Journal of
eISSN: 2376-0060


Case Series Volume 8 Issue 3
1Department of Respirology, Western University, Canada
2Department of Internal Medicine, Western University, Canada
Correspondence: Fahad Alsulami, Respirology Fellow, London, Ontario, Canada
Received: August 05, 2021 | Published: September 2, 2021
Citation: Alsulami F, Dhaliwal I, Mrkobrada M, et al. Post Covid-19 organizing pneumonia: Case series for 6 patients with post-COVID interstitial lung disease. J Lung Pulm Respir Res. 2021;8(3):108-111. DOI: 10.15406/jlprr.2021.08.00261
Organizing pneumonia secondary to viral infection is well established entity in the literature. Here we describe 6 cases of organizing pneumonia secondary to COVID-19. All six cases were presented with respiratory symptoms after their initial COVID-19 infection, and they had CT changes compatible with organizing pneumonia. Steroid treatment was initiated in all cases empirically without the need for trans-bronchial biopsy. All presented cases showed significant improvement with steroid clinically and radiographically.
Keywords: COVID-19, organizing pneumonia, systemic glucocorticoids, viral pneumonia, interstitial lung diseases
OP, organizing pneumonia; PCR, polymorase chain reaction; GGO, ground-glass opacities; ICU, intensive care unit
A 71-year-old male with past medical history significant for coronary artery disease, hypertension, and dyslipidemia presented with a 10-day history of fever, cough with non-purulent sputum, and loss of smell sensation. On the first admission, he presented with a blood pressure of 128/86 mmHg, temperature of 37.1°C, pulse of 120 bpm, and oxygen saturation of 89% while resting on room air. Laboratory data revealed serum LDH (250 U/L), leukocytes (8.4 x10*9/L), and C-reactive protein (CRP) (30.4 mg/L). Lymphopenia and coagulopathy were not observed. Chest X-ray (CXR) revealed evidence of air space disease predominantly distributed in the subpleural regions of the left lower lung zone (Figure 1a). Then the patient was diagnosed with COVID-19 and was treated with Remdesivir for 4-days, Dexamethasone for 10-days, and Amoxicillin/Clavulanic Acid for 7-days. During hospital admission, he continued to improve clinically, and his oxygen requirement decreased to 2 L/min oxygen via nasal cannula. All microbiological studies were negative, including sputum, blood, and urine. On day 8, the patient was discharged home, completing his few remaining days of oral steroids, with close follow-up in the outpatient COVID assessment clinic.
During his outpatient assessment, 2 weeks later, he complained of a 2-days history of fever (38.6°C), worsening dyspnea, cough, prompting re-admission to the hospital 2 weeks after discharge. He was able to titrate off his supplemental oxygen originally, but recently noticed an increased nasal cannula oxygen requirement up to 5 L/min oxygen when his symptoms reappeared. Upon re-admission, microbiological re-examination, including sputum and blood cultures, were negative in addition to a negative COVID-19 real-time PCR which was repeated. His CXR revealed peripheral lung consolidation and reduced lung volumes (Figure 1b). Further, his chest CT scan revealed extensive subpleural ground-glass attenuation distributed in both lung regions with evidence of increased interstitial lung markings and volume loss of the lower lobes (Figure 1c-1e). The patient’s clinical presentation and radiologic findings were compatible with organizing pneumonia (OP). He was started on dexamethasone daily dose of 6 mg (equivalent to prednisone 0.5mg/kg/day). After 2-days of steroid therapy, his fever and respiratory condition greatly improved, and his oxygen requirement decreased to 2 L/min oxygen via nasal cannula. The patient was discharged after 4-days with a plan to continue dexamethasone for four weeks. During outpatient clinic assessment on day 17 after discharge, the patient reported significant respiratory improvement and more exercise tolerance. His home reading of oxygen through pulse oximeter revealed oxygen saturation of 95% on room air at rest and 90% after moderate ambulation. Chest imaging on day 17 during the clinic visit revealed improvement of lung volume and infiltrate (Figure 1f). Dexamethasone was slowly tapered without complication or disease recurrence so far.

Figure 1 (a) Initial chest X-ray during COVID infection. (b) First chest X-ray during the second presentation shows multifocal airspace disease. (c,d,e) Different cuts of the CT chest showes peripheral dense GGO. (f) Chest X-ray after steroid treatment showed improvement of the airspace disease.
Case 2
54-year-old male nurse, with a past medical history only significant for hypothyroidism requiring levothyroxine 75 mcg daily. He presented to the emergency department with a 9-days history of progressive shortness of breath, cough, fever, and chills. Examinations were carried out during the Emergency Room visit and revealed a blood pressure of 88/64 mmHg, temperature of 39.4 °C, pulse of 91 bpm, and oxygen saturation of 93% on 5 L/min oxygen via nasal cannula. Laboratory data revealed leukocytes (6.9 x10*9/L) with lymphopenia (0.7 x10*9/L) and CRP was 344 mg/L. Arterial blood gas analysis showed PaO2 was 49 mmHg under an oxygen mask with FiO2 of 85%. CXR revealed increasing bilateral multifocal parenchymal consolidation (Figure 2a). Further, his CT chest revealed extensive peripheral bilateral multilobar consolidation (Figure 2b).
The patient was transferred to the intensive care unit (ICU) with hypoxic respiratory failure supported with humidified High Flow Oxygen via nasal cannula (HFNC) (FiO2 85%, 50L). Upon testing for a fourth time, his PCR returned positive for COVID-19. Other microbiologic data, including sputum, blood, and urine cultures, were negative. During ICU stay, the patient received antimicrobial coverage with vancomycin and piperacillin-tazobactam for 5 days. The patient was doing self-proning on a daily basis while in ICU, and he did not require intubation.
High flow oxygen via nasal cannula (HFNC) was weaning off on day 12 (the time of HFNC supporting was 11 days) when his oxygen requirement was decreased with a minimal radiographic improvement on his chest X-ray (Figure 2c). The patient was then transferred to the floor, and he was clinically improving. The patient was discharged home after 15-days of total hospital stay with transient home oxygen of 2L via nasal cannula.
During virtual follow-up with the patient it was noted that he was still having ongoing hypoxia and worsening dyspnea on exertion despite considerable interval improvement on his chest x-ray (Figure 2d). The chest CT on day 11 post-discharge shows new bilateral GGO with aggravating consolidation on new areas with scarring (Figure 2e), compatible with OP. Oral dexamethasone 8 mg daily (equivalent to prednisone of 0.5 mg/kg/day) was started. Within a few days his clinical symptoms improved, and by 8 weeks, significant clinical improvement was observed, and repeated CT chest 8-weeks after “resuming” steroids revealed obvious remission and absorption of the patchy GGO and scarring changes (Figure 2f). The dexamethasone dose was gradually tapered off with no complications or recurrence of the disease.
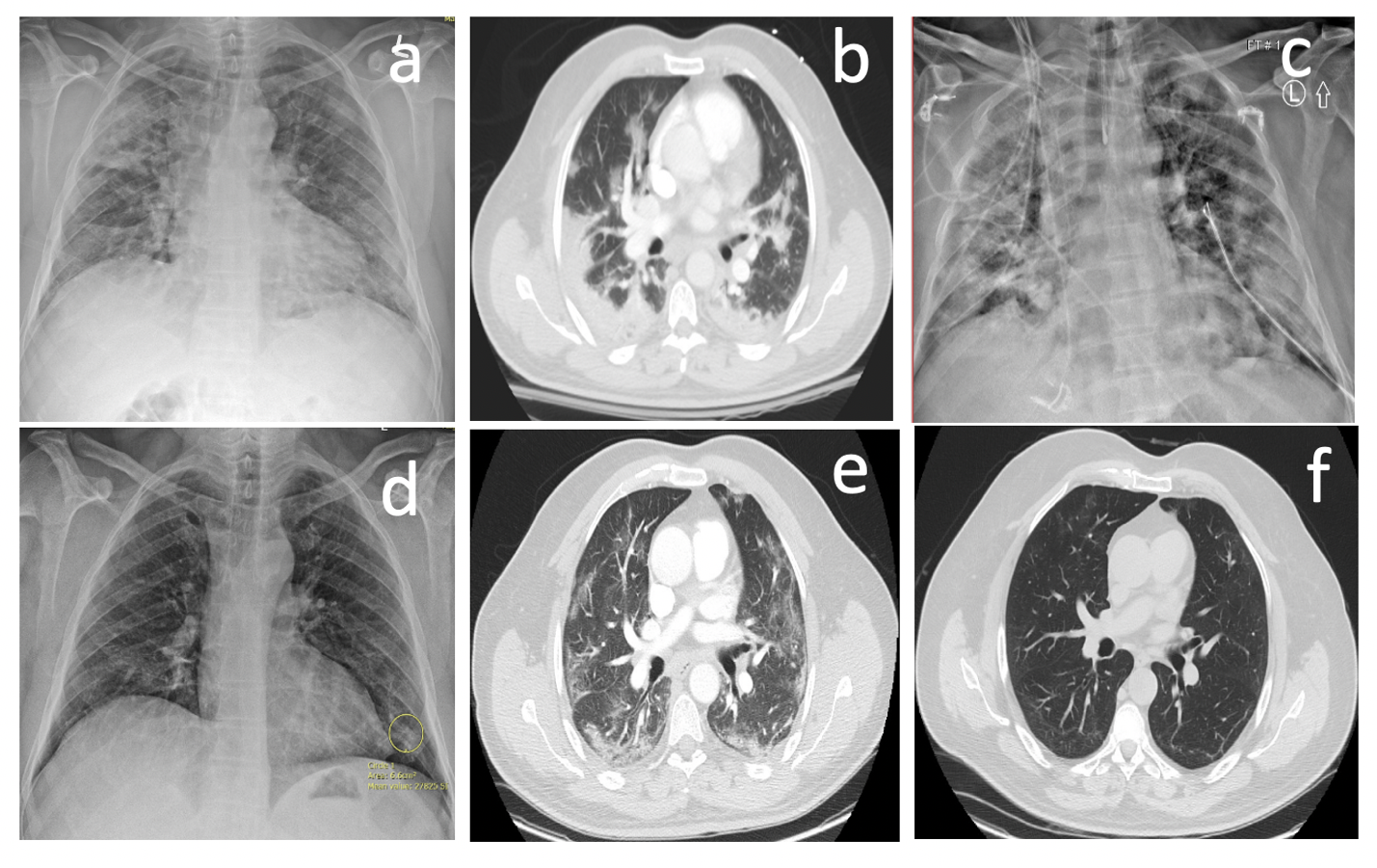
Figure 2 (a) Initial chest X-ray during COVID infection shows multifocal airspace disease. (b) CT-Chest shows peripheral dense GGO. (c) Chest X-ray shows extensive multifocal airspace disease. (d) Chest X-ray after steroid treatment showed improvement of the airspace disease. (e,f) Repeated CT-chest during the steroid course shows resolution of the GGO.
Case 3
A 57-year-old male with a previous history of only left bundle branch block, without medication presented to the Emergency Department with a 7-days history of headaches, fevers, dyspnea, and chills. The patient worked on a farm where there was a COVID-19 outbreak and he was found to be positive for COVID-19. On day 5, a CXR revealed bilateral progression of multifocal airspace opacities (Figure 3a). On the same day, the patient was intubated because of rapidly deteriorating respiratory symptoms and increased oxygen requirement. While on mechanical ventilation, the patient received dexamethasone for 10-days. Further, re-examinations of sputum were positive for pan-sensitive Streptococcus pneumonia, so he was treated with a full course of antimicrobial agent.
The patient’s oxygen requirements improved, and he was eventually extubated after 28 days of mechanical ventilation. However, after extubation, the patient still required oxygen through high flow oxygen via nasal cannula (HFNC), and he was noted to be persistently tachypneic. This picture persisted for 1-week post-extubation. Repeated real-time PCR for the COVID-19 virus was tested and revealed continuous negativity. CT chest with contrast showed no evidence of pulmonary embolism but extensive bilateral ground-glass opacities with associated diffuse alveolar damage (Figure 3b-3c), compatible with OP. The patient was started on prednisone of 0.5 mg/kg/day daily. The patient was transferred to the medical floor after 3-days of steroid with significant respiratory improvement and decreased oxygen requirement to 2 L/min oxygen via nasal cannula. One week later, the patient was discharged to home with stable clinical conditions, and his oxygen saturation was 90% on room air.
During clinic visit 8-weeks after discharge, the patient reported improving respiratory condition. His blood gas analysis on room air showed PaO2 of 70%. Repeated CT chest revealed significant improvement of previously noted peripheral GGO (Figure 3d-3e). The steroid was gradually tapered and stopped with no complications or recurrence of the disease.
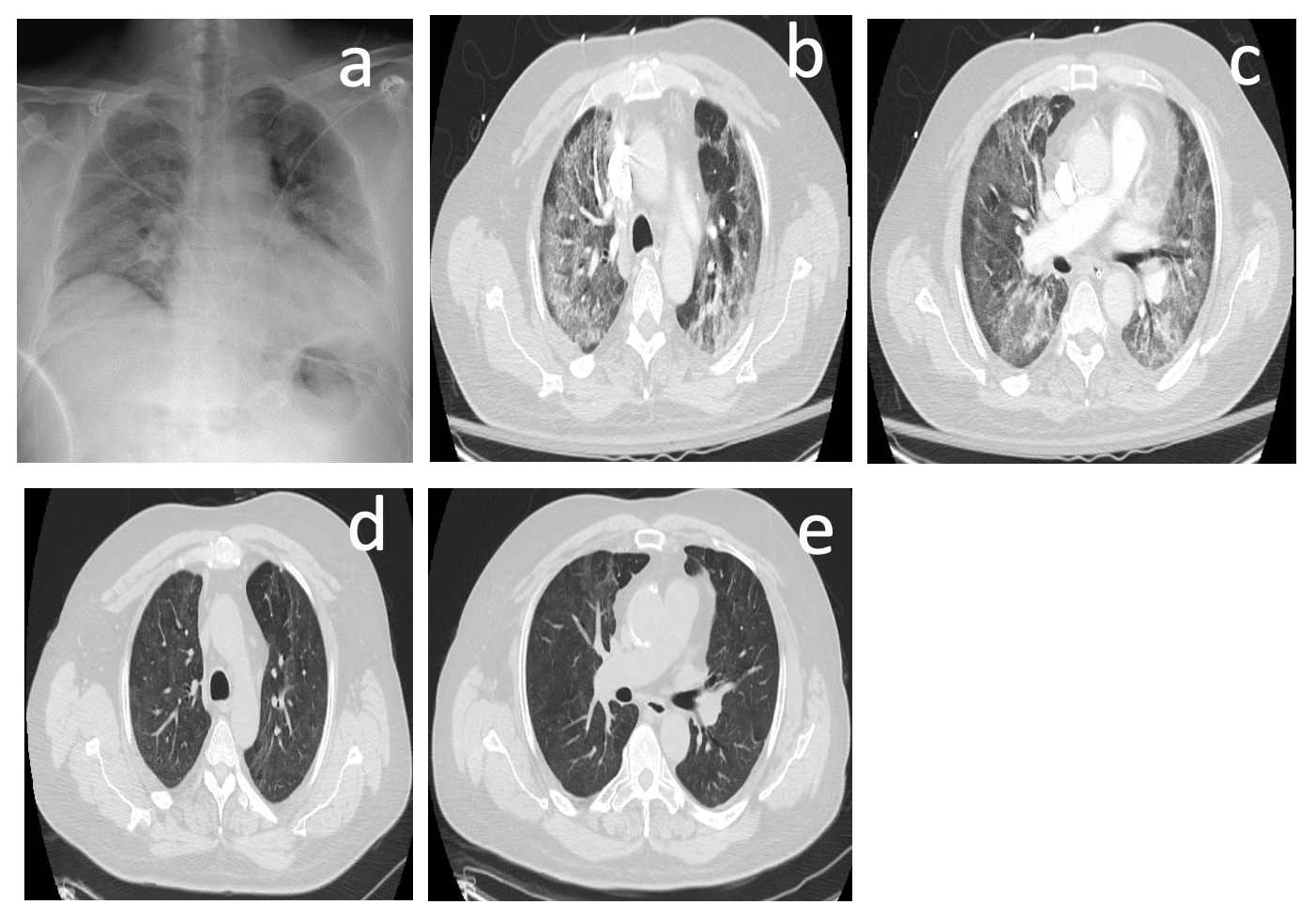
Figure 3 (a) Initial chest X-ray during COVID infection shows multifocal airspace disease. (b,c) CT-Chest shows peripheral dense GGO. (d,e) CT- Chest during the steroid treatment revealed complete resolution of the GGO.
Case 4
A 56-year-old female patient not known to have any medical illness. the patient was tested positive for COVID-19 six days prior to the presentation to the clinic. She presented to the clinic with persistent respiratory symptoms including shortness of breath, cough, myalgia, loss of smell and taste sensation and headache. Also, she was found to be hypoxic during physical examination with oxygen saturation of 88% on room air. The patient was started on dexamethasone 10mg orally. During clinic follow-up assessment, the patient was found to have persistent dyspnea and hypoxia despite steroid treatment. On day 16 of her illness CT chest was requested and revealed subpleural reticulation with peripheral (Figure 4a). This radiographic changes and persistent respiratory symptoms were concerning for possible OP. The patient was treated with prolonged steroid course with Dexamethasone. She completed 4 weeks of dexamethasone with planned tapering dose. She had complete resolution of her respiratory symptoms and hypoxia. Repeated chest x-ray six weeks after steroid treatment was normal with no evidence of airspace or interstitial lung disease (Figure 4b).
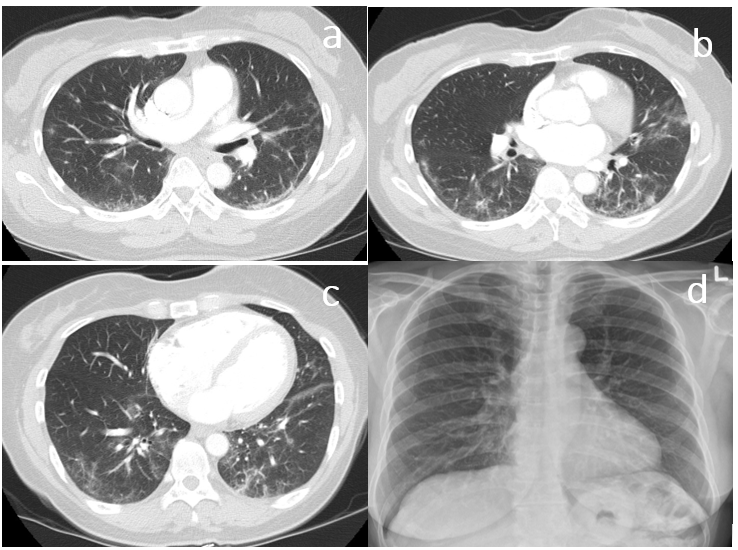
Figure 4 (a,b,c) Parenchymal changes including subpleural reticulation, ground-glass opacity and consolidative opacities. (d) Chest x-ray shows no evidence of airspace or interestitial lung disease.
Case 5
A 49-year-old male patient known case of diabetes, dyslipidemia and GERD. He was admitted to the hospital with significant respiratory symptoms of shortness of breath, cough, pleuritic chest pain and hypoxia. Initial laboratory pork up revealed positive COVID-19 infection and his initial chest x-ray revealed bilateral ill-defined opacities (Figure 5a). CT scan during admission revealed diffuse extensive bilateral ground glass opacities with no evidence of pulmonary embolism (Figure 5b). The patient was started on steroid (dexamethasone 10mg orally daily) for a total of 10 days. He was discharged from the hospital after 10 days of total hospital admission with home oxygen of 2L nasal prongs. During clinic follow up on day 15 as an outpatient, the patient was noted to have persistent hypoxia despite negative COVID 19 test and persistent opacities on the chest x-ray (Figure 5c). CT pulmonary angiogram was arranged for the patient to rule out pulmonary embolism and to evaluate his lung parenchyma. The result of the CT scan was positive for pulmonary embolism and new evidence of peripheral diffuse lung opacities different in distribution and densities compared to the previous CT scan (Figure 5d). Based on the CT scan appearance and clinical picture, the patient was started on anticoagulation as well as extended duration of steroid aiming to treat possible organizing pneumonia. Clinic assessment after one month of steroid initiation revealed significant respiratory improvement and oxygen saturation was maintained on rome air. Repeated CT scan after one month showed interval resolution of the previously noted peripheral GGO (Figure 5e). Another follow-up CT scan after two months showed complete resolution of the GGO (Figure 5f).
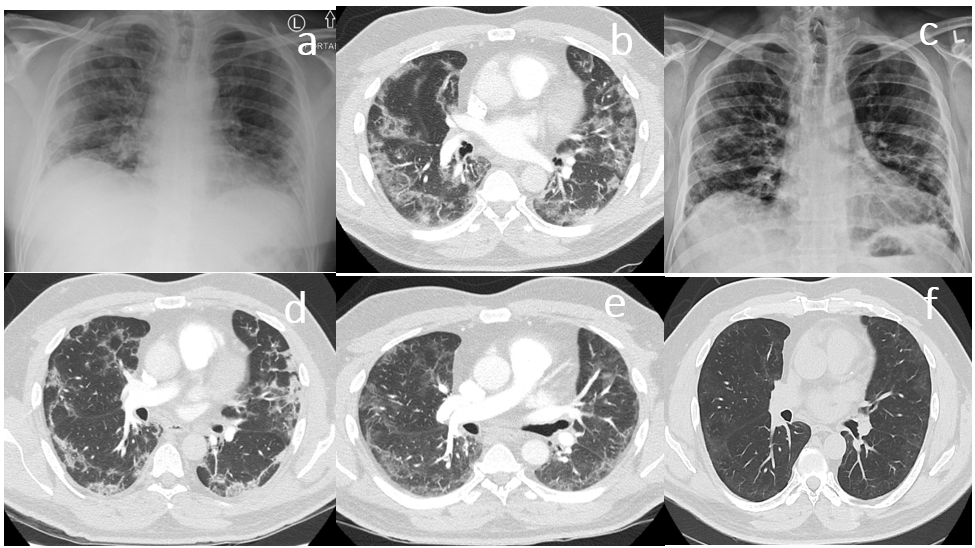
Figure 5 (a) Initial chest X-ray during COVID infection shows multifocal airspace disease. (b) CT-Chest shows peripheral dense GGO. (c) Repeated chest x-ray shows persistent bilater airspace disease. (d) CT-chest shows dense bilateral GGO. (e) CT-chest shows improvement of the GGO. (f) CT-Chest shows complete resolution of the GGO.
Case 6
An 83-year-old female patient known case of diabetes and coronary artery disease. The patient was tested positive for COVID-19 and presented to the hospital 10 days after onset of symptoms with persistent dyspnea and chest pain. She was admitted to the hospital and her initial work-up revealed an evidence of new LBBB and chest x-ray showed bilateral airspace opacities (Figure 6a). The patient was discharged home with supplemental oxygen and completed a 10-days course of dexamethasone as outpatient. During outpatient clinic assessment three weeks after discharge, it was observed that the patient still continues to have persistent dyspnea and oxygen requirement despite full course of dexamethasone treatment her documented oxygen at home Spo2 93% on 2L nasal prongs. CT chest was arranged and revealed bilateral subpleural reticulation with no evidence of pulmonary embolism (Figure 6c-6d). She was started on prednisone (0.5mg/kg/day) aiming to treat possibility of OP. After three weeks of steroid treatment, the patient reported significant clinical improvement and her documented oxygen SpO2 was 97% on room air. The prednisone dose was gradually tapered off with no complications or recurrence of the disease.
Herein, we present 6 patients with rapidly progressive respiratory symptoms following initial presentation with covid-19 infection. The patients’ presentations are consistent with that of OP secondary to viral infections in several aspects. All patients presented with rapidly progressive worsening respiratory symptoms after initial therapy for their COVID infection. Interestingly, all patients relatively quickly after their initial infections, but were managed in 3 different settings (ICU, medical ward, outpatient). These patients also had PCR sero-conversion of covid-19 detected by real-time PCR. Furthermore, their microbiologic data did not reveal any significant superimposed infection in five out of six patients. Moreover, they had significant improvement after starting steroids, which further suggests Organizing pneumonia as an etiology for their decompensated respiratory symptoms.
Generally, OP can be classified into an idiopathic form (cryptogenic OP) and secondary organizing pneumonia with no major differences in clinical presentation between both forms.1 Organizing pneumonia secondary to viral infection is a very well established entity in the literature. It has been described in patients with MERS-CoV, influenza B, and H1N1.2-4
Corticosteroids are considered the mainstay of treatment for patients with organizing pneumonia, with evidence of complete recovery in up to 80% of patients within a few weeks to 3 months.5
To the best of our knowledge, there is minimal data in the literature, mostly from an autopsy, reporting diffuse alveolar damage (DAD) or acute fibrinous and organizing pneumonia (AFOP) in patients with covid-19.6 In contrast, a recent radiological retrospective study that looked into the radiographic patterns of OP in patients with covid-19 showed pure GGO in (32.2%), mixed GGO and consolidation in (21.2%), and consolidation with linear opacity in (17.7%).7 Moreover, There is a recent observational study that looked into persistent post-COVID inflammatory lung chanages and reported ongoing symptoms in 39% of the patients. Interstitial Lung disease, predominately OP, were observed in 4.8% of that cohort with signfocant radiographic and symptomatic imrovement following steroid treatment.8
It is well known that not every case of OP is supported by pathological evidence. The main role of a biopsy in patients with suspected OP is to identify other potential etiologies with similar disease presentation. The histopathologic features of organizing pneumonia can be observed in other interstitial lung diseases, so reliance on transbronchial biopsies may increase the likelihood of delaying or misdiagnosis of OP. Besides, radiographic features of organizing pneumonia are characteristic, and the diagnostic accuracy of CT for organizing pneumonia is high (79%).9
In conclusion, The diagnosis of OP secondary to COVID-19 needs a combination of both clinical and radiological expertise in the appropriate clinical context. If the scenario is not typical, a lung biopsy is required for histopathologic correlation. Additionally, more studies are required, including randomized control trials to improve further our understanding of organizing pneumonia secondary to viral infection like COVID-19.
None.
Authors have no conflict of interest to declare.

©2021 Alsulami, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.