Journal of
eISSN: 2373-437X


Clinical Paper Volume 4 Issue 2
1Microbiologist, Medical Microbiology Unit Head, Angios Vascular Center & Wound Clinic, Venezuela
2Aggregate Professor Microbiology, Universidad Central de Venezuela, Venezuela
3Internal Medicine Specialist, Angios Vascular Center & Wound Clinic, Venezuela
Correspondence: Marcel Marcano-Lozada, MD. Medical Microbiology Unit, Angios Vascular Center & Wound Clinic, Caracas, Venezuela
Received: February 14, 2017 | Published: March 1, 2017
Citation: Lozada MM, Leon SM (2017) Mrsa Biofilm-Producer Chronic Osteomielitis in a Diabetic Patient Successfully Treated with Antimicrobial Monotherapy. J Microbiol Exp 4(2): 00108 DOI: 10.15406/jmen.2017.04.00108
We presented in a schematized way a clinical case of a diabetic patient with severe chronic osteomyelitis that involves the microbiological diagnosis and therapeutic management that ends in the health restitution after the treatment.
M.P. is a male, 75 years old with 5 important morbidities:
Polymedicated for all the mentioned pathologies.
He comes to the Medical Microbiology Unit in January 2010 with a chronic right pretibial ulcer of 7 years of evolution that increased size in the previous year and presents in the bottom one fistula and purulent discharge, severe pain and limitation for walking.
The microbiological isolates, treatments & clinical evolution (partial outcome) at different medical facilities for the previous 7 years to the Medical Microbiology
Unit intervention was the following:
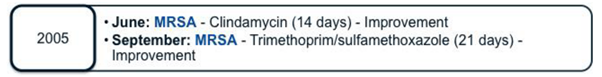
MSSA: Methicillin-Sensible Staphylococcus aureus, EFA: Enterococcus faecalis
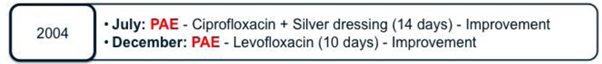
PAE: Pseudomonas aeruginosa
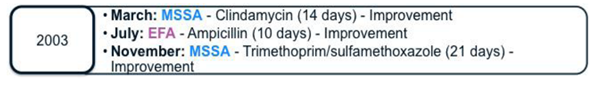
MRSA: Methicillin-Resistant Staphylococcus aureus
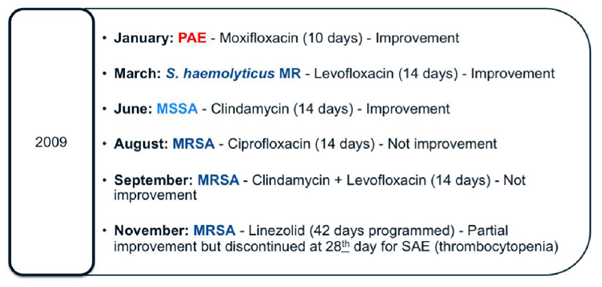
S. haemolyticus MR: Staphylococcus haemolyticus Methicillin-Resistant
In January 2010, the patient comes to Angios Vascular Centre and was referred to the Medical Microbiology Unit for clinical & microbiological evaluation for the expert physician in Medical Microbiology, and the multidisciplinary approach for different specialties. The microbiological isolates, treatments & clinical evolution in the year 2010 were the following:
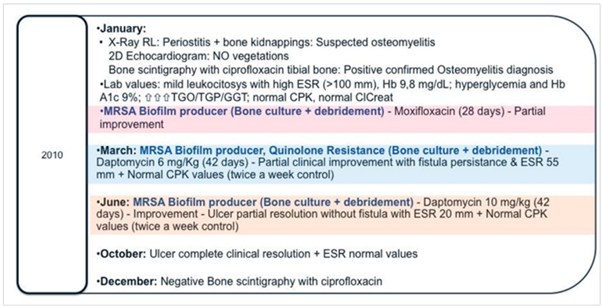
ESR: Erythrocyte Sedimentation Rate, HbA1c: Glycohemoglobin, CPK: Creatine PhosphoKinase, ClCreat: Creatinine Clearance
We present in detail the antimicrobial susceptibility patterns from the three MRSA isolates of right tibial bone samples obtained during the treatment: (Table 1).
Antibiotic |
January |
March |
June |
Susceptibility Repot |
|||
pencillin |
R |
R |
R |
Oxacillin |
R |
R |
R |
Erithromycin |
R |
R |
R |
Clindamycin |
R |
R |
R |
Ciprofloxacin |
S |
S |
S |
Gentamicin |
S |
S |
S |
Trimethoprism-sulfamethoxazole |
S |
S |
S |
Rifampin |
S |
S |
S |
Quinupristin/dalfopristin |
S |
S |
S |
Teicoplanin |
S |
S |
S |
Linezolid |
S |
S |
S |
Vancomycin |
S 1,5µg/mL |
S 1,5µg/mL |
S 1µg/mL |
Daptomycin |
S 0.032µg/mL |
S 0.19µg/mL |
S 0.19µg/mL |
Table 1 Susceptibility Repot
S, Susceptible; R, Resistant
*Susceptibility to Vancomycin and Daptomycin was performed by the E-test method, for the remaining antimicrobials were performed by the disc diffusion method.
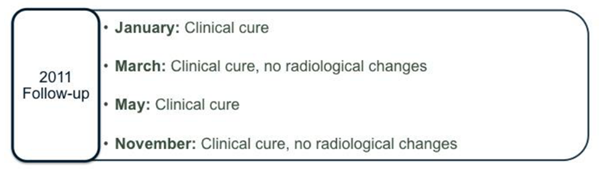
The successful one-year follow-up clinical outcome:
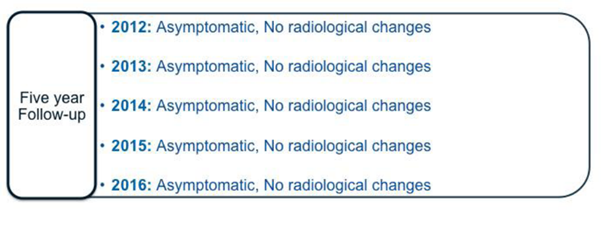
At next five-year follow-up the successful clinical outcome remains:
The correct diagnosis of the etiology of chronic osteomyelitis in an elderly patient, severely ill and with multiple treatment failures, can guide anti-infective therapy to achieve bone eradication of bacterial infection.
In the case at hand, the appropriate surgical intervention with a broad osteotomy in the required opportunities (three times), which also allowed the microorganism to be identified and could continue to be directed, and rotating antimicrobial therapy, since the emergence of resistance to wuinolones resulted in the choice of Daptomycin at doses similar to those used in bacteremia for 6 weeks (6mg/Kg), and subsequently allowed to define the escalation of doses of Daptomycin at 10mg/Kg for a further 6 weeks, without any adverse events during this treatment. At the time of this intervention, the escalation monotherapy with Daptomycin has no many reported experience, and de-escalation generally was associated with muscle or nephrotoxicity.
All the anti-infective therapy was intravenous administered in the ambulatory setting know as OPAT (Outpatient Parenteral Antimicrobial Therapy), in a special unit dedicated to the one-daily administration of the medication, in order to avoid hospitalization and its complications, and reducing costs based on a pharmacoeconomic model in addition, the patients daily routine was not affected.
At follow-up at the first year and then at the following five years, clinical and radiological cure is maintained, with no bone changes or fistulas or pain in the affected limb.
It is noteworthy that in our case, the patient was not a candidate to use combination therapy because of the liver disease he presented and, in addition, the expected drug interactions complicated the use of combination therapy that could have eliminated the biofilm-producing microorganism much more early. In special situations such as this, it is demonstrated that the use of long-term high-potency monotherapy can achieve the cure of osteomyelitis (including that caused by biofilm-producing bacteria) and return an adequate quality of life to the patient.
None.
The authors declare no conflict of interest.
None.

©2017 Lozada, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.