Journal of
eISSN: 2379-6359


Case Report Volume 5 Issue 2
Department of Otolaryngology, The General Hospital of Mexico, Mexico
Correspondence: Alfredo Carrillo Munoz Euler 152 int 204 Mexico City, Mexico, Tel +52(55)5908-1325
Received: May 11, 2016 | Published: December 29, 2016
Citation: Carrillo-Munoz A (2016) Cholesteatoma of the External Auditory Canal: A Case Report. J Otolaryngol ENT Res 5(2): 00138. DOI: 10.15406/joentr.2016.05.00138
Cholesteatoma of external auditory canal a rare pathology. Clinically, it is a mass of keratin that erodes the ear canal, causing necrosis and bone lysis through several mechanisms. We present a case of this disease in a 40-year-old patient with symptoms of several years of evolution, treated by canal wall-down mastoidectomy with complete removal of cholesteatoma without recurrence at 2years.
Keywords: cholesteatoma, external auditory canal, keratosis obturans, canaloplasty, bone erosion, chronic otorrhea, jugular fossa, mastoidectomy, facial palsy
Cholesteatoma of the External Auditory Canal Cholesteatoma of (CEAC) is defined as an accumulation of keratin that produces periosteitis and bone erosion of its walls1-4 (usually in their lower portions or above) the eardrum and middle ear sometimes not affected.5 It differs from the keratosis obturans because it produces a circumferential widening of the EAC, chronic Otorrhea and pain, but no concomitant bone lysis.
The CEAC is a rare disease, its diagnosis is mainly clinical and is based on imaging studies however, it is often not diagnosed promptly. It is estimated that the CEAC is responsible for 0.1-0.5% of otologic pathology1,3 with an incidence of 0.3 cases per year per 100,000 inhabitants; that is, sixty times less than its nearest equivalent, ear cholesteatoma of the middle ear.6
Its origin may be spontaneous or arise from a previous ear condition or surgical procedure.7 Spontaneous CEAC is slightly less frequent, constituting approximately 48% of cases.8
Because the CEAC has no pathognomonic signs or symptoms, often confused with keroatosis obturans during clinical evaluation. For this reason, the pattern of bone erosion, detection of necrosis and sequestrum of the underlying bone is essential to carry out an accurate diagnosis.
Due to advances in imaging methods, the CEAC can be differentiated from other diseases and inflammatory or EAC tumors processes.3,4 Also it must be differentiated from necrotizing otitis externa and malignant tumors such as squamous cell carcinoma of the EAC.
Treatment involves removal of granulation tissue. Usually accompanied by performing a canaloplasty, mastoidectomy or obliteration of the residual defect, as the case warrants, being sure to remove all bone matrix and necrotic tissue.
Here, we present a case of spontaneous CEAC with a literature review in order to spread the existence of this rare entity, presenting clinical features and emphasizing proper diagnosis and treatment.
40-year-old female with a tumor in the left EAC. Her history of spontaneous whitish not fetid left intermittent Otorrhea for the past 4years. During this time she has experienced occasional left mild sharp earache and mild progressive hearing loss. She also denies other otologic symptoms. Otoscopy reveals a 100% blocked EAC due a pedunculated, smooth, regular edges, pink, mobile tumor, covered with fetid non mucoid whitish discharge (Figure 1). The right EAC is normal. Exploration with 256, 512 and 1024Hz tuning shows a left sided conductive loss. General laboratory studies: blood count, blood chemistry normal. VDRL negative. Audiometric finding: severe left conductive could not be performed due the presence of the tumor.
CT scan temporal bone shows left mastoid cells occupied by soft tissue density suggestive of chronic disease and EAC with the presence of soft tissue density, the tympanic cavity is also occupied by same soft tissue density that erodes its walls and no ossicular chain is observed. Carotid artery, jugular fossa, semicircular canals, cochlea and other structures unchanged (Figure 2). The right ear is normal. The skull MRI shows a hypointense occupying the left EAC on T1 that becomes hyper intense in T2 sequence and shows a heterogeneous enhancement when contrast is applied (Figure 3).
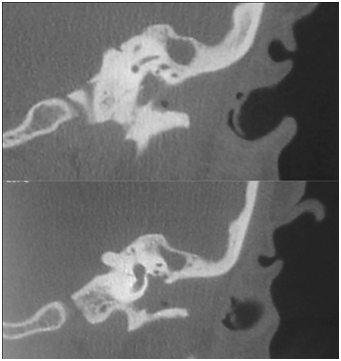
Figure 2A Coronal CT scan with tumor in the EAC and tympanic cavity; lysis of the tympanic membrane and oscicular chain.
We decided to schedule the patient for surgical and resection of tumor of the EAC. A retroauricular approach was performed, accessing to the EAC and we found a tumor invading and eroding the posterior wall, invading the mastoid process, there was no eardrum or ossicular chain. A wall-down mastoidectomy was performed. There were no incidents during the procedure. After two years of follow-up the patient is still free of disease.
CEAC is an accumulation of keratin with osteitic and osteloytic capacity.1,2,9 It is a diagnostic challenge because of its invasive nature and the wide range of possibilities before the clinician faces against a mass of such characteristics.
The etiology and pathogenesis are still poorly understood, but there are several theories about its origin, including: localized periostitis, chronic inflammation of the EAC, failure in the epithelial cells clearance mechanisms or the dehiscence of the petrotimpanic fissure.4
All these theories converge on the idea that maybe ischemia and secondary bone infection due the keratin accumulation eventually lead to necrosis and reactive periostitis of the bony EAC.3,6 According to available literature, this disease most often affects elderly patients, is mostly one-sided presentation and there is no gender predominance.9,10
Audiometric state is usually variable; it can be found from normal hearing to moderate conductive hearing loss.11 Histopathological studies confirm the presence of periostitis located in the eroded area, periosteitis and bone sequestrums, and granulation tissue. It is common to find epidermal epithelial cells surrounding bone sequestrum. The matrix of keratin begins to reshape and form recesses that invade the mastoid and other middle ear structures.1,12
In spontaneous cases, patients do not have any history of otologic symptoms and there is wide variation in frequency and quantity of Otorrhea, otalgia, and facial palsy. On physical examination, this tumor often extends to the floor of the and the posterior wall near the osteochondral junction of the canal. The eroded area is usually filled by bone sequestrum. The appearance of the tympanic membrane is variable and can range from an intact or slightly hyperemic membrane, to be absent with lysis of the ossicles and tympanic cavity walls.
The role of imaging studies is crucial to make the correct diagnosis, assess extension and surgical treatment. They allow you to define the location, depth of invasion of concomitant structures and plan a more suitable approach for a complete resection of the disease. Typically, the CEAC is observed as an oval-shaped soft tissue density associated with bone lysis and regular margins. Bone erosions can reach forward to the temporomandibular joint, hypo tympanum and the jugular bulb inferiorly, posteriorly may involve the mastoid and the fallopian canal; nevertheless, the tympanic membrane may remain intact.1,3
Naim et al proposed the first classification for CEAC. They divided the CEAC in the following stages for study: stage I, hyperplasia of the canal epithelium; stage II, periosteitis; stage III, defective bony canal; and stage IV, erosion of the adjacent anatomic structure.12
A more recent classification proposed by Shin et al.,13 considers tomographic findings and is useful as a guide for addressing the surgical approach: Stage I: Cholesteatoma of external auditory canal only: Stage II: invasion of the membrane and tympanic cavity; Stage III: with invasion of mastoid; Stage IV: extra temporal extension.
It is important to distinguish when evaluating a probable spontaneous CEAC, because there are other diseases with very similar features so that history of local trauma, surgery, acquired stenosis, epithelial cysts, or epidermal invasions secondary to temporal bone fracture.3
Because of its ability to cause necrosis of the temporal bone and subsequent accumulation of keratin in the EAC, we must take into account any history of head and neck radiation.12,13 Another differential diagnosis is necrotizing otitis externa, which should be suspected in the presence of risk factors such as: elderly immunocompromised patients, diabetes mellitus, etc. and in which we see abundant stenosis and granulation tissue in the osteochondral junction of the EAC. In this entity, imaging studies are very useful in early detection.
Finally, biopsy should always be considered searching for malignancy.3 Treatment depends on the stage of the disease. For localized lesions, treatment consists on debridement of necrotic tissue and keratin. In larger defects, a mastoidectomy and reconstruction of the EAC should be considered.1,11 Surgical criteria include chronic pain, recurrent infections with resistant strains despite proper cleaning and debridement, complications such as facial palsy or the presence of vertigo.3,6
There is no exact frequency of recurrences reported in the literature so that long-term monitoring is recommended in all cases. By using open surgical techniques as wall-down mastoidectomy, microscopic exploration helps to detect early recurrence. In cases where closed techniques are preferred, annual tomographic scanning is recommended or in the presence of symptoms that suggest recurrence such as facial palsy, Otorrhea, or otalgiam.14
None.
Author declares there are no conflicts of interest.
None.

©2016 Carrillo-Munoz. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.