Journal of
eISSN: 2376-0060


Case Report Volume 11 Issue 1
Department of Chest Diseases, Bartın State Hospital, Türkey
Correspondence: Aytekin İdikut, Bartın State Hospital, Tuna Mahallesi 846. Cadde No:15 74100, Turkey, Tel +90 539 879 23
Received: March 10, 2024 | Published: March 25, 2024
Citation: Aytekin I. Inheritance from the past: Chronic calcific empyema. J Lung Pulm Respir Res. 2024;11(1):27-29. DOI: 10.15406/jlprr.2024.11.00313
Introduction: Fibrothorax, characterized by the widespread thickening of the pleura, can develop as a result of several disorders and can be seen as a consequence of empyema. After a very long latent period, reactivation or infection may occur. Hemothorax, empyema, asbestos exposure, and tuberculosis are frequent etiologies. This can occur frequently with bronchopleural fistula or pleurocutaneous fistula. In our article, we will present a case with a stable lesion containing fluid between calcified pleural sheets for many years, but a fistula has not yet developed, and recurrent hospital admissions with vague clinical findings.
Case presentation: A 96-year-old man patient was admitted due to experiencing difficulty in breathing. He has been diagnosed with hypertension and heart failure and does not have a history of regular drug usage. According to his medical records, he had pulmonary tuberculosis around 65 years ago. He has been experiencing a chronic cough, expectoration of mucus, and dyspnea for approximately two decades. He received oral antibiotic treatments, but as his symptoms began to improve, he did not attend follow-up appointments. Upon reviewing the patient's past examinations, it was observed that thoracic CT scans conducted in 2010, 2022, and 2024 revealed the presence of pleural thickening, areas with fluid density, and calcifications in the right hemithorax. Additionally, areas with fluid density were consistently observed within the stable calcific mass lesion throughout this period. A close clinical monitoring protocol was instituted due to the patient's refusal to undergo thoracentesis, stable lung imaging for 14, and normal acute phase reactants and sputum cultures.
Conclusion: In chronic calcified pleurisy, which is evaluated in favor of sequelae in patients with appropriate history and clinical findings, the etiology should be clarified by informing the patients, and treatment options should be evaluated without further degrading the patient's clinical.
Keywords: tuberculous empyema, chronic calcified empyema, fibrothorax, pleural diseases
Fibrothorax, characterized by widespread thickening of the pleura, can result from a variety of disorders and may be seen as a consequence of empyema.1,2 Tuberculous empyema is identified by the presence of a thick pleural structure that is densely and irregularly calcified.3 This calcification occurs in both the parietal and visceral pleura, which surround a localized collection of pleural fluid. This fluid often contains a large number of tuberculosis bacilli. Following a prolonged period of inactivity, there is a possibility of reactivation or infection. This scenario can often arise with bronchopleural fistula or pleurocutaneous fistula.3,4 Our paper will discuss a case involving a long-standing stable lesion that contains fluid between calcified pleural sheets. Despite the absence of a fistula, the patient has experienced multiple hospital hospitalizations with unclear clinical symptoms.
A 96-year-old male patient presented at the outpatient clinic with dyspnea. There was no accompanying cough and sputum. There were no occurrences of night sweats or weight loss. The patient was a rural resident who worked as an animal husbandry professional. An assessment of the patient's medical records revealed that approximately 65 years ago, he was diagnosed with pulmonary tuberculosis.
The duration of his anti-tuberculosis treatment and the specific medications he got remain unknown. He has a smoking history of 20 packs per year, has been smoke-free for 35 years, and abstains from alcohol consumption. He had hypertension and heart failure, but the patient had no history of regular drug use. He has been having frequent coughs, phlegm and shortness of breath for about 20 years. He was given oral antibiotic treatments, but when his complaints started to regress, he did not go for follow-up examinations. He used oral antibiotics 4 times in the last year, and hospitalization was recommended once, but the patient did not accept it. Looking at the patient's retrospective examinations, pleural thickening, areas containing fluid density, and calcifications were observed in the right hemithorax in the Thorax CT scans taken in 2010 and 2022 (Figures 1 & 2). In the CT scan of the patient taken in January 2024, approximately 3,5 cm was observed on the right hemithorax, which could be evaluated in favor of pleurisy sequelae (Figures 3 & 4). Sputum analysis for three Acid-resistant bacilli tests was negative. There is no elevated sedimentation, CRP, or leukocytosis.
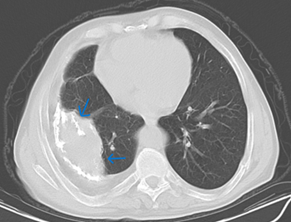
Figure 1 Mediastinal window of March 2010 thorax CT showing a calcified pleural empyema, first CT in the patient's medical history.
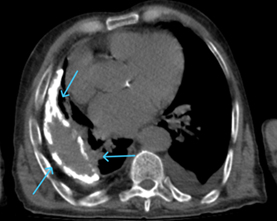
Figure 2 Mediastinal window of April 2022 thorax CT, the lesion structure remained stable and became more calcified.
An intensive inflammatory response produces fibrothorax typically caused by a complicated undrained pleural effusion. As a consequence, there is fibrin deposition between the pleural surfaces and, in certain cases, the visceral and parietal pleura fuse to form a solitary layer of fibrous tissue, which is frequently calcified. The development of fibrothorax may give rise to recurring or persistent fluid retention. Lung expansion becomes challenging, and atelectasis may ensue as a consequence. Intercostal spaces may become constricted, the mediastinum is drawn toward the developing fibrothorax, and the volume of the affected hemithorax decreases.
The presence of restrictive type disorder can be detected through respiratory function assessments. The most common causes of fibrothorax are hemothorax, tuberculous pleurisy and complicated parapneumonic effusion/empyema. Additionally, asbestos exposure, collagen vascular disease, drug-induced pleuritis, therapeutic pneumothorax, and pleurodesis may all contribute to its development. Tuberculous empyema represents a chronic, active infection of the pleural space containing large numbers of tuberculosis bacilli. Depending on the extent of inflammation, the infection's severity and activity may differ. The inflammatory process can persist for years without manifesting any clinical symptoms.
Typically, patients are identified through routine chest radiography examinations or subsequent to the occurrence of bronchopleural fistula or empyema. On computed tomography, the presence of dense, calcific pleural thickening encircling loculated pleural fluid raises suspicions regarding the diagnosis of tuberculous empyema. Pleural fluid is acid-fast bacilli-positive. Pleural space drainage and antituberculous drug therapy comprise the treatment. Obstacles to treatment include the inability to achieve therapeutic drug concentrations in the pleural fluid, which can result in drug resistance, and the inability of the lung to expand despite surgery.1,2,4–6
In chronic calcified pleurisy, which is evaluated in favor of sequelae in patients with appropriate history and clinical findings, the etiology should be elucidated, and treatment options should be assessed without causing the patient's clinic to deteriorate. Assessing patients without seeing previous radiological images can result in inaccurate diagnostic procedures and result in time wastage in patient care.
A calcific empyema that has been stable for years should be carefully considered in terms of potential consequences, such as bronchopleural fistula. The article highlights that chronic calcific empyema, a condition that is infrequently encountered in clinical settings, can frequently be mistaken for acute empyema and parapneumonic effusion with circumstances where prompt diagnostic choices are required, such as emergency rooms and critical care units. It is important to compare radiological findings with any previous imaging, if available, and make decisions on an individual basis for the accurate diagnosis and treatment approach.
Thanks to the patient for consenting to the publication of photographs and relevant data.
The author declares that he has no conflict of interest.
None.

©2024 Aytekin. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.