Journal of
eISSN: 2379-6359


Case Report Volume 8 Issue 6
1Department of Otorhinolaryngology Hospital Sultanah Nur Zahirah, Malaysia
2Department of Otorhinolaryngology Head Neck Surgery School of Medical Sciences Universiti Sains Malaysia Health Campus, Malaysia
Correspondence: Irfan Mohamad Department of Otorhinolaryngology Head Neck Surgery School of Medical Sciences Universiti Sains Malaysia Health Campus Kota Bharu Kelantan, Malaysia, Tel 609-7676420
Received: July 24, 2017 | Published: October 13, 2017
Citation: Ibrahim F, Ghazali L, Abdullah K, Mohamad I (2017) Hemorrhagic Vallecular Cyst as a Rare Cause of Odynophagia. J Otolaryngol ENT Res 8(6): 00267. DOI: 10.15406/joentr.2017.08.00267
Vallecular cysts are usually asymptomatic but they may present with obstructive or irritative symptoms depending on the size at presentation. It is a benign curable disease. The common symptom includes foreign body sensation in the throat, or even dysphagia. We report a case of a healthy young gentleman who presented with sudden onset of odynophagia, which upon diagnostic laryngoscopy showed an intralesional bleeding of a vallecular cyst. After the computed tomography scan confirmed the lesion was no highly vascularized, endoscopic excision was performed. The symptom relieved immediately after the surgery.
Keywords: cyst, vallecula, hemorrhage, odynophagia, lymphoepithelial cysts
Vallecular cysts are retention cysts of the minor salivary glands in the vallecula and base of tongue.1 They have been classified as ductal cysts, retention cysts, and lymphoepithelial cysts. Inflammation, irritation and trauma are the known etiology of the lesion.2 Differential diagnosis of the vallecular cyst include hemangiomas, lymphangiomas, teratomas, dermoid cyst, lingual thyroid and the internal thyroglossal duct cyst.3 The patients usually asymptomatic or presented as odynophagia. In an extremely rare occurrence, a sudden increase in size for example in an intralesional bleeding cyst may manifest as an acute symptom of odynophagia.
A 29-year-old healthy gentleman was referred from the emergency department after he experienced sudden onset of odynophagia during dinner. The patient thought it was a stucked fish bone. He had no history of dysphagia or airway problem. Bedside laryngoscopy examination revealed a large hemorrhagic cystic lesion occupying right valleculla (Figure 1). Considering the differential diagnosis of oropharyngeal hemangioma however revealed a normal oral cavity, oropharynx, glottis and supraglottic structures. There was no evidence of foreign body either. Blood investigation was normal.

Figure 1 A cystic mass with bluish discoloration seen on endoscopy, indicating intralesional hemorrhage.
Urgent computed tomography (CT) scan of neck confirmed the presence of a cystic lesion arising from right vallecula measuring 3.1cm x 2.7cm x 1.9cm, compressing epiglottis the posteriorly and causing slight obliteration to the oropharynx (Figure 2). No radiographic evidence of foreign body seen.
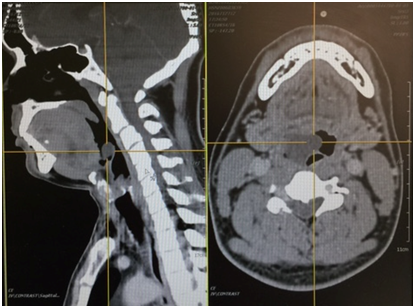
Figure 2 CT scan confirmed the localized well delineated fluid-contained mass in the right vallecula, as identified on the sagital and axial cuts.
As odynophagia persisted, patient was planned for a diagnostic rigid laryngoscopic examination and excision of cyst under general anaesthesia. The nasotracheal intubation process was uneventful. The intubation was performed by the senior airway anaesthetist with the aim not to disrupt the cyst architecture.
Intraoperatively, the cyst was seen to appear bluish in color. Under endoscopic guidance, it was completely excised using cold instruments (Figure 3). The appearance was suggestive of an acute hemorrhagic event had occurred within the cyst earlier. No foreign body was seen in the larynx and oesophagus.
He was symptom-free during immediate post operative period. He was tolerating orally well and was discharged home on the next day. A repeat laryngoscopy two-week after showed that operation site has completely healed. As per logistics reasons, he requested to continue follow up in another hospital. We advised him to adhere to the follow up schedule as the lesion is known to recur.
Several theories for the pathogenesis of vallecular cysts have been postulated. The most acceptable is as a result from obstruction of mucous glands at the base of the tongue. The cysts histologically are lined with mucous glands. It will gradually increases in size with time as the glands continue to secrete the mucous content.4 At any point, spontaneous bleeding in the cyst may occur, and rapid expansion of the size is expected. The condition will produce acute symptoms, as observed in our case.
Cysts of the vallecula are rare, accounting for 10.5% to 20.1% of all laryngeal cysts. The incidence of vallecular cysts on laryngoscopy has been reported as 1 in 1,250 to 1 in 4,200.5 It can occur at any age even though higher incidences in the fifth and sixth decades are observed. It has no gender predilection. The most common location of epiglottic cyst is lingual surface of the epiglottis.6
They are usually asymptomatic but there are also possible symptoms that may presented such as stridor, cough, dysphonia, foreign body sensation, hoarseness, and dysphagia. For infant, it may cause stridor, failure to thrive, respiratory distress or even life-threatening airway obstruction. Infection of the cyst may spread to the surrounding structures and cause edema and inflammation.7,8
The main investigative tool in diagnosis of a vallecular cyst is by direct laryngoscopy as the presence of the lesion can be confirmed and the degree of airway compromise can be assessed. Plain radiograph is almost useless owing to the nature of the lesion, thus CT or MRI does provide helpful extra information particularly for confirmatory diagnostic and intervention planning.9
The treatment modalities of management in vallecular cyst disease include simple draining of the cyst by puncture, marsupialization of the mucosa, or excision to achieve complete removal of the cyst. Follow up is warranted for the patient as disease recurrence is still a possibility regardless how complete the surgery was thought.
The literature and data sources were explored with the assistance of librarian Ms Purvi Nirmal (MLiSc) of Gujarat Adani Institute of Medical Sciences. Discrepancies of data were discussed with Dr. Narendra Hirani (M.S.) and Dr. Chandrasekhar Ranade (M.S.) faculties in the E.N.T. department of Gujarat Adani Institute of Medical Sciences. Levels of evidence and other biostatistics matter were discussed with biostatistician Dr Ajay Pathak (PhD) of P.S.M department of P. S. Medical College.
Author declares there are no conflicts of interest.
None.

©2017 Ibrahim, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.