Journal of
eISSN: 2376-0060


Case Report Volume 11 Issue 1
1Department of Respiratory Medicine, National Hospital for Respiratory Diseases, Welisara, Sri Lanka
2Department of Cardio-thoracic surgery, National Hospital for Respiratory Diseases, Welisara, Sri Lanka
Correspondence: , Tel +94702614055
Received: February 16, 2024 | Published: February 28, 2024
Citation: Gunathilaka MDN, Bandara LMH, Handagala S, et al. Recurrent spontaneous pneumothorax in a patient with wilson disease who is on long-term D-penicillamine: Case report. J Lung Pulm Respir Res. 2024;11(1):15-17. DOI: 10.15406/jlprr.2024.11.00310
Introduction: Recurrent spontaneous pneumothoraces (PSP) in association with liver disease is well known to occur with alpha 1 antitrypsin deficiency (AATD). Wilson disease (WD) association with recurrent PSP is not a known entity.
Case presentation: A 42-year-old nonsmoker man with a history of recurrent PSP was admitted with a large right pneumothorax. Following intercostal chest drain (ICD) patient’s breathing improved and the lung expanded. Despite that, he continued to have a small residual pneumothorax (<2cm). Twelve years ago, he was diagnosed with WD. The patient was on treatment with D-penicillamine. After 3 years of the diagnosis of WD, the patient developed left-sided recurrent PSPs where he ended up with a left-pleurectomy in 2015. For the current event, initially expectant management was done for residual pneumothorax. All the possible causes for PSP were excluded. On follow-up, he continued to be symptomatic. A thoracic surgical referral was arranged for Video-Assisted Thoracoscopic Surgery (VATS) and redo-pleurectomy. The safety of future treatment with D-penicillamine is not concluded as there is no convincing evidence to prove it as a culprit agent for PSPs. Multidisciplinary discussion was arranged and consideration of treatment with alternative copper chelating therapy was emphasized.
Conclusion: Though rare, it is important to observe for occurrence of PSP in WD patients. This case report will be eye-opening for the association of lung disease and WD and related treatment.
Keywords: D-penicillamine, recurrent pneumothorax, wilson disease, case report
AATD, alpha-1 antitrypsin deficiency; FLAIR, fluid-attenuated inversion recovery; ICD, intercostal drainage; PSP, primary spontaneous pneumothorax; SLE, systemic lupus erythematosus; VATS, video assisted thoracoscopic surgery; WD, Wilson disease
Wilson disease (WD) is an autosomal recessive disorder with liver disease and neurological sequale. Well-known clinical manifestations include cirrhosis, neurological manifestations and renal manifestations.1 Lung diseases association with WD is sparsely reported in the literature. Treatment with D-penicillamine is high-profile to cause varied adverse events of the respiratory system including pleural-based diseases and rarely pleural effusions.2
Recurrent spontaneous pneumothoraces in association with either W or D-penicillamine have not been documented in the medical literature. In this case report we publish a very rare co-occurrence of recurrent PSP in a patient with WD.
A 42-year-old non-smoking male with a history of multiple spontaneous pneumothoraces (which had been treated with pleurectomy) was referred to our tertiary center with sudden onset difficulty in breathing and right-sided pleuritic chest pain. He was found to have a large right-sided pneumothorax managed initially with intercostal chest drain (ICD). Following the drain insertion, patient’s breathing improved and the lung expanded. Despite that, he continued to have a small residual pneumothorax (<2cm) (Figure 1a & b).
Twelve years ago, he was evaluated for tremors and ataxia where he was diagnosed to have WD with positive ATP7B gene homozygous mutation, very low serum ceruloplasmin level. Additionally, his MRI brain showed a giant panda sign and positive Kayser- Fleischer (KF) rings (Figure 2). Since then, the patient has been on treatment with D-penicillamine.
After three years the first diagnosis of WD, the patient developed left-sided recurrent PSPs (Figure 1c & d), where he ended up in video assisted thoracoscopic (VATS) guided left-side pleurectomy in 2015. Since then, he has been stable until the current presentation.
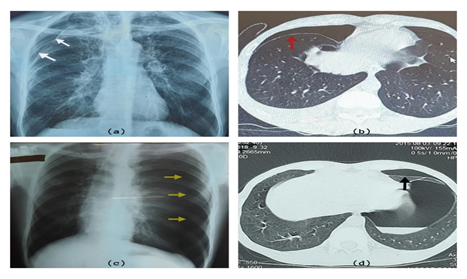
Figure 1 a & b illustrates the current presentation with right side residual pneumothorax in CXR (white arrows) and HRCT of the chest (red arrows). c & d -illustrate past-left sided pneumothorax in CXR (yellow arrows) and HRCT (black arrow).
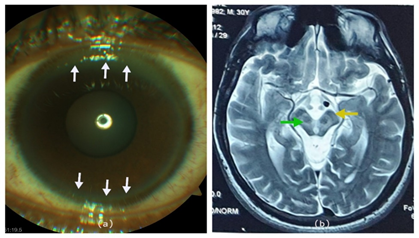
Figure 2 (a) White arrows indicate the KF rings of the anterior chamber of the eye. (b) MRI of brain fluid attenuated inversion recovery (FLAIR) image showing the face of a giant panda sign. The green arrow shows increased signal intensity in the midbrain, yellow arrow shows preservation of signal intensity of pars-reticulates of substantia nigra.
There was no similar history in the family and there was no evidence of significant exposures, neuro-cutaneous diseases, and interstitial lung diseases. He was a lifetime non-smoker and had not used any other substances.
Examination revealed normal vital signs, reduced chest expansion and absent breath sounds on the upper zone of right chest.
Immediate anteroposterior chest radiograph revealed right-side mild (<2cm) pneumothorax and high-resolution chest tomography revealed an uncomplicated right-side pneumothorax without associating sub pleural blebs, cystic/bullous lung disease. The parenchyma and the mediastinum were otherwise normal. His pulmonary function test was found to be normal. The results of routine blood investigations were essentially normal including retroviral screening.
Evaluation for possible causes of PSP workup was done including tuberculosis, Marfan syndrome, alpha 1 antitrypsin deficiency (AATD), Interstitial lung disease, neurocutaneous syndromes and cystic lung diseases.
As our patient was asymptomatic with residual small pneumothorax, initially expectant management was done. But on follow-up visits he continued to have no improvement, a thoracic surgical referral was arranged for video-assisted thoracoscopic surgery (VATS) and redo-pleurectomy. Safety of future treatment with D-penicillamine is not concluded in this patient as there is no convincing evidence to prove it as a culprit agent for PSPs. Multidisciplinary discussions with the treating neurologist, pulmonologist, patient and the family were arranged and consideration of treatment with alternative copper chelating therapy was emphasized.
Wilson disease, which is also known as hepatolenticular degeneration, is an autosomal recessive disorder with dysfunctional copper metabolism.3 ATP7B mutation is the primary pathology that cause dysfunctional biliary copper metabolism.4 As a result, free copper is accumulates inside the mitochondria of the liver, the limbus of the cornea, basal ganglia and kidneys.3 These will manifest as cirrhosis, KF rings, neuro-psychiatric manifestations, and renal tubular disorder.4
Co-existing liver and lung diseases is well known to occur in patients with AATD.5 Though, recurrent pneumothoraces in association with AATD has been reported in the literature, association with WD is not yet reported.5 The exact mechanism by which the pneumothorax occurs remains unclear.
D-penicillamine which is a chelating agent for copper, is a high-profile cause for various multisystemic side effects. By the immunosuppressive mechanism of action, it can cause blood dyscrasia, dermatitis, nephrotic syndrome, myasthenia gravis and systemic lupus erythematosus (SLE).6 Moreover, it is well known to cause respiratory system-related side effects such as bronchospasms,7 bronchiolitis obliterans,8 Good pasture’s syndrome and interstitial pneumonitis.9 D-penicillamine–induced SLE can be associated with pneumonitis, alveolitis and pleural effusions. However, very few cases of pleural-based diseases were reported with direct association to D-penicillamine.7 A single case has been reported with pleural effusion who has received twelve years of D-penicillamine treatment.2 However, in medicine, surprises might happen hence, meticulous evaluation is needed for identification of very rare associations.10,11
Our case demonstrates a very rare occurrence of recurrent pneumothoraces in a patient diagnosed with WD who is on long-term D-penicillamine therapy. To the best of our knowledge, this is the first case report with recurrent pneumothoraces in association to WD. D-penicillamine treatment causing pleural effusion after long term treatment has been described in the literature but pneumothorax association is not mentioned.2
This case would mark an eye opener for a rare association of recurrent spontaneous pneumothoraces either with temporal association to WD or penicillamine treatment. Therefore, we consider it as worth reporting of this rare association which will enlighten the future readers.
Given the rarity of recurrent pneumothoraces association with WD and usage of D-penicillamine, it is truly important to observe for occurrence of such complications in these group of patients. This case report will be an impressive observation for association of recurrent pneumothorax and WD.
We thank the patient for consenting to the publication of photographs and relevant data.
The authors declare that there is no conflict of interest regarding the publication of this paper.

©2024 Gunathilaka, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.