Journal of
eISSN: 2379-6359


Research Article Volume 6 Issue 1
1Department of Clinical Neurophysiology Hospital Universitario Santa Cristina, Spain
2Department of Otorhinolaryngology Hospital Universitario Puerta de Hierro Majadahonda, Spain
3UAM Hospital Universitario La Princesa, Spain
Correspondence: Gabriela Goizueta San Martín, Neuromuscular Unit, Department of Clinical Neurophysiology, Hospital Universitario Santa Cristina, C/Maestro Amadeo Vives, 2-3, 28009, Madrid, Spain, Tel +34 915574432
Received: November 04, 2016 | Published: January 30, 2017
Citation: Goizueta San Martin G, Gorriz Gil C, Pinilla Urraca M, Barón Sanchez J, Fernandez Cuadros M, et al. (2017) Protocol for Neurophysiological Studies of the Superior and Recurrent Laryngeal Nerves and of the Cricothyroid and Thyroarytenoid Muscles. Clinical Utility. J Otolaryngol ENT Res 6(1): 00149. DOI: 10.15406/joentr.2017.06.00149
Objective: This study describes a protocol for laryngeal neurophysiological studies and presents reference values for motor nerve conduction with percutaneous stimulation (Electroneurography-ENG) and muscle function using laryngeal Electromyography (EMG).
Methods: We obtained motor nerve conduction values for 50 superior laryngeal and 12 recurrent laryngeal nerves using an external approach with percutaneous stimulation for both nerves. We also obtained normal values of the motor unit action potentials (MUAPs) of the twenty cricothyroid and the twelve thyroarytenoid muscles in healthy subjects and conducted a statistical analysis of mean.
Results: Mean latency of the superior laryngeal nerve was 1.67±0.25ms; mean amplitude of Potential Action Muscular Compound (CMAP) was 2.04±1.03mV. Mean Latency and amplitude of the recurrent laryngeal nerve were 1.66±0.14ms and 6.21±2.77mV, respectively. Mean duration of cricothyroid motor unit action potentials (MUAP) was 5.1±0.26ms, amplitude was 144.24±45.79μV. In the thyroarytenoid muscle: mean duration of MUAP was 5.13±0.22ms, amplitude 159.52±51.52μV and the interference pattern had an amplitude of 200-600μV for both
Conclusions: This survey of healthy subjects establishes laryngeal nerve and muscle reference values, which are essential for assessing anomalies at these locations.
Keywords: laryngeal electroneuromyography, study protocol, reference values, laryngeal disease, laryngeal nerve, neurophysiology
ENG, electroneurography; EMG, electromyography; MUAPs, motor unit action potentials; CMAP, potential action muscular compound; LENMG, laryngeal electroneuromyography; LEMG, laryngeal electromyography
Neurophysiological studies of the larynx using laryngeal electroneuromyography (LENMG), which includes electromyography (EMG) and electroneurography (ENG), are essential for assessing neuromuscular function and for differential diagnosis of voice alterations (dysphonia) secondary to specific laryngeal disease or to other more general processes affecting the larynx. Laryngeal disease can be caused by lesions to nerves (superior or recurrent laryngeal nerves), lesions to muscles innervated by those nerves, abnormalities in neuromuscular transmission, central nervous system alterations, or alterations in joints. Laryngeal electromyography (LEMG) was introduced by Weddell G et al.,1 LEMG was first used in the clinical setting by Faaborg-Andersen K, Buchthal F.2‒5 These authors studied motor unit action potentials.6‒11 Sawashima M et al.,7 and Sram F. and Kaldova E.12 were the first authors to report normal electromyographic findings in cricoarytenoid joint ankylosis. Faaborg-Andersen4 was the first researcher to describe and use this technique for diagnosing paralysis secondary to surgical nerve lesions; this observation was followed by those of others.3,5,7,12‒23
Other more general diseases able to affect the larynx include generalised muscle diseases with dysphonia as an initial symptom;24 motor neuron degenerative diseases, generalised peripheral neuropathies;25 myasthenia24,26‒28 and Central nervous system lesions which could lead to abnormal movements.12,29‒38
The direct route of access was used in earlier procedures; tracheostomy was sometimes used to introduce and place different types of electrodes in the throat6,39‒41 among others. The transcutaneous approach to the vocal cord through the cricothyroid membrane was introduced by Fink BR et al.,42 and subsequently used surface electrodes for electromyography by other.43‒45
The Neurophysiological examination of the larynx is increasing progressively, since it is clinically useful in diagnosing neuromuscular diseases. Nevertheless, the values of motor nerve conduction of laryngeal nerves are under-developed.
For these reasons, the purpose of our study is to present a protocol for neurophysiological studies of the larynx, to obtain normal motor nerve conduction values for the superior nerve (with surface registration in cricothyroid muscle) and recurrent laryngeal nerve (with a concentric needle electrode for registration on the thyroarytenoid muscle). The percutaneous stimulation for both nerves is a less aggressive technique that favours the neurophysiological exploration and is not commonly described. We also obtained normal values and evaluate motor unit action potentials and the recruitment pattern in the cricothyroid and thyroarytenoid muscles with transcutaneous insertion of the concentric needle electrode for both.
We studied 50 superior laryngeal nerves (36 unilateral and 7 bilateral subjects), 12 recurrent laryngeal nerves (9 unilateral and 3 bilateral subjects), 20 cricothyroid (15 unilateral and 5 bilateral subjects) and 12 thyroarytenoid muscles (9 unilateral and 3 bilateral subjects) in healthy individuals. The procedure began with researchers giving a detailed explanation of the test to be performed; all participants signed informed consent forms. Subjects remained in the supine position with cervical hyperextension (Figure 1), the percutaneous approach requires a concentric needle electrode, as in the present study. The EMG study of the cricothyroid muscle (Figure 2a), located on the anterolateral aspect of the cricoid cartilage, was performed by placing the concentric needle electrode above the cricoid cartilage and inserting the electrode in the cricothyroid muscle at an angle of 45°. The position of the electrode was confirmed by asking the patient to lift his or her head or move it laterally without speaking, and to phonate /e: on ascending and descending scales to analyse the recruitment pattern. For the thyroarytenoid muscle (Figure 2b), the concentric needle electrode was inserted through the skin and the cricothyroid membrane and then oriented at an angle of 20° laterally and 45° proximally (submucosa) to avoid entering the subglottal cavity. The patient was asked to phonate /e:/ several times. The muscle study analysed activity at rest, maximum effort (recruitment pattern), and 20 muscular motor unit action potentials (MUAPs) on each muscle (measuring mean duration, amplitude, and polyphasia).

Figure 1 Patient position for undergoing laryngeal ENG and EMG. The patient remains supine with the neck hyper extended.
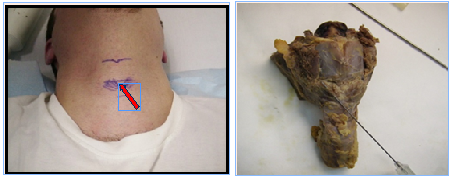
Figure 2a Direction of insertion of the concentric needle electrode for EMG. Cricothyroid muscle anatomical location.
The ENG of the superior laryngeal nerve (Figure 3a) was conducted using surface for percutaneous stimulation electrodes on the superior lateral area of the thyroid cartilage and record its activity (contraction of the cricothyroid muscle) with active surface electrode on the cricothyroid muscle and indifferent electrode on the clavicle. (The study can also be performed using a concentric needle electrode inserted into the cricothyroid muscle to record muscle activity). Activity in the recurrent laryngeal nerve (Figure 3b) is registered using a concentric needle electrode inserted in the thyroarytenoid muscle, along with a cutaneous stimulator placed on the lateral inferior area of the thyroid cartilage, the area just lateral to the trachea (between trachea and carotid artery). The distance between the point of stimulation and the recording electrode is 3cm for the superior laryngeal nerve. For the recurrent laryngeal nerve, the distance between the point of stimulation and the insertion point of the concentric needle electrode is also 3cm. (This distance does not reflect the exact route of the nerve but serves as a datum). The latency of the CMPA was acquired from point of electrical stimulation at the first evoked waveform deflection from the baseline in ms. A supramaximal stimulus was applied in all cases (10-15mA). The stimulus duration was 0.1ms. We also assessed the morphology, latency in ms, and amplitude (negative-peak amplitude) of CMAP in mV.
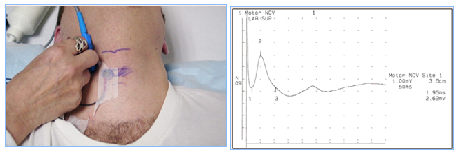
Figure 3a Electrode placement for ENG of the superior laryngeal nerve. Recording using a surface electrode on the crycothyroid muscle (reference electrode is placed on the clavicle). Cutaneous stimulator on the lateral superior edge of the thyroid cartilage. Example of CMAP.
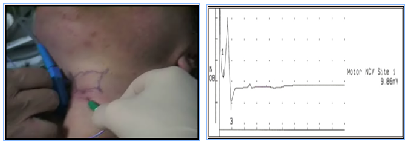
Figure 3b ENG of recurrent laryngeal nerve. Recording with concentric needle electrode on the thyroarytenoid muscle. Stimulator on the lateral
inferior edge of the thyroid cartilege. Example of CMAP.
Statistical study
A descriptive analysis and a comparative study for laterality is been performed to determine the normal values of electromyography and motor nerve conduction on laryngeal muscles and nerves. The numerical variables with 25, 50 and 75 median percentiles, minimum and maximum values, mean and 2.0 Standard Deviation (95%) were determined. The categorical variables were reported by absolute and relative frequency. In the descriptive analysis, to establish the normality of values on electomyography and nerve conduction motor studies, mean±2.0 Standard deviations (95.45%) were applied, by convention. Besides, theoretically, analysis should be computed at least on 50 healthy subjects. As the sample showed not normal distribution, the non-parametric test of Wilcoxon for paired samples, to evaluate the side-to-side difference, was used. The significance level was 95% with a α-error of 0.05, and a pos-hoc power analyses was performed. The Statistical package STATATM v. 14.1 was used.
The results of the nerve conduction study for the Superior Laryngeal nerve are shown in Table 1. This nerve was explored in 43 subjects (43 unilateral and 7 bilateral); 15 men and 28 women; aged 21 to 76years (median age: 50 years). Median latency of the superior laryngeal nerve was 1.77ms and median amplitude was 1.51mV. Table 2 shows the results of the nerve conduction study for the Recurrent Laryngeal nerve. Median latency was 1.62ms and median amplitude was 6.16mV. We studied the CMAP in 9 subjects: 9 unilateral and 3 bilateral (4 men and 5 women) aged 22 to 64 (median age: 52years).
Stats |
Age |
LAT-R ms |
AMP-R mV |
LAT-L ms |
AMP-L mV |
N |
43 |
50 |
50 |
7 |
7 |
p50 |
50 |
1.77 |
1.51 |
1.85 |
1.34 |
p25 |
41 |
1.45 |
1.31 |
1.58 |
1.31 |
p75 |
57 |
1.85 |
2.57 |
1.9 |
1.66 |
Min |
21 |
1.05 |
1 |
1.5 |
1.05 |
Max |
76 |
1.95 |
5 |
1.95 |
2.57 |
Table 1 Superior laryngeal nerve
Statistics (count median p25 p75 min max) Lat: Latency; AMP: Amplitude. Signification: Lat R-L: P=0.3173. Amp R-L: P=0.3105
Stats |
Age |
LAT-R ms |
AMP-R mV |
LAT-L ms |
AMP-L mV |
N |
9 |
12 |
12 |
3 |
3 |
p50 |
52 |
1.625 |
6.165 |
1.6 |
5.63 |
p25 |
47 |
1.55 |
4.71 |
1.5 |
5.14 |
p75 |
60 |
1.8 |
8.48 |
1.8 |
9.86 |
Min |
22 |
1.45 |
1.5 |
1.5 |
5.14 |
Max |
64 |
1.84 |
9.9 |
1.8 |
9.86 |
Table 2 Recurrent nerve
Statistics (count median p25 p75 min max) Lat: Latency; AMP: Amplitude. Signification: Lat R-L: P=0.3173. Amp R-L: P=0.5930
Normal values obtained for the parameters of the EMG study of the cricothyroid and thyroarytenoid muscles are shown in Table 3 and Table 4. The EMG study of the cricothyroid muscle was conducted in 20 muscles and 15 subjects: 15 unilateral and 5 bilateral (4 men and 11 women); aged 33 to 72 (mean age: 48years). Median duration of MUAP was 5.14ms, amplitude was 157.38μV and polyphasia was 1.05%. The EMG study of the thyroarytenoid muscle was explored in 9 subjects (9 unilateral and 3 bilateral) (4 men and 5 women) aged 22 to 64 (median age: 52years). Mean duration of MUAP was 5.15ms, amplitude was 148.8μV and polyphasia was 1.05%. The amplitude of the interference pattern was 200-600μV for both muscles.
Stats |
EDAD |
MD-R ms |
AM-R μV |
MD-L ms |
AMPL μV |
N |
15 |
20 |
20 |
5 |
5 |
p50 |
48 |
5.1 |
134.8 |
5 |
140.6 |
p25 |
40 |
4.95 |
115.85 |
4.9 |
124.4 |
p75 |
53 |
5.2 |
159.65 |
5.05 |
141.6 |
Min |
33 |
4.8 |
77.9 |
4.8 |
117.7 |
Max |
72 |
5.9 |
288 |
5.9 |
155 |
Table 3 Cricothyroid muscle
Statistics (count median p25 p75 min max). Polyphasia: 1.05%, MD: Median Duration; AMP: Amplitude. Signification: MD R-L: P=0.8759. AMP R-L: P=0.2763
Stats |
EDAD |
MD-R ms |
AMP-R μV |
DM-L ms |
AMP-L μV |
N |
9 |
12 |
12 |
3 |
3 |
p50 |
52 |
5.15 |
148.8 |
5.2 |
164.3 |
p25 |
47 |
4.97 |
12.55 |
5.1 |
114 |
p75 |
60 |
5.25 |
197.9 |
5.5 |
208 |
Min |
22 |
4.8 |
92.3 |
5.1 |
114 |
Max |
64 |
5.5 |
267 |
5.5 |
208 |
Table 4 Thyroarytenoid muscle
Statistics (count median p25 p75 min max). Polyphasia: 1%, MD: Median Duration; AMP: Amplitude
Signification: MD R-L: P=0.1655. AMP R-L: P=0.1088
Figure 4a presents an example of MUAP and Figure 4b shows the typical recruitment pattern of this muscle. The amplitude of the recruitment pattern and the MUAP parameters for the thyroarytenoid muscle are similar to those of the cricothyroid (Figures 4c and 4d).
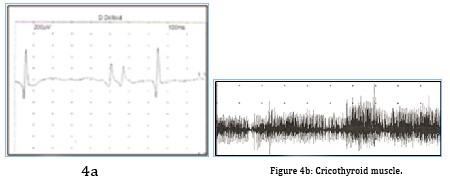
Figure 4 Examples of EMG results. (a) and (b) MUAP and recruitment pattern of the cricothyroid muscle. Maximum effort: phonation of /e/ on ascending and descending pitches.
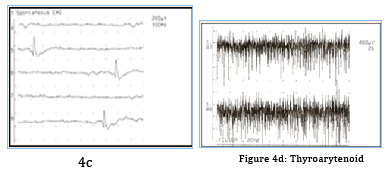
Figure 4 (c) and (d) MUAP and recruiment pattern of the thyroarytenoid muscle. Maximun effort: continuous phonation of /e/
In table 5, we present as a resume, the mean latencies and amplitudes (and their SD) of laryngeal superior and recurrent nerves. Besides, we present the mean duration and amplitudes (and the SD) of cricothyroid and thyroarytenoid muscles.
Nerve |
Latency (ms) |
Amplitude (mV) |
|
|
Mean ±SD |
Mean ±SD |
|
Laringeal Superior |
1.67±0.25 |
2.04±1.03 |
|
(N:50) |
|||
Recurrent |
1.66±0.14 |
6.21±2.77 |
|
(N:12) |
|||
Muscle |
MD (ms) |
Amplitude (µV) |
|
Mean ±SD |
Mean ±SD |
||
Cricothyroid |
5.10±0.26 |
144.24±45.79 |
|
(N:20) |
|||
Thyroarytenoid |
5.13±0.22 |
159.52±51.52 |
|
(N:12) |
|
|
|
Table 5 Resume
ST: Standard Deviation; MD: Median Duration; Ms: miliseconds; µV: microvolts
No significant age or sex differences were identified. There is no significant difference in the parameters evaluated in both sides. None of the patients developed complications during or after the test at the next follow-up.
The principal purpose of the present study is to present a protocol for neurophysiological studies of the larynx and it's clinical utility, to obtain normal motor nerve conduction values for the superior and recurrent nerves with surface registration for cricothyroid muscle and recurrent laryngeal nerve with transcutaneous insertion of the concentric needle electrode in thyroarytenoid muscle, and percutaneous stimulation for both nerves. We also obtained normal values and evaluate motor unit action potentials and the recruitment pattern in the cricothyroid and thyroarytenoid muscles with transcutaneous insertion of the concentric needle electrode for both.
For laryngeal studies, the position of the subjects can be performed in two ways. Subjects can be in the supine position with cervical hyperextension (Figure 1); or with patients just sited. We believe that the first position is easy to perform and well tolerated by patients. Explaining the procedure to patients before conducting the study and asking them to remain supine position with the neck hyperextended helps them feel more relaxed, which in turn facilitates performing the study.
The direct route of access was used in earlier procedures; tracheostomy was sometimes used to introduce and place different types of electrodes in the throat. Using the direct route of access, Thumfart's electrode applicator was used to insert a hooked-wire electrode into the muscle for laryngeal nerve conduction studies, as previous published literature states.41,42 Our protocol describes a new most accessible route. Using an external approach for both the EMG study (transcutaneous insertion) and the motor nerve conduction study of the superior and recurrent laryngeal nerves with percutaneous stimulation (ENG) makes it much easier to conduct the neurophysiological study. A recent study by Kim et al.,46 supports this idea. Patient discomfort is similar to that associated with a neurophysiological study in any other territory.
The distance between the stimulator and the recording electrode is 3cm for the superior laryngeal nerve. In the recurrent laryngeal nerve, the distance between the point of stimulation and the insertion point of the concentric needle electrode is also 3cm. (This distance does not reflect the exact route of the nerve but we serves as reference data). This is important for assessing latency and determining the nature of nerve lesions (demyelinating, axonal, or a combination of both).
The physiological characteristics of laryngeal muscles have been thoroughly described in the literature since the earliest studies:3,5,8,11,47‒49 among others.
Our findings do not differ significantly from those reported by the authors mentioned previously in terms of EMG results. Nevertheless, our protocol is distinctive in that by exploring muscles transcutaneous insertion, the study becomes more accessible and may also be useful for a subsequent conduction study with percutaneous stimulation of the nerves innervating those muscles.
There are few studies reporting reference values for motor conduction of the superior and recurrent laryngeal nerves, and the approaches they describe vary.46,50,51 For this reason, establishing a simple and functional examination technique with an external approach (percutaneous stimulation) and determining reference values for the procedure may be of great use for neurophysiological studies of the larynx.52,53 Here subsides another contribution of our study.
Our results for the Recurrent Laryngeal nerve are shown in Table 2. These values are similar to others reported by recent studies Kim SJ et al.,46 using similar techniques. In our case, a concentric needle electrode was applied directly (transcutaneous insertion) to the thyroarytenoid muscle for recording and percutaneous stimulation was performed on the lateral inferior area of the thyroid cartilage. There have been fewer studies in healthy subjects since conventional procedure is more uncomfortable to perform on the recurrent laryngeal nerve, although it does provide interesting data. Performing this technique on the superior laryngeal nerve is more straight forward and the reference values we report may be useful for future studies.
No significant age or sex differences were identified. There is no significant difference in the parameters evaluated in both sides. Neurophysiological studies of the larynx are an extremely useful and increasingly in-demand tool since they can be used for the differential diagnosis of voice alterations (dysphonia) to rule out vocal cord paresis.9‒12,37,54,55‒58 When impairment is due to alterations in the cricoarytenoid joint, EMG and ENG studies yield normal results.7,21 In some cases, dysphonia is caused by either local or generalised muscle alterations, such as polymyositis manifesting with dysphonia.24 In these cases, concentric needle electrodes inserted in the muscles of the larynx will detect increased insertion activity as well as any spontaneous activity (fibrillation potentials, positive waves, high frequency discharges, etc. depending on the aetiology). The recruitment pattern is interferential with low amplitudes and motor unit action potentials show myopathic features, that is, decreased mean duration and amplitude with an increased percentage of polyphasia.
Cases of nerve damage, such as paralysis of the laryngeal nerves secondary to surgery;13,14,16‒20,23,26,41 or of motor neuron disease, for example, display signs of axonal lesion at rest (fibrillation potentials, positive waves, fasciculations, etc.), reduced recruitment pattern with a normal amplitude, and MUAP with signs of reinnervation (increased mean duration and percentage of polyphasia). The amplitude depends on the stage of the pathological process. The neurophysiological study of the larynx is also very useful for establishing a prognosis for functional recovery.16,20,32,35,38,59,60
The ENG assesses morphology, latency (time elapsed from the stimulus to when CMAPs start), and CMAP amplitude (negative peak). It can detect alterations in the myelin sheath (increased distal latency and dispersed morphology), as in the case of Guillain-Barré syndrome.25 as well as axon alterations (neurogenic pattern in muscles innervated by those axons), and combinations of both. Both EMG and ENG are necessary for determining the progression and prognosis of the disease. Cricothyroid muscle EMG and ENG, which assess the function of one of the brainstem motor nuclei, are especially useful for diagnosing lower motor neuron disease due to the simplicity of the technique.24,25
Patients presenting fluctuating dysphonia with marked fatigability may undergo repetitive stimulation (Figure 5a) to study neuromuscular transmission (myasthenia).26‒28 This technique is conducted using surface electrodes for both stimulation (superior laryngeal nerve) and activity recording (cricothyroid muscle). Patients may also undergo single-fibre studies (jitter).61
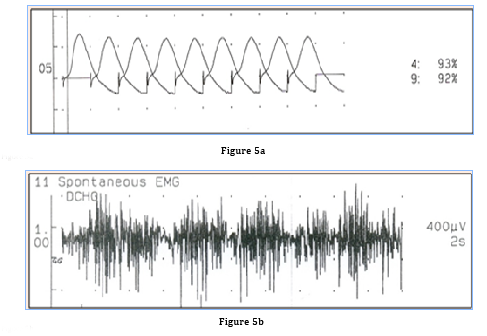
Figure 5 Examples of (a) Repetitive stimulation of the superior laryngeal nerve and recording of cricothyroid muscle activity. Laryngeal dystonia. (b) Recording of thyroarytenoid muscle activity.
EMG may also be necessary for the differential diagnosis of patients showing abnormal movements, as in dystonia (Figure 5b); this study is essential for subsequent treatment with botulinum toxin.22,29,31,33-35,62
In summary, neurophysiological studies are highly useful and relevant for diagnosing neuromuscular diseases involving laryngeal nerves or muscles. As a result, increasing numbers of researchers support use of this technique.11,56,63,64
We recommend including this technique in routine studies performed in neurophysiology and ENT laboratories, and consider it essential for diagnosing neurological disorders of the larynx.
There have been fewer studies in healthy subjects since this procedure is more uncomfortable to perform on the recurrent laryngeal nerve and thyroarytenoid muscle (limits the statistical study),65,66 although it does provide interesting data since there are not many reports of normal value in the literature with this procedure.67,68
Laryngeal electroneuromyography is essential for diagnosis and performing differential diagnosis of voice alterations. Firstly, our study presents a protocol with percutaneous stimulation on laryngeal neurography (improving the known techniques), and an external approach by transcutaneous insertion for myography. Secondly, it includes reference values on normal subjects, supporting more data to the scarce values referred on the literature. Besides, this study provides additional information supporting the use of these techniques.
This study can help determine the most suitable treatment based on the type of lesion diagnosed by these methods. Although neurophysiological exploration of laryngeal nerves and muscles is not a common procedure, laryngeal disorders are frequent and dysphonia is a relevant initial symptom of generalised neuromuscular diseases. Neurography and myography of laryngeal nerves and muscles, respectively, should therefore be included in routine studies currently performed by neurophysiology and ENT laboratories.
We would like to thank Dr J. Artieda (Department of Neurology, Universidad de Navarra) for reviewing the manuscript, A. Royuela Vicente (DptoUnidad de Bioestadística del IIS H. Puerta de Hierro-Majadahonda) and the Spanish Society of Neurology's Research Operations Office. Ethical permission number “Comité Etico 458-A”.
Authotr declares there are no conflicts of interest.
None.

©2017 Goizueta, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.