Journal of
eISSN: 2376-0060


Case Report Volume 3 Issue 6
1Department of Medical Education, Southeastern Regional Medical Center, USA
2Southeastern Regional Medical Center, USA
Correspondence: Andres Endara-Bravo, Southeastern Regional Medical Center, Southeastern Pulmonary and Sleep Clinic, 401 West 27th Street Lumberton, NC 28358, Tel 910-674-519, Fax 910-272-7155
Received: July 15, 2016 | Published: December 28, 2016
Citation: Plum M, Pfirman K, Endara-Bravo A. Lacrimal duct air regurgitation in an adult patient on continuous positive airway pressure therapy. J Lung Pulm Respir Res. 2016;3(6):173–174. DOI: 10.15406/jlprr.2016.03.00107
Continuous Positive Airway Pressure (CPAP) is indicated of Obstructive Sleep Apnea (OSA) but has been associated with a variety of complications. We describe a patient who experienced lacrimal duct air regurgitation (LDAR) requiring discontinuation of CPAP. While this has been previously reported in patients with a Lester-Jones tube and in CPAP forums, we discuss an alternative treatment using a Mandibular Advancement Device (MAD) to treat OSA in a patient with lacrimal duct air regurgitation.
A 52-year-old Caucasian female with no significant history was diagnosed with moderate OSA with an Apnea-Hypoxia Index (AHI) of 16, requiring CPAP at 10 cm H20. During the initial night of CPAP therapy, the patient complained of air regurgitation through the right eye that was associated with morning scleral injection and xerophthalmia. Symptoms resolved after discontinuing CPAP therapy.
The patient recalls having air regurgitation while sneezing and blowing her nose since her childhood, but this has not caused major ophthalmologic problems prior. Past medical history was negative for ophthalmologic surgeries. Physical examination revealed normal vital signs along with a Body Mass Index (BMI) of 34.4 kg/m2. External eye examination was unremarkable.
Despite a decrease in CPAP pressure and a change from a nasal mask to a full-face mask, air regurgitation was not alleviated. A MAD successfully treated her OSA. Follow-up Home Sleep Test with MAD showed an AHI of 3.
The pathophysiology of LDAR is explained by the positive pressure created in the upper airways that is exaggerated with CPAP. This occurs by forcing air into the nasolacrimal duct through the inferior meatus in patients with abnormal valves including the valves of Beraud, Taillefer, Rosenmuller, and/or especially Hasner (Figure 1).1 Valve insufficiency may be due to embryological defects and/or agenesis during development that are usually completed in the eighth month of gestation.2 There may also be an effect of LDAR increasing the evaporation of the secretions resulting in alteration of the tear composition, xeromyceria, and desiccation of the epithelium of eye.1 This disrupts the lacrimation dynamics resulting in xeropthalmia.1
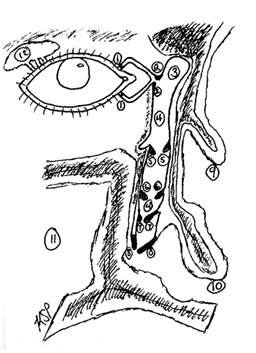
Figure 1 Anatomy of the Lacrimal System.
1. Valve of Foltz 2. Valve of Rosen Muller 3. Lacrimal sac 4. Nasolacrimal duct 5. Valve of Beraud (Krause) 6. Valve of Hyrtl 7. Valve of Taillefer 8. Valve of Hasner 9. Middle Concha (Turbinate) 10. Inferior Concha (Turbinate) 11. Maxillary Sinus 12. Orbital and palpebral component of lacrimal gland.
The use of CPAP is indicated for the treatment of OSA.3 Many studies have previously reported complications associated with CPAP for treatment of OSA. Ocular complications related to CPAP for treatment of OSA include: floppy eyelid syndrome, ocular irritation, abnormal tear break-up, increased upper and lower lid laxity, and conjunctivitis.4
To date, there have been similar complications cited in patients whom have undergone conjunctivodacrocystorhinostomy and dacryocystorhinostomy using Lester-Jones tube insertion and silicone stent deployment, and in one child, using nasal continuous positive airway ventilation for respiratory support in neuromuscular disorders requiring considerably higher pressure than those needed for OSA treatment.5,6
Several online CPAP forums discuss individual reports of LDAR. LDAR was described as a feeling of air leaking through the tear duct, audible air bubbling under the eyelid, air trapped under the eyelid, and air circulating around the eye when the eyelids are closed. LDAR was associated with self-reported frequent awaking throughout the night and decreased compliance with PAP therapy. A variety of solutions were offered based on personal success and failures in treating LDAR. Treatment included switching from a nasal mask to a full mask, although some people noted worsening with full mask, and using a Valsalva maneuver which allowed temporary relief.
Usage of an oral device such as a MAD has not previously been reported in the treatment of OSA with LDAR on CPAP. Interventions including reducing CPAP, switching to variable pressure and using barrier ointment were ultimately unsuccessful in a limited number of patients with either Lester-Jones tube or prior dacryocystorhinostomy.
Patients with newly diagnosed OSA and patients who do not tolerate CPAP should be questioned about previous ophthalmic/ENT procedures and a history of LDAR. Patients should be screened for LDAR with valsalva maneuvers prior to starting PAP therapy. Early recognition of LDAR can increase compliance with treatment for OSA with reasonable alternative therapies such as a MAD.
None.
The author declares no conflict of interest.

©2016 Plum, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.