Journal of
eISSN: 2379-6359


Case Report Volume 6 Issue 3
Private Practice, India
Correspondence: Lanka Mahesh Private Practice New Delhi S 382 Panshila Park New Delhi 110017, India
Received: January 25, 2017 | Published: March 27, 2017
Citation: Mahesh L, Narayan T, Shukla S (2017) Histologic and Tomographic Clinical Report with 13 Years Follow-up of Sinus Augmentation through Caldwell Luc Procedure in a Case of Chronic Sinusitis. J Otolaryngol ENT Res 6(3): 00166. DOI: 10.15406/joentr.2017.06.00166
Aim: A case report discussing Caldwell Luc sinus augmentation as an adjunct for implant placement in the maxillary posterior and how to manage treatment with 8year clinical histological and radiological follow up.
Purpose: To evaluate the histologic and tomographic prognosis of sinus augmentation through a Caldwell Luc procedure.
Materials and Methods: A patient reported with RCT treated tooth with vertical fracture in 16, and long standing sinusitis. During sinus augmentation procedure, 16 was extracted, sinus was approached through the canine fossa, sinus lining was removed and the area grafted with Mineros (Biohorizons, AL, USA), alloderm membrane was placed over the void and passed through the mucosa in a pouch to cover the extraction socket. A Biohorizons external implant 4/15mm was placed after 8months and it was loaded after 6months.
Results: histologic and tomographic reports show excellent uptake of graft after eight months, and complete osseointegration between implant and bone interface.
Discussion: mucous lining has the property to grow itself within 4weeks after its complete removal. This property of the lining makes procedures like caldwellluc possible in which its removal can be done, also giving relief from diseases like long standing sinusitis. Bone grafting can also be done with such procedures, enabling increased height, ultimately making implant placement possible.
Conclusion: Implant placement in the maxillary molar area may be complicated due to enlargement of the maxillary sinus, crestal resorption due to periodontal issues, and resorption of the residual ridge or a combination of these factors. Osseous agumentation assists in creating a boney bed that can accommodate implant placement allowing utilization of implants in the posterior maxilla.
Keywords: caldwell luc procedure, sinus lining, bone grafting, augmentation, antrum, pneumatization, ostium
Implants and their use in dentistry have revolutionized surgical procedures and ridge augmentation procedures. When we consider implant placement in posterior maxilla, maxillary sinus and ridge height above it plays the most important role in prognosis of the implant placement. For poor posterior residual alveolar ridge, augmentation is the only method of choice. Although Tatum1 was first credited with augmentation of the maxillary sinus for implant placement, Boyne’s2 landmark paper described the use of autogenous bone grafting with long-term follow-up. From those initial investigations, many materials and techniques have become available to the surgeons, giving us better choices towards treatment planning for posterior maxilla with different graft materials. Although, presence of sinus poses a challenge in ridge augmentation procedures, also because sinus plays an important role in maintaining body’s physiology. Variable maxillary sinus bone graft-related complications, such as pain, infection, implant displacement into the sinus, bone loss, insufficient new bone regeneration, and oroantral fistula, lead to the failure of sinus bone grafting.3
Anatomy and physiology of the maxillary sinus
The maxillary sinus, or the antrum of Highmore, is usually the largest of the paired paranasal sinuses3. Each maxillary sinus has a volume of approximately 15 cc and is generally pyramidal is shape. The maxillary sinus is the 1st one to develop at the third month of the fetal life and has two growth phases. The first phase is called as the primary pneumatization process and the second as secondary pneumatization process. Postnatally growth continues rapidly with 3 growth spurts: from birth to 2.5years, from 7.5 to 10years and 12 to 14years.4,5 Maxillary sinus has a horizontally pyramidal shape that consists of a base, apex and 4 sides. The base comprises the vertical lateral wall of the nasal cavity, whereas the apex is at the junction of the maxillary and zygomatic bones, in some instances, when the sinus is large the apex may extend into the zygoma. The remaining 3 walls of the sinus make the superior, anterior and posterior walls of the sinus.
The superior wall makes up the roof of the sinus, which is also the floor of the orbit. The anterior wall forms the facial portion of the maxillary bone. The posterior and lateral walls blend together to form the posterolateral wall of the sinus which separates it from the infratemporal fossa and forms the maxillary tuberosity and pterygoid fossa.6 The average dimensions of the sinus are 28-33mm in height, 23-25mm in width, and 32-34mm in anterior-posterior length.7 The floor of the maxillary sinus usually is directly above the three posterior maxillary molars, although the sinus floor may extend to the apices of the premolars and also, but rarely, to the canine. The sinus may ‘‘invade’’ the alveolar bone surrounding the roots of the posterior maxillary teeth, where it may pose a surgical hazard when extracting teeth in this area. The formation of septa (i.e, Underwood’s septa), both complete and incomplete, within the sinus is often noted. Velasquez-Plata and colleagues8 reported presence of septa as revealed by computed tomogram in 24% of the sinuses in 156 patients. There are 4 types of maxillary sinus, depending upon the shape the can be classified as: semi-ellipsoid (15%), parabloid (30%), hyperbolic (47%), cone shaped (8%).9
The anterior superior alveolar, infraorbital, and posterior superior alveolar nerves and arteries provide both the innervation and blood supply to the sinus. The maxillary ostium provides drainage of the sinus and egress of mucous and lymphatic fluid into the nasal cavity. The ostium is located on the highest and most medial aspect of the sinus wall. The ostium drains into the semilunar hiatus of the middle meatus of the nasal cavity. In a septated sinus, accessory ostia are usually found to facilitate drainage of the separated compartments.5,6
There are many theories regarding the function of the paranasal sinuses, however, none are widely accepted.10 According to these postulations, the physiologic functions of the paranasal sinuses include decreasing skull weight; providing vocal resonance; improving olfaction; adding humidity to air to keep tissues in the nose, mouth, and throat moist; and regulating intranasal pressure.
The sinus is lined by a thin, ciliated mucous membrane of respiratory mucosa. These cilia beat at the rate of 1000 strokes/min11 and move the overlying mucous blanket toward the ostium rapidly at a rate of approximately 6 mm per minute, helping to overcome its relatively nondependant drainage position.12 In addition to removing particulate matter from the sinus, the mucous blanket also acts to prevent desiccation of the tissues.
This sinus lining has a very high and rapid regenerative capacity after trauma or surgical removal.13 Experimental operative removal of mucous lining in rabbits show regeneration and reepithelialization within 2 weeks, however such regeneration is never complete and results in sparse goblet cells, atypical glands and occasional polyp formation.14
Sinus augmentation procedure
Gillies & Rowe15 first demonstrated that bone graft could be placed against the sinus wall during osteotomies during the midface and since then sinus augmentation has become a common procedure. There are various methods available for maxillary augmentation from simple to aggressive procedures. Selection of the method depends upon the condition of the ridge. Le Fort I osteotomy, direct sinus lift, indirect sinus lift and Caldwell Luc operation are some of the widely used procedures for augmentation.
In the Caldwell Luc procedure, the surgeon gains access to the inferior aspect and floor of the sinus via a lateral approach. A 3-cm incision centered over the canine tooth and first premolar while leaving about 0.5-1cm of gingiva intact above the dentition to facilitate closure is given. Using a periosteal elevator, periosteum is elevated from the anterior wall of the maxilla. Care is taken to identify and avoid injury to the infraorbital nerve in the canine fossa. Mallet and osteotome, is used to enter maxillary sinus through its anterior thin bone. Thereafter, rongeurs are used to enlarge the opening, maxillary wall is then either fractured medially off a superior ‘‘hinge’’ or pushed bodily into the sinus. The mobilized lateral maxillary wall segment forms a ‘‘roof’’ under which grafting can proceed along the maxillary sinus floor as necessary. Dental implants can be placed simultaneously with this procedure, fixtures. However, primary stability of the implants requires approximately 4 mm of bone height. In the severely atrophic maxilla (i.e, <4mm of bone height), consideration must be given to a staged approach where the bone graft is allowed to consolidate before the dental implants are placed.16
The most critical step and the most common complication in any sinus augmentation procedure is the perforation of mucous lining of the maxillary sinus (Table 1). Though it has a high regenerative capacity after trauma or surgical removal, Almost care should be taken not to perforate the lining, mucous lining can regenerate within 2weeks after its complete removal. Reconstruction of bony sinus goes against the basic surgical principals of always having soft tissue coverage on all sides of the graft and implant. All grafts or implants used for reconstruction of the sinus walls are left exposed to the open sinus17 and this raises the question of graft’s or implant’s prognosis, but today with variety of grafts (autografts, xenografts, allografts) available this can be answered and assured with 100% success. There are various materials used for grafting which show excellent uptake through the host body, making implant placement possible in big three dimensional defects. Autogenou bone, Deproteinized sterilized bovine bone, Hydroxyapatite, Demineralized freeze-dried bone(DFDB), freeze-dried bone(FDBA), b Tricalcium phosphate are few of the examples of bone grafts available.18,19 Animal and human clinical research has shown that DFDBA powder used alone does not give good results, also when placed in an area of low oxygen tension, the material forms fibrous or cartilage tissue rather than bone.19
Type of Perforation |
Description |
Method of Repairing |
Instruction on Implant Placement |
Type I |
Produced in the most apical part of the window |
They seal spontaneously but a collagen membrane may be placed |
Continue with the sinus lift. It is possible to place simultane-ous implants |
Type IIA |
Produced along the lateral or coronal walls of the window. The sinus extends 4 to 5 mm proximal to the perforation |
Enlarge the osteotomy until in-tact membrane is exposed. If the perforation is smaller of 3 mm, it is sealed with a collagen tape, and if larger than 3 mm, a synthetic membrane or a resorbable membrane of porcine origin is placed |
Continue with the sinus lift. It is possible to place simultane-ous implants |
TYPE IIB |
Differs from the above is based of the perforation which is located at the limit of the maxillary si-nus, therefore the osteotomy can membrane |
A resorbable membrane is placed so that its limits extrude around the bone around the preparation |
Continue with the sinus lift. It is not possible to place simulta-neous implants |
Type III |
Produced in any part within the window extension |
A resorbable membrane is placed so that its limits extrude around the bone around the preparation |
Continue with the sinus lift. It is not possible to place simulta-neous implants |
Table 1 17Shows Types of Perforations and Methods of Repairing
A 28year old male patient reported to the clinic. The patient had RCT treated, vertical fracture in relation to the maxillary right first molar and long standing sinusitis(Figure 1). Vertical fracture took place due to incomplete procedure of crown placement. Sinus augmentation through Caldwell luc approach was decided as the treatment plan. Permission from the otolaryngologist was taken and patient was described about the procedure. A written consent was taken for the same. Radiographs were taken. Typically the radiographic finding of chronic sinusitis is nonspecific and variable. Findings include mucosal thickening or pacification and polyposis. Classically the bone is remodeled and thickened secondary to osteitis.20 None of these features were visible on the radiograph taken for this patient, however, clinical history demonstrated long standing sinusitis. Following administration of local anesthetic a crestal incision was made after extraction of the first maxillary molar and a full thickness flap was elevated. The sinus was approached through a Caldwell Luc procedure, wherein an osseous window was created to access the sinus, and the sinus lining was completely removed(Figure 2 & 3). A piece of Alloderm, an alloplastic connective tissue membrane was prepared following the manufacturers instructions by rinsing in sterile saline(Figure 4). The membrane was then placed into the sinus to act as barrier to contain the osseous graft material(Figure 5). The sinus was then packed with 3 cc Grafton (DBM Putty) graft material was placed into the sinus. Wound site was sutured using alloplastic sutures.
A radiograph was taken to verify osseous maturation of the sinus graft at four months post augmentation(Figure 6 & 7). Clinically the ridge presented with a wide dimension between the buccal and palatal plates maintaining adequate space for implant placement. A Biohorizon 4mm x 15mm external hex threaded implant was then placed and allowed to integrate over a 5month period unloaded. Following the integration period the implant was restored with a stock abutment and cemented porcelain fused to metal crown. Five years following the extraction, sinus augmentation, placement of implant and restoration the implant demonstrated maintenance of the bone both apically to the implant and crestally as viewed radiographically.
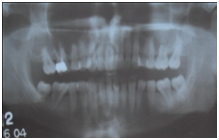
Figure 1 Preoperative radiograph demonstrating a failing maxillary molar that was previously endodontically treated.
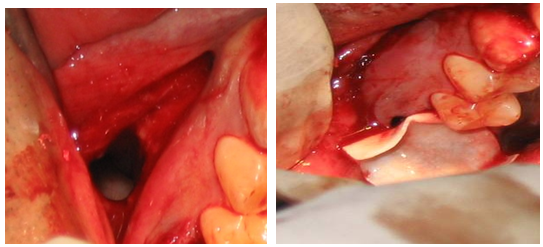
Figure 2 Complete removal of Figure 3 Alloderm placed over the diseased sinus membrane. Socket and passed over the osseous window then inserted into the sinus to act as a barrier to contain the graft.
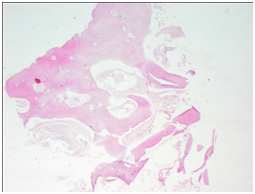
Figure 5 depicting a histological section of a core biopsy obtained during implant placement, stained with Hematoxylin & Eosin, showing good vascularized bone with no evidence of residual graft material (4X).
Post operative OPG shows excellent uptake of the graft, without interfering with the sinus lining. It also shows complete growth of the sinus lining over the graft material, making increased height of the maxillary ridge, appropriate for implant placement.
Maxillary sinus because of its anatomic position in the middle of the face and having a communication with the nasal channel gets injured and undergoes many histologic and pathologic changes. However it may remain asymptomatic in most of the individuals. With the extraction of maxillary teeth the upper posterior ridge collapses making any type of implant almost impossible to put without sinus augmentation procedure. The commonly done sinus augmentation procedure is direct sinus lift. But for the case presented in this article, Caldwell luk was opted as the choice of procedure due to long standing sinusitis, in which whole of sinus lining is removed, enabling it to regenerate. Mucous lining has the property to regenerate itself within 2weeks, even after its complete removal. There is lot of literature available on mucous lining and its complete regeneration after its removal along with experimental results. Knowlton & McGregor21 described the process of mucosal regeneration after its stripping in dogs. At 1month, ciliated epithelium began to grow, at 3months the lining had reformed almost completely and at 5months sinus was entirely lined by mucous membrane. According to Gorham & Bacher,22 clinical examination done on man’s mucous lining after its complete removal showed the cavity to be unevenly red at 2weeks, at 1 month small patches of glistening surface began to appear, after 3-5months the entire area was covered with glistening, pale pink surface.
Thus this surgical procedure served us with two purposes, first being complete removal of the lining, giving patient relief from sinusitis and enabling bone grafting for implant placement. Direct sinus lift, would have given us just the height and width if the maxillary ridge, without healing sinusitis of the patient. After removal of sinus lining through Caldwell luc procedure, sinus cavity becomes a big void just like any enlarged defect where graft can be incorporated. The sinus lining starts to grow above the graft within 2weeks without jeopardizing the normal functioning of the human body. As the graft matures and becomes host bone within 5months sinus floor has a new height and health restored where an implant can be placed, along with the new sinus lining. Usually during sinus augmentation the most common complication is the perforation of the sinus lining. If that occurs during direct sinus lift procedures, it is best advised to abort the procedure and renter after 4weeks when mucous lining grows back.
Implant placement in the maxillary molar area may be complicated due to enlargement of the maxillary sinus, crestal resorption due to periodontal issues, and resorption of the residual ridge or a combination of these factors. Osseous agumentation assists in creating a boney bed that can accommodate implant placement allowing utilization of implants in the posterior maxilla.
None.
Author declares there are no conflicts of interest.
None.

©2017 Mahesh, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.