Journal of
eISSN: 2379-6359


Review Article Volume 7 Issue 1
Otorhinolaryngologist Asir central Hospital, Saudi Arabia
Correspondence: Ibrahim Sumaily Otorhinolaryngologist Asir central Hospital Abha KSA, Saudi Arabia, Tel +966504621902
Received: April 11, 2017 | Published: May 2, 2017
Citation: Sumaily I (2017) Current Approach to Cerebrospinal Fluid Rhinorrhea Diagnosis and Management. J Otolaryngol ENT Res 7(1): 00191. DOI: 10.15406/joentr.2017.07.00191
Cerebrospinal fluid (CSF) rhinorrhea clinical approach and therapeutic techniques are rapidly growing and the literature is almost daily enriched with new studies, techniques, and trials. In this article I tried to collect, summarize and organize the updates on this topic from the English literature, and deliver it in a clinical approach manner with suggested algorithm and clarifying illustration so it can be easily understood by the readers and applied by those who are dealing with such cases.
CSF Rhinorrhea is defined as the presence of CSF within the nasal cavity as a result of abnormal communication between the subarachnoid space and the extracranial space. See Figure 1. This communication can be as a result of each of the following:
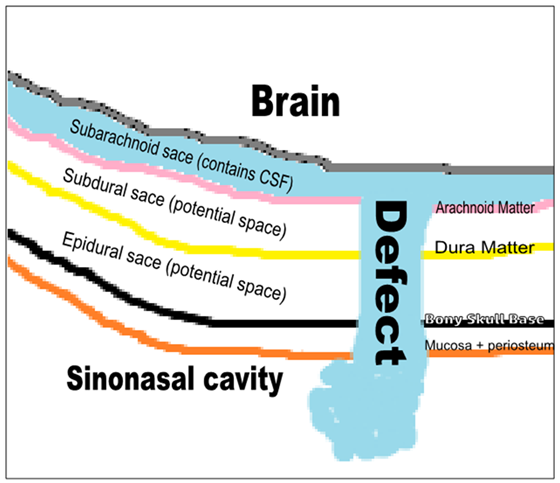
Figure 1 Content of the anterior skull base and the defect site where CSF leaks to sinonasal cavity.
Clinical
Laboratory
Imaging
This can be classified into primary and secondary:
Primary (helpful in the detection of most of the leaks).10,11
Secondary (useful if primary modalities failed to show the site of the leak):12
Radionuclide cisternography by radioactive isotopes (indium-111 (111In)) injection either into the lumbar or suboccipital subdural and nasal pledgets in various high-risk areas. Head scans are acquired 2, 6, 12, and 24 hours. And follow-up scans after 48- or 72-hours. It is useful in the detection of intermittent CSF fluid leaks with sensitivity range of 50 to 100%, and specificity 100%. It is relatively poor in exact localization, therefore it is reserved for complex cases when the diagnosis is in question.24
Management
Management can be classified as conservative and interventional:
Intracranial approach
70 to 90% success rate. Combined intracranial extradural and intradural approach allows the visualization and repair of the entire anterior skull base. The intracranial approach is indicated in the following conditions:2,28‒30
CSF leak is severe, recurrent, or not amenable to the endoscopic treatment.
Extracranial approaches
Preparations
Use navigation.44 30cm length scope is better. If using intraoperative fluorescein, a blue filter for the light source may aid in the identification of the defect. The mucosa is completely stripped away from the defect for at least 5mm in all the directions. Encephaloceles need to be reduced by using bipolar electrocautery at the stalk. Several Graft materials can be used; cartilage, bone, mucoperichondrium, septal mucosa, turbinate, fascia, abdominal fat, conchal cartilage, free tissue, pedicle tissue or composite grafts. The uses of the various types of graft materials do not seem to alter the outcome.4,45,46,47 Different ways of applying the graft; Bathplug see (Figure 3) where a fat plug with a specifically secured vicryl suture into the intradural space,48 Composite mucochondrial flap, for larger defects,49 Middle turbinate, composite bone/mucosa, for moderate and large defects,42 Inferior turbinate graft for defects > 2cm.50
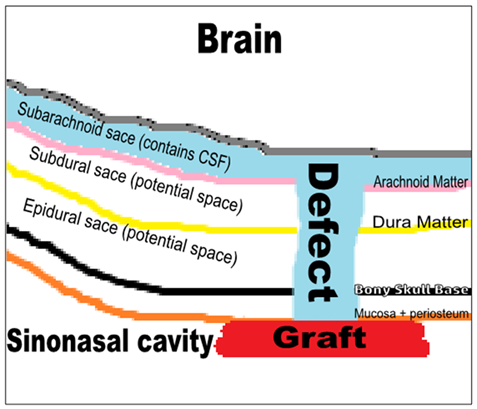
Figure 4 Overlay technique, where the graft is applied as a lining for the roof of the sinonasal cavity.
Either Overlay where the graft is applied within the nasal/sinus cavity to seal the defect or underlay where the graft is applied beyond the skull base. In the underlay technique it can be either epidural or intradural, where the results are almost equal but the intradural technique is relatively difficult. If the dura is widely opened and massive intraoperative CSF leakage is encountered, direct suturing of the dura is better.52,53,54 Nowadays sandwich technique, by combining intradural and extradural grafts, is the trend among the experts and seen to adds more security to the sealing of CSF and augments the results of repair.55 Laser tissue welding is an experimental technique that has been found to create an above-average-strength seal without significant inflammatory sequelae.56 Tissue sealants to add stability to a multilayered repair. Apply gel foam between the graft and the nasal pack. Remove the pack in 3-5days. Tissue glue can obviate the need for packing.57 Bed rest 3-5days with head elevation and antibiotic is recommended.
Adjuvant Technique, lumbar drain: Not in all cases.58 Useful in cases of frontal and sphenoid sinus defects with or without meningocele or encephalocele,59,60,61 and in those with high ICP. It can be kept for 3-5days.
Complications of endoscopic techniques include meningitis (0.3%), brain abscess (0.9%), subdural hematoma (0.3%), smell disorders (0.6%), and headache (0.3%). These possible complications are much less when compared to Craniotomy.60
The recurrence of CSF rhinorrhea occurs in up to 50%.62 Causes include spontaneous CSF rhinorrhea, elevated body mass index, extensive skull base defects, middle age, female gender, diabetic patients, in cases of multiple leaks, those with high intracranial pressure.63,64,65 Frontal sinus leak and the lateral sphenoid leaks repair have the highest failure rate (44%).66 In order to prevent recurrence, exact localization of the defect and proper technique, graft choice and Differentiating between high and low flow leaks are essential.67‒70 Also, early detection of high ICP, (20 cm H2O), and applying a lumbar drain will decrease the risk of recurrence.71 Prophylactic universal sellar reconstruction in cases of pituitary surgery found to decrease the risk of recurrence.72,73
CSF rhinorrhea71‒77 most commonly due to trauma where conservative measures are useful and the chance of spontaneous healing is high. In cases of iatrogenic and spontaneous leaks, it is less likely to heal with conservative measures. So, treating these cases early is recommended to prevent life-threatening sequelae. Beta-2 transfer in is the gold standard in the diagnosis of a CSF leak. MRI with FLAIR sequence is very useful and specific diagnostic and localizing technique without risk of contrast or radiation exposure, and therefore can be the first single diagnostic79 modality. Endoscopic management is the most useful approach for most of the cases. Conservative80‒82 measures are advised to be utilized postoperatively for most of the cases to avoid failure, which is commonly attributed to inadequate exposure intraoperatively and non appropriate care postoperatively.
None.
Author declares there are no conflicts of interest.
None.

©2017 Sumaily. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.