social history, presented to the emergency department with a 3-month history of progressively worsening left-sided neck swelling and pain. He had sustained blunt trauma to the neck just prior to the start of his symptoms. He was treated with a round of amoxicillin followed by steroids as an outpatient with minimal improvement in his symptoms. He eventually presented to the emergency department (ED) when the pain was significant enough to restrict his neck range of motion. Other associated symptoms included fevers, malaise, night sweats and a 30 pound weight loss. At presentation to the ED, he was noted to have a fever of 101.3 F and a large indurated, erythematous left neck. On exam, the area was tender to palpation and crossed from the anterior midline neck to the left posterior neck and down the left clavicular area. No fluctuance was appreciated. Neck range of motion was severely limited, particularly with head turn to the left. Flexible fiberoptic laryngoscope showed slight airway deviation to right with no other abnormalities. Work up demonstrated leukocytosis with a left shift and CT scan showed a large left neck mass causing slight airway deviation to the right with no obvious abscess formation (Figure 1A) (Figure 1B). MRI imaging demonstrated an enlarged contrast-enhancing left sternocleidomastoid mass extending medially to involve the left parapharyngeal space, visceral space, and left retropharyngeal space at the level of the thyroid cartilage (Figure 1C) (Figure 1D). Given the type B constitutional symptoms suggestive of an infectious process versus malignancy, empiric IV antibiotics (vancomycin, zosyn, and unasyn) were initiated. An ultrasound guided core needle biopsy was performed which was inconclusive. Quantiferon and HIV tests were negative. Given the lack of a diagnosis, decision was made to perform an incisional biopsy under general anesthesia on hospital day 5 at which time there was a central area of spontaneous seropurulent drainage. Incisional biopsies of the sternocleidomastoid muscle and cultures of the drainage were obtained. Surgical pathology demonstrated skeletal muscle and fibrous tissue with dense suppurative and chronic inflammation, suggestive of a reactive or inflammatory process. There was no evidence of malignancy. Cultures were consistent with Staphylococcus epidermidis and Propionibacterium acnes. Constellations of findings were suggestive of pyomyositis. The patient’s symptoms improved and he was discharged on day 10 with oral antibiotics. Patient did not return for his follow up appointments however he did endorse dramatic resolution of his swelling and symptoms by phone.
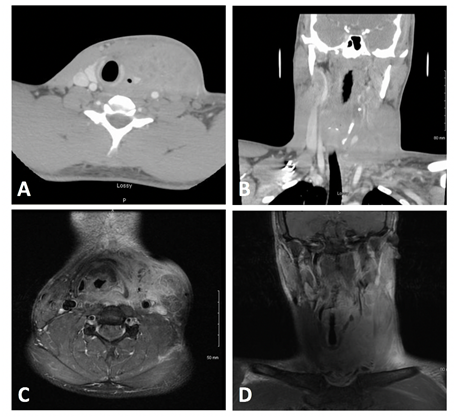
Figure 1 Complex 4.6 x 7.4 x 7.2 cm centrally necrotic enhancing mass centered about the inferior left sternocleidomastoid muscle causing slight airway deviation to the right. MRI shows mass extending medially to involve the left parapharyngeal space, visceral space, and left retropharyngeal space at the level of the thyroid cartilage. A) Axial CT B) Coronal CT C) Axial MRI D) Coronal MRI.
Pyomyositis is an acute bacterial infection arising from hematogenous spread, often without an obvious local source of infection and can subsequently result in abscess formation within skeletal muscles and sepsis.3 Larger muscle groups such as quadriceps, gluteal, and iliopsoas are most often affected, whereas involvement of neck muscles is very rare. The exact pathogenesis remains unclear; it is proposed to be a complication of transient bacteremia in a setting of muscle injury. The most common microorganism detected in blood cultures or surgical specimens from 90% of tropical cases and 75% of temperate cases is Staphylococcus aureus.2 Group A streptococci is the second most common organism implicated, whereas Staphylococcus, Bartonella and Salmonella species are the most common causative organisms in patients with HIV infection.4 It is more prevalent in young men, with a male-to-female ratio of 1.5:1, with the highest incidence peaking in middle age.4 Pyomyositis often presents subacutely, with a prodrome of low-grade fever and nonspecific aches and pain, prompting patients to seek medical advice five to six days after symptom onset. The clinical progression of disease consists of three distinct stages:
Stage 1–Invasive stage: characterized by local, insidious, progressive pain, low-grade fever, generalized malaise, and muscle aches. A microorganism invades a deep layer of muscle tissue via hematogenous or lymphatic spread, thus superficial physical findings are absent. This stage can last from 12 hours to a year, with a mean of 24 days, and accounts for only 2% of clinical presentations.5
Stage 2–Purulent stage: associated with destruction of muscle architecture, formation of deep abscesses, severe muscle pain, restricted range of motion, edema, and high-grade fevers. This stage accounts for approximately 90% of clinical presentations.5
Stage 3–Late stage: characterized by intense pain and systemic findings, including disseminated infection, septic shock, and multi-organ system failure due to undiagnosed/untreated purulent stage. Mortality associated with disease identified at this stage is 0.89-14%.5
Differential diagnosis for a neck mass is vast and can encompass a congenital abnormality, muscle strain, hematoma, malignancy, venous thrombosis, septic arthritis, osteomyelitis, and so on. High index of suspicion must be maintained since the early diagnosis is often missed since there is no suppuration in the early stages of the disease. Blood cultures are sterile in a majority of patients and wound cultures are inconclusive in up to 30% of cases. Therefore, muscle biopsy with culture is the gold standard to confirm the diagnosis and rule out similar diagnoses like polymyositis and intermuscular abscesses.2 Prior to incisional biopsy, it is important to rule out neoplastic processes if possible. Imaging is the best diagnostic modality, with computed tomography (CT) preferred over ultrasound to better delineate muscle structure and identify the extent of infection. Magnetic resonance imaging (MRI) remains the gold standard for radiographic diagnosis of pyomyositis because it more accurately characterizes diffuse inflammation and any subsequent abscess formation.3 Pyomyositis appears as diffuse muscle enlargement with increased signal on T2-weighted images. Occasionally, fluid collection within the muscle may be seen as hyperintense on T2-weighted images and isointense to hypointense on T1-weighted images.2,3 Gadolinium may reveal a rim enhancement of varying thickness in the abscess wall during the purulent stage.6
Treatment varies based on the stage of the disease at presentation. During the invasive stage, treatment consists of intravenous antibiotics for 2-4 weeks. Empiric antibiotics are initially recommended, with coverage for S. aureus and Haemolytic streptococci. If the underlying microorganism is identified, treatment can be guided by testing sensitivity. Surgical drainage of an abscess followed by antibiotic treatment is necessary for patients presenting in purulent stage.6
In summary, we present an atypical case presentation of pyomyositis. This unique case illustrates a purulent-late presentation after a non-penetrating trauma several months prior to symptom onset. CT scan findings demonstrated extravasation of air around the trachea, suggesting the possibility of airway perforation secondary to blunt trauma as the source of infection. The uncommon cervical musculature involvement, unusual bacteria, and history of trauma, makes this case an interesting look at a challenging diagnosis of an infection that although rare, is increasing in the United States. In a patient presenting with a neck mass, trauma with secondary infection is something to consider as an etiology. Prompt recognition and treatment can result in rapid resolution of the infectious process and decrease patient morbidity.
This work was supported by the Department of Otolaryngology, University of Kansas Medical Center and Department of Otolaryngology, St. Luke’s Hospital.
The authors declare no conflicts of interest.

©2018 Snyder, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.