Journal of
eISSN: 2376-0060


Research Article Volume 6 Issue 4
1Department of Physiology, Elsheikh Abdallah Elbadri University, Sudan
2Department of Physiology, National Ribat University, Sudan
Correspondence: Omer Abdalla Elbedri Abdalla, Department of Physiology, Faculty of Medicine, Elsheikh Abdallah Elbadri University, Berber, PO Box 25, Nile State, Sudan
Received: August 23, 2019 | Published: August 16, 2019
Citation: Abdalla OAE, Musa OA. Respiratory muscles power reversibility test as a new test in asthma diagnosis. J Lung Pulm Respir Res . 2019;6(4):73-75. DOI: 10.15406/jlprr.2019.03.00211
Making diagnosis of asthma requires a critical evaluation of the patient’s symptoms, medical history, physical examination and diagnostic tests. It is known that a reduction of respiratory muscle pressures (MIP and MEP) for assessment of respiratory muscles power has been associated with several neuromuscular diseases, but it is also possible to point out lower values in patients with chronic obstructive pulmonary diseases as in asthma. As asthma diagnosis by reversibility test is not very sensitive in intermittent and mild asthma and pulmonary function is related to respiratory muscle pressures (RMP), could we use the reversibility of RMP in the patients for asthma diagnosis is the main issue investigated in this research. The aim of the study to determine the validity of asthma diagnosis by reversibility testing of respiratory muscles power. A cross-sectional hospital based study carried out in Lung function tests clinic in Police and Alban Gadeed hospitals in Khartoum during the years 2010-2011 to determine the reversibility of the lung function (FEV1 and PEFR) and respiratory muscles power (MEP and MIP). Thirty five known asthmatic subjects attending the referred chest clinic for follow up, and 20 healthy non asthmatic controls were included in the study. FEV1, PEFR, MEP and MIP were measured for all subjects before and after bronchodilator. Reversibility test was considered positive assuming the cut-off point for FEV1, MEP and MIP is ≥12% and for PEFR≥20%.The results showed percent of change in asthmatic group before and after bronchodilator test for FEV1 , PEFR, MEP, MIP were: 10.45, 11.84, 12.15 and 16.73 respectively. The difference was statistically significant. Sensitivity and specificity of reversibility testing for FEV1 (40%, 75%), for PEFR (31%, 65%), for MEP (49%, 70%) and for MIP (71%, 65%). In conclusion, the respiratory muscles power reversibility test could be a potentially sensitive diagnostic test for asthma
Keywords: pulmonary, lung function, respiratory muscles power, asthma
FVC, forced vital capacity; FEV1, forced expiratory volume in first second; PEFR, peak expiratory flow rate; RMP, respiratory muscle pressures; MEP, maximal expiratory pressure; MIP, maximal inspiratory pressure
Making the diagnosis of asthma requires a critical evaluation of the patient’s symptoms, medical history, physical examination and diagnostic tests.1
In several diseases, the evaluation of respiratory muscles power can prove to be very useful. The measurement of the respiratory muscle pressures (MEP, maximal expiratory pressure; MIP, maximal inspiratory pressure) is the most widely used to assess respiratory muscles power.2,3 It is known that a reduction of MIP and MEP has been associated with several neuromuscular diseases, but it is also possible to point out lower values in patients with chronic obstructive pulmonary diseases as in asthma.4-6 Age and sex could influence MIP and MEP values; these are lower in females than in males and quite constant until seventy years of age when they start to decrease.7
Inspiratory muscle training (IMT) was studied in a group of 25 children with asthma and compared with another 25 asthmatic controls not subjected to the same IMT as the first ones. MIP, MEP and PEFR increased significantly in IMT group. MIP increased from-48.32±5.70 to-109.92±18.04cm H2O and MEP increased from 50.64±6.55 to 82.04±17.01cmH2O and PEFR increased from 173.60±50.82 to 312.00±54.85. The study concluded that IMT can increase the efficiency of respiratory muscles, lung function and improve the clinical situation of the patients.8 This positive correlation of IMT and improved pulmonary function indicate the important relation between respiratory muscle pressures (RMP) and the level of pulmonary function value.
Reversibility test is considered positive for asthma diagnosis if FEV1 is increased by 12-15%. Values more than 12% in FEV1 compared to baseline during a single testing session suggest significant bronchodilation.9,10 An improvement of more than 20% from baseline in PEFR is also considered positive response to bronchodilators as recommended by British Thoracic Society (BTS).11
Low sensitivity of the reversibility test by pulmonary function may need to search for other tests to diagnose asthma as in mild & intermittent asthma types.
As asthma diagnosis by reversibility test is not very sensitive in intermittent and mild asthma, and pulmonary function is related to RMP, could we use the reversibility of RMP in the patients for asthma diagnosis is the main issue investigated in this research.
General:
Specific:
This study aim at the following:
This is a cross-sectional hospital based study carried out in Lung function tests clinic in Police and Alban Gadeed hospitals in Khartoum during the years 2010-2011 to determine the reversibility of the lung function (FEV1 and PEFR) and respiratory muscles power (MEP and MIP). Thirty five known asthmatic subjects (19 female,16 males) attending the referred chest clinic for follow up , and 20 healthy non asthmatic controls (12 female, 8males) were included in the study.
Following signed written consent, baseline test for FEV1, PEFR, MEP and MIP (before bronchodilator) were obtained for all subjects. Two to four puffs of salbutamol inhaler were given to all subjects through mouth via a spacer device and the same test was repeated for all subjects after 15minutes of salbutamol inhaler (after bronchodilator). The % of change of each parameter was calculated.
Lung function (FVC, FEV1, PEFR) and respiratory muscle pressures (MEP, MIP) were measured using digital spirometer and respiratory pressure meter respectively. Paired t- test was used for comparing variables before and after the test. P value<0.05 were considered to be significant. Reversibility test was considered positive assuming the cut-off point for FEV1, MEP and MIP is≥12% and for PEFR≥20%.
35 asthmatic subjects (19 females and 16 males) and 20 non asthmatic healthy controls (12 females and 8 males) were included in the study. The two groups were matched in terms of age, sex height (ht) and weight (wt). Mean, standard deviation (SD) before and after bronchodilator test in asthmatics were as follows: FVC (2.56±0.86, 2.83±0.90L), FEV1 (2.01±0.78, 2.22±0.80L), PEFR (291.77±127.87, 326.31±137.91liter/sec), MEP (82.54±23.44, 92.57±26.90cm H2O) and MIP (65.37±26.92, 76.31±25.62cmH2O). The percent of change after bronchodilator test were: 10.54, 10.45, 11.84, 12.15 and 16.73 respectively (Table 1)(Figure 1). The difference was statistically significant. Mean, SD before and after bronchodilator test in control group were as follows: FVC (3.10±0.64, 3.15±0.61L), FEV1 (2.71±0.57, 2.79±0.59L), PEFR (329.45±120.71, 338.65±125.39L/sec), MEP (81.10±24.74, 84.75±27.15cmH2O) and MIP (72.60±24.05, 74.30±24.60cmH2O). The percent of change after bronchodilator test were: 1.61, 2.95, 2.79, 4.50 and 3.18 respectively. The difference was statistically insignificant. The total number of cases with positive MEP, MIP, FEV1 and PEFR reversibility testing in asthmatics was: 17, 25, 14 and 11 respectively. Sensitivity and specificity of reversibility testing in all asthmatic subjects for FEV1 (40%, 75%), for PEFR (31%, 65%), for MEP (49%, 70%) and for MIP (71%, 65%). Sensitivity of FEV1, PEFR, MEP and MIP reversibility testing in mild & intermittent asthma were 29%, 29%, 43% and 67% respectively and in severe & moderate asthma were 50%, 33%, 57% and 78% respectively (Table 2).
Parameter |
Asthmatics |
% change |
P value |
mean±SD |
|||
FVC(L) before BD |
2.56±0.86 |
10.54 |
0.007 |
FVC(L) after BD |
2.83±0.90 |
||
FEV1(L) before BD |
2.01±0.78 |
10.45 |
0.000 |
FEV1(L) after BD |
2.22±0.80 |
||
PEFR(L/sec) before BD |
291.77±127.87 |
11.84 |
0.001 |
PEFR(L/sec) after BD |
326.31±137.91 |
||
MEP(cmH2O) before BD |
82.54±23.44 |
12.15 |
0.002 |
MEP(cmH2O) after BD |
92.57±26.90 |
||
MIP(cmH2O) before BD |
65.37±26.92 |
17.73 |
0.000 |
MIP(cmH2O) after BD |
76.31±25.62 |
|
|
Table 1 Mean, SD, % change and P value before and after bronchodilator(BD) reversibility test of FVC,FEV1,PEFR,MEP and MIP of asthmatics(n=35)
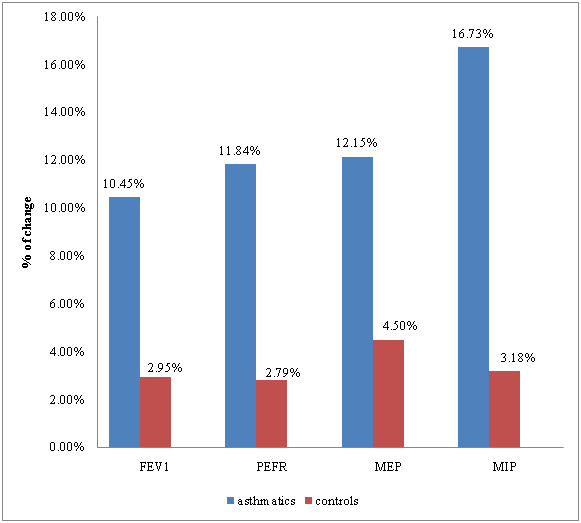
Figure 1 % of change in FEV1, PEFR, MEP and MIP after the bronchodilator in asthmatics and control subjects.
Type of asthma |
Sensitivity |
|
|
|
FEV1 |
PEFR |
MEP |
MIP |
|
Mild & intermittent |
29% |
29% |
43% |
67% |
Moderate& severe |
50% |
33% |
57% |
78% |
Table 2 Sensitivity of FEV1, PEFR , MEP and MIP reversibility testing in mild & intermittent asthma and moderate& severe asthma
The respiratory pressure meter measures the respiratory muscles power as a function of the air volume expired or inspired by effort.
In the present study of reversibility testing, significant increase was observed in lung function (FVC, FEV1 and PEFR) of asthmatic subjects compared to controls (non asthmatic) after bronchodilator test. Similar results were also obtained for MEP and MIP where significant increase in these parameters was observed in asthmatics after bronchodilator test. The greater percent of change in asthmatic subjects after reversibility testing has occurred in respiratory muscle pressures (MEP & MIP) more than lung function parameters in the present study. Eleven cases with FEV1 negative reversibility testing were found to be MIP positive for reversibility testing, however, 9 of these 11 cases were classified as mild and intermittent asthmatics. This implies that patients with negative reversibility testing of lung function could be diagnosed by respiratory muscle pressures reversibility testing even those with mild and intermittent asthma. MEP and MIP were found to be lower in patients with severe airway impairment than normal healthy subjects in a study conducted by Claudio Terzano et al.,12 The reduction in MEP and MIP was found to be lower in patients with slight reduction of FEV1.12
Asthma increases the work load on respiratory pump by causing increase in airway resistance, the inspiratory muscles bear the majority of this load whereas expiratory muscle recruitment is relatively minor.13 This is may explain in part the result that MIP increased more than MEP after bronchodilator test. Higher sensitivity of MEP and MIP reversibility testing in asthmatic subjects compared to that of FEVI and PEFR may imply that respiratory muscle pressures reversibility tests could be a potential sensitive test in diagnosis of asthma. Higher sensitivity of MEP and MIP reversibility test in intermittent and mild asthma may further imply that respiratory muscle pressures reversibility testing could be a better sensitive test in diagnosis of mild and intermittent asthma.
Further studies must also focus on broncho provocation tests of respiratory muscles power in asthmatics who had negative reversibility testing for further confirmation of the results obtained in our present study.
Respiratory muscles power reversibility test could be a potentially sensitive diagnostic test for asthma.
My research project was partially or fully sponsored by (Elsheikh Abdallah Elbadri University) with grant number (1,000$). In case of no financial assistance for the research work, provide the information regarding the sponsor.
This study was from the thesis of the degree of specialty in radiology (Project no. 96-01-01-14066) of Mohammad Javad Athari and supported by Shiraz University of medical sciences, Shiraz, Iran.
The authors declare that there is no conflict of interest.

©2019 Abdalla, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.