Journal of
eISSN: 2379-6359


Research Article Volume 6 Issue 1
1Faculty of medicine of Tunis University Tunis El Manar, Tunisia
2Salah Azaïez institute, Tunisia
Correspondence: Imene Yeddes Faculty of medicine of Tunis Salah Azaiez Institute University Tunis El Manar 15 Rue Djebel Lakhdhar La Rabta 1007 Tunis, Tunisie, Tel 002695539008
Received: May 04, 2016 | Published: January 6, 2017
Citation: Yeddes I, Bahloul A, Meddeb I, Ghachem BT, Mhiri A, et al. (2017) Single Photon Emission Computed Tomography/Computed Tomography (SPECT/CT) of the Skull in Necrotizing Otitis Externa: Comparison with Planar Bone Scintigraphy, SPECT and CT. J Otolaryngol ENT Res 6(1): 00145. DOI: 10.15406/joentr.2017.06.00145
Purpose: Assess the diagnostic performance of single photon emission tomography/computed tomography (SPECT/CT) for identifying necrotizing otitis externa (NOE) and compare this technique with planar bone scintigraphy (BS), SPECT and CT.
Methods: Data from 13 patients with suspected NOE were retrospectively studied. Planar BS and SPECT images were interpreted by nuclear medicine physician, CT images by radiologist and SPECT/CT images by both nuclear medicine physician and radiologist. Planar BS, SPECT and SPECT/CT images were taken as positive in the presence of increased skull base uptake and CT images in the presence of periosteal reaction and bone lysis. Clinical evolution, imaging results, microbiology and histopathology were taken into consideration to determine the final diagnosis. Sensitivity, specificity, and predictive values, were calculated for each technique. The McNemar's test chi-squared with Yates correction of 0.5 was used to compare sensitivities and specificities.
Results: SPECT/CT had the highest sensitivity (100%), followed by SPECT (90%), planar BS (80%) and CT (60%). Specificity was 100% for all imaging modalities since all reported positive cases were identified as NOE in the final diagnosis. No statistically significant difference was noted when comparing SPECT/CT with planar BS, SPECT and CT. However, borderline statistical significance was found between SPECT/CT and CT (p-value=0.08). SPECT/CT was the best imaging modalities in the accurate location of sites of osteomyelitis.
Conclusion: SPECT/CT showed high sensitivity and specificity in the diagnosis of NOE, but was not statistically superior to planar BS, CT or SPECT in this small patient population.
Keywords:necrotizing otitis externa, bone scintigraphy, single photon emission computed tomography, spect, spect/ct, ct, otalgia, otorrhea
NOE, necrotizing otitis externa; BS, bone scintigraphy; EAC, external auditory canal; CT, computed tomography; MRI, magnetic resonance imaging; SPECT, single photon emission tomography; MIP, maximum intensity projection; PPV, positive predictive value; NPV, negative predictive value
Necrotizing otitis externa (NOE), also called malignant otitis externa, corresponds to osteomyelitis of the skull base.1 NOE occurs primarily in diabetic elderly patients with a male preponderance.2 Typically due to pseudomonas aeruginosa, NOE begins as a soft tissue infection of the external auditory canal (EAC) and spreads via the fissures of Santorini and the tympanomastoid suture to involve the cranial base.3
The typical patient presents with exquisitely painful Otorrhea that is disproportionate to the clinical signs.4 Otological examination may reveal oedema of the EAC and the presence of granulation tissue.5 Prompt intravenous antibiotic treatment is required until there is resolution of symptoms and return of the EAC to normal.2 The diagnosis is based on a combination of clinical, laboratory and image findings. With absence of single definite diagnostic criteria, the diagnosis is often delayed.1
Current imaging diagnostic tools include Computed Tomography (CT), Magnetic resonance imaging (MRI) and nuclear scintigraphy. CT scan is fast and economical.6 However, CT findings of bone erosion and demineralization are late features of NOE. Magnetic resonance imaging better shows changes in soft tissue but it is generally not recommended as a first-line diagnostic imaging modality (given its lower sensitivity for imaging bone erosion compared with CT).7 99mTechnetium Methylene Diphosphonate (99mTc-MDP) planar bone scintigraphy (BS) and single photon emission tomography (SPECT) have proven reliable in early distinction between severe otitis externa and NOE.8 Although the better anatomical resolution of SPECT, both techniques have low specificity.9 Recently, some reports showed the utility of hybrid SPECT/CT in diagnosis of NOE.10,11
The objective of this study was to assess diagnostic performance of 99mTc-MDP hybrid SPECT/CT for identifying NOE and to compare it with planar BS, SPECT and CT.
Data from 13 patients with suspected NOE were retrospectively studied between February 2011 and December 2014. All patients underwent a three-phase bone scintigraphy, performed after intravenous injection of 550-750MBq of 99mTc MDP. Images were acquired on double headed SPECT camera with 2-slice CT scanner (Symbia T2 SPECT/CT; Siemens) equipped with a Parallel-hole, low-energy and high-resolution collimators. An energy window centered at 140keV with a width of 20% (126-156keV) was used.
Planar images acquisition
Rapid sequential images (flow phase) of the skull were acquired for 1min (3 seconds/frame) in a 64×64 matrix. Blood pool and delayed static images (matrix 256x256, 3minutes’ acquisition time) were acquired immediately after flow phase and at 3 hours respectively, in anterior, posterior and lateral views of the skull. Delayed whole body images (matrix 256x1024) were acquired at 3 hours.
SPECT and SPECT/CT acquisition
SPECT of the skull was acquired in a body contour orbit over 360° arcs with 64 stops and 20seconds/stop. The matrix was 128×128 and the pixel size was 4.8mm. The CT part of the SPECT/CT was acquired with acquisition parameter of 130keV voltage, 100mAs, pitch-1 and 512×512 matrix. The reconstruction of CT images was performed by using the B08 kernel for attenuation correction and the B60 kernel for bone imaging.
SPECT/CT Data processing
Attenuation correction was applied to SPECT images using the CT attenuation maps. The corrected SPECT images were reconstructed in coronal, sagittal and transaxial planes with Flash-3D software (Siemens Healthcare) with eight subsets and eight iterations. Fusion of the SPECT and CT planes and processing of fused images were carried out using the Siemens Syngo Multi Modality Workplace (Siemens Medical Solutions, Erlangen, Germany).
Image interpretation
Planar BS, SPECT, SPECT/CT and CT images were interpreted by physician blinded to the clinical findings and diagnoses. Images interpretation was made in separate sessions to minimize recall bias. Planar BS and SPECT images were interpreted by nuclear medicine physician, CT images by radiologist and SPECT/CT images by both nuclear medicine physician and radiologist. The criterion of a positive scan on planar images was an increased uptake on flow, blood pool and delayed phases. On SPECT, increased skull base uptake on maximum intensity projection (MIP) SPECT images was taken as positive. On CT, presence of periosteal reaction and bone lysis were taken as positive. In SPECT/CT, any abnormal uptake in skull base region associated or not with CT destructive bone lesion was taken as positive. Triangulation of any increased uptake regions on fused SPECT/CT planes allowed us anatomical localization and detection of associated bone lesion.
Determining of the final diagnosis
To determine the final diagnosis, many parameters were taken into consideration such as clinical presentation and evolution, imaging results (Bone scintigraphy, CT, MRI), microbiology and histopathology. Thus, 10 patients were classified having NOE. The remaining 3 patients were classified as having severe external otitis without osteomyelitis.
Statistical analysis
Sensitivity, specificity, and predictive values, were calculated for planar BS, SPECT, CT, and SPECT/CT. To compare sensitivity and specificity of these diagnostic tests, we used the McNemar's test chi-squared with Yates correction of 0.5 applied on 2 by 2 contingency tables. A low value of the calculated p-value <0.05 (significance level α=5%) was considered a significant result to demonstrate superiority of one diagnostic test over another. All statistical analysis was performed using SPSS (IBM SPSS Statistics, IBM Company).
Patient characteristics
Thirteen patients with clinically suspected NOE were included. Patient characteristics including age, sex, diabetes, clinical presentation, imaging findings, and final diagnosis are detailed in Table 1. The mean age was 72±11.2years. Nine patients (69%) were male and four (31%) were female. Ten patients (77%) were diabetic. All patients presented otalgia which was left sided in 7 cases (54%) and right sided in 6 cases (44%). On the basis of the final diagnosis, ten patients (77%) had NOE with skull base osteomyelitis and three patients had severe external otitis without skull base osteomyelitis.
No. |
Age |
Sex |
Diabetes |
Clinic Symptoms |
CT |
Planar Images |
SPECT |
SPECT/CT |
Final Diagnosis |
|
1 |
63 |
M |
Yes |
Otalgia, Otorrhea |
No bone erosion |
Significant uptake (T) |
Significant uptake |
Significant uptake (Sq+Ty) |
NOE |
|
2 |
74 |
M |
No |
Otalgia, Otorrhea |
bone erosion |
Significant uptake (T) |
Significant uptake |
Significant uptake (P+M) |
NOE |
|
3 |
75 |
M |
Yes |
Otalgia, Facial palsy |
bone erosion |
Significant uptake (T) |
Significant uptake (T+S) |
Significant uptake (T+S) |
NOE |
|
4 |
70 |
M |
Yes |
Otalgia, Otorrhea |
bone erosion |
Significant uptake (T) |
Significant uptake |
Significant uptake (M) |
NOE |
|
5 |
89 |
M |
Yes |
Otalgia |
No bone erosion |
Significant uptake (T) |
Significant uptake (T+S) |
Significant uptake (T+S) |
NOE |
|
6 |
62 |
F |
Yes |
Otalgia, Otorrhea |
No bone erosion |
No significant uptake |
No significant |
No significant uptake |
SOE |
|
7 |
48 |
F |
Yes |
Otalgia, Otorrhea |
No bone erosion |
No significant uptake |
No significant |
No significant uptake |
SOE |
|
8 |
74 |
M |
Yes |
Otalgia, Otorrhea |
bone erosion |
Significant uptake (T) |
Significant uptake |
Significant uptake (P+TM) |
NOE |
|
9 |
76 |
M |
Yes |
Otalgia, Facial palsy |
bone erosion |
No significant uptake |
Significant uptake |
Significant uptake (P+M) |
NOE |
|
10 |
90 |
F |
No |
Otalgia, Otorrhea |
No bone erosion |
No significant uptake |
No significant |
No significant uptake |
SOE |
|
11 |
74 |
M |
No |
Otalgia, Otorrhea |
No bone erosion |
No significant uptake |
No significant |
Significant uptake (Ty) |
NOE |
|
12 |
74 |
F |
Yes |
Otalgia, Otorrhea |
bone erosion |
Significant uptake (T) |
Significant uptake |
Significant uptake (P+M) |
NOE |
|
13 |
63 |
M |
Yes |
Otalgia, Otorrhea |
No bone erosion |
Significant uptake (T) |
Significant uptake |
Significant uptake (Sq+Ty) |
NOE |
Table 1 Patient characteristics
NOE: Necrotizing Otitis Externa; SOE: Severe Otitis Externa; T: Temporal Bone; S: Sphenoid Bone; M: Mastoid process of the temporal bone; P: Petrous portion of the temporal bone; Sq: Squamous portion of temporal bone; Ty: Tympanic bone; TM: Temporomandibular joint
Planar BS, CT, SPECT and SPECT/CT
The sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), and accuracy of planar BS, CT, SPECT, and SPECT/CT are detailed in Table 2. Typical cases are shown in Figures 1, 2 & 3. The diagnostic accuracy was lowest for CT (69.2 %) and highest for SPECT/CT (100 %). SPECT/CT had the highest sensitivity (100%). Specificity was 100% (3/3) for all imaging modalities since all positive cases reported by CT, planar BS, SPECT and SPECT/CT were identified as NOE in the final diagnosis.
|
Planar BS |
CT |
SPECT |
SPECT/CT |
|
Sensitivity |
80% (8/10) |
60% (6/10) |
90% (9/10) |
100% (10/10) |
|
(44.4-97.5) |
(24.2-87.8) |
(55.5-99.7) |
(69.1-100) |
||
Specificity |
100% (3/3) |
100% (3/3) |
100% (3/3) |
100% (3/3) |
|
(29.3-100%) |
(29.3-100) |
(29.3-100) |
(29.2-100) |
||
PPV |
100% (8/8) |
100% (6/6) |
100% (9/9) |
100% (10/10) |
|
(63.1-100) |
(54.1-100%) |
(63.4-100%) |
(69.1-100) |
||
NPV |
60% (3/5) |
42.9% (3/7) |
75% (3/4) |
100% (3/3) |
|
(14.7-94.7) |
(9.9-81.6) |
(19.4-99.4) |
(29.2-100) |
||
Accuracy |
84.6% (11/13) |
69.2% (9/13) |
92.3% (12/13) |
100% (13/13) |
|
Table 2 Sensitivity, specificity, PPV, NPV and accuracy of planar BS, CT, SPECT and SPECT/CT for diagnostic of NOE (with 95% confidence interval)
The temporal bone was involved on imaging in all cases of NOE (n=10). SPECT and SPECT/CT showed associated involvement of the sphenoid bone in 20% of NOE (n=2). SPECT/CT was the best imaging modalities in accurate location of involved bones. Planar BS was less preferment in this sense.
Figure 1, A 74year old non diabetic male, presented with severe otalgia and Otorrhea. The clinical exam showed inflammation and stenosis of the external auditory canal. Bone scintigraphy was performed for suspected NOE. Planar BS images (a, b) showed increased radiotracer uptake in the left temporal bone (arrow). SPECT images (c, f) showed also increased uptake in the left temporal bone. SPECT/CT Images (e, h) allowed accurate location of the site of involvement showing increased uptake in petrous portion (arrowhead) and mastoid process (arrow). CT images (d, g) showed osteolysis in the petrous portion of the temporal bone (arrowhead). On clinical follow up the patient started improving with systemic antibiotics and the final diagnosis was NOE.
Figure 2, A 63year old diabetic male, presented with unrelenting otalgia and persistent purulent Otorrhea refractory to antibiotics. The clinical exam showed oedema, stenosis and granulation tissue of the external auditory canal. Planar BS (a, b) and SPECT images (c, f) showed increased radiotracer uptake (arrow) in the right temporal bone. CT images (d, g) did not reveal any obvious abnormality. SPECT/CT images (e, h) showed increased radiotracer uptake in the squamous portion (arrow) and tympanic portion (arrowhead) of temporal bone. Considering clinical follow and bone scintigraphy, the final diagnosis was NOE. This case illustrate that bone scintigraphy is more sensitive than CT. SPECT/CT was superior to planar BS and SPECT in accurately locating the involved bone.
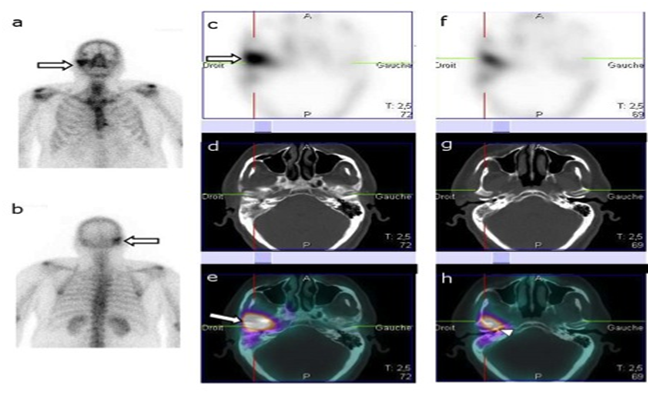
Figure 2 The clinical exam showed oedema, stenosis and granulation tissue of the external auditory canal.
Figure 3, A 76year old diabetic male, presented with severe otalgia and facial nerve palsy. The clinical exam showed inflammation and stenosis of the external auditory canal. Blood pool images (a, b) were normal. Delayed static images (c, d) showed slight increased uptake in the temporal bone region. Planar BS was judged to be negative. SPECT image (e) showed obvious increased radiotracer uptake in the petrous portion of the right temporal bone (arrow). CT image (f) showed right petrous bone osteolysis (arrowhead). SPECT/CT Image (g) showed increased radiotracer uptake in petrous (arrowhead) and mastoid portion of right temporal bone. Considering clinical follow and imaging findings, the final diagnosis was NOE. This case illustrate that SPECT and SPECT/CT are more sensitive than Planar BS.
Comparison of imaging modalities
The results of the comparison of planar BS, CT, SPECT and SPECT/CT sensitivities using the McNemar's test chi-squared with Yates correction of 0.5 are detailed in Table 3. Borderline statistical significance was found between CT and SPECT/CT (p-value=0.08). No statistically proved significant difference was noted between Planar BS and SPECT (p=0.62), SPECT and SPECT/CT (p=0.62), CT and Planar BS (p=0.45), Planar BS and SPECT/CT (p=0.29) and CT and SPECT (p=0.15).
Compared Modalities |
chi-squared |
p-value |
Planar BS-SPECT |
0.25 |
0.62 |
SPECT-SPECT/CT |
0.25 |
0.62 |
CT-Planar BS |
0.56 |
0.45 |
Planar-SPECT/CT |
1.12 |
0.29 |
CT-SPECT |
2.08 |
0.15 |
CT-SPECT/CT |
3.06 |
0.08 |
Table 3 Comparison of planar BS, CT, SPECT and SPECT/CT sensitivities using the McNemar's test chi-squared with Yates correction of 0.5
Necrotizing otitis externa is a severe infection of EAC with progression to adjacent soft tissue and osseous structures. Patients with NOE are mostly elderly diabetic people presented as Otorrhea and otalgia.4 Current diagnostic tools include CT, MRI and nuclear scintigraphy. The combination of radiological and radionuclide exams is crucial both in initial diagnosis and further follow-up of the treatment response.12
CT scanning was found to be a fast and economical tool in the initial assessment of patients with NOE.6 Initial CT findings in NOE include effacement of fat planes in the sub temporal area13 and subtle cortical bone erosions. However, CT scanning has limitations. First, CT evidence of osteolysis is a common finding but it can be associated with various tumors and congenital lesions of the skull base.2 Hence CT cannot always provide a distinction between inflammatory and neoplastic processes. Second, more than 30% of the affected bone must be demineralized to appear eroded on CT.4,14 Therefore in the early stage of osteomyelitis before bone demineralization, there may be no bony changes seen on CT.5 This fact may explain the low sensitivity of CT (60%) seen in our study.
Due to its superior contrast resolution, MRI is the imaging technique of choice in assessing soft-tissue involvement in NOE.7,15 On T1-weighted images the EAC and soft tissues within the sub temporal region are thickened and demonstrate reduced T1 signal.5,7 The T2-weighted sequences return isointense or slightly hyperintense signal intensity. Assessment of potential skull base and intracranial complications can be made by MRI due to its ability to assess involvement of the medullary space of bone and identify subtle dural enhancement. Highly sensitive MRI findings of osteomyelitis include marrow T1 hypo intensity and T2 hyper intensity.16 The use of fat suppression on the post gadolinium study is necessary to assess skull base enhancement accurately. However, MRI is nonspecific and differential diagnoses of central skull base osteomyelitis including neoplastic and non-neoplastic entities (inflammatory pseudo tumor, Wegener granulomatosis, tuberculosis, sarcoid, fibrous dysplasia, and Paget disease) must be ruled out.16
99mTc-MDP planar BS and SPECT are known to be sensitive modalities in detecting bony involvement even if the CT examination is normal allowing earlier diagnosis of NOE and treatment initiation.17 Hardoff et al.,8 reported that early and reliable distinction between severe otitis externa and NOE can be made in diabetic patients by using Lesion-to-nonlesion count ratios on SPECT bone scintigraphy. In our study, 99mTc-MDP planar BS and SPECT showed retrospectively a sensitivity of 80% and 90%. The site of the infection was localized by planar BS in the temporal bone in 8 positive cases. Accurate location of the site of involvement in the temporal bone was made by SPECT in 2 cases among the positive cases on planar BS. In 2 cases SPECT shows supplementary sphenoid bone involvement compared to planar BS. Hence, SPECT was more sensitive in detecting NOE and more accurate in locating the site of infection than planar BS.
Chakraborty D et al.,19 have reported an important role of SPECT/CT in early evaluating the extent of skull base involvement in case of NOE. Chen et al. 11 recommended to use routinely SPECT/CT when assessing patients with suspected NOE even without evidence of lesion on planar images. In a recent study by Sharma et al.,20 99mTc-MDP SPECT/CT locate the site of involvement in all patients and enabled highly accurate diagnosis of skull base osteomyelitis. In our study, SPECT/CT showed a high sensitivity (100%). There were no false negative cases and all negatives cases were classified as severe external otitis without osteomyelitis on the final diagnosis. In one patient, the diagnosis of NOE was made by SPECT/CT while other imaging modalities were negative. Thus, SPECT/CT changed the final report in one case.
Planar images are a sum of uptake from all tissues imaged. That’s why it may be possible that planar bone scintigraphy may include uptake from bony structures and inflamed soft tissues as well.18 By combining SPECT and CT, fused images allow anatomic location of the site of uptake and enable better differentiation between inflamed soft tissue uptake and bony structures uptake. SPECT/CT gave an accurate location of the site of osteomyelitis in 6 cases among the 8 positive cases on planar BS. SPECT/CT was more accurate in locating the involved bone in 6 cases among the 9 positive cases on SPECT. The involvement of the sphenoid bone missed on planar BS and seen on SPECT was confirmed by SPECT/CT images. Hence, by combining functional and anatomic images, SPECT/CT emerged as the most accurate modality in locating the site of osteomyelitis.
High specificity (100%) was found for all imaging modalities. There were no false positive cases and all positive cases reported by CT, planar BS, SPECT and SPECT/CT were identified as NOE in the final diagnosis. SPECT/CT appeared to be the most sensitive (100%) while CT showed the lower sensitivity (60%) with 4 false negative cases. However, there was no statistically significant difference when comparing imaging modalities sensitivities probably because of the small sample size. A borderline statistical significance (p-value =0.08) was found when comparing sensitivities of SPECT/CT and CT.
This study has some limitations which have to be pointed out. First, the small patient population of the study reduced its statistical power. To deal with that and to recruit as many eligible cases as possible, the study included patients with suspected NOE for a period of 4years. The second limitation was the retrospective nature of the study. Third, MRI findings were not available. To overcome such limitations, we suggest performing a large multicenter prospective study comparing SPECT/CT and MRI.
99Tc-MDP SPECT/CT enabled high sensitivity and specificity in the diagnosis of NOE in this small patient population. SPECT/CT provided accurate location of the skull base site of osteomyelitis. However, no statistically significant difference was found when comparing the sensitivity of SPECT/CT with that of CT, planar BS and SPECT.
This article does not contain any studies with human participants or animals performed by any of the authors.
None.
Author declares there are no conflicts of interest.
None.

©2017 Yeddes, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.