Journal of
eISSN: 2376-0060


Case Report Volume 10 Issue 2
1Allergology C Department, Tunis El Manar University, Tunisia
2Surgery Department, Ariana, Abderrahman Mami Hospital, Tunis El Manar University, Tunisia
3Department of Epidemiology and Statistics, Hbib Thameur Hospital, Tunisia
Correspondence: Amani Ben Mansour, Allergology C Department, Abdurrahman Mami Hospital, 1080 Ariana, Tunisia
Received: April 27, 2023 | Published: May 8, 2023
Citation: Mansour AB, Khzami NE, Saad SB, et al. A rare presentation of multifocal tuberculosis in an immunocompetent patient. J Lung Pulm Respir Res. 2023;10(2):31-33. DOI: 10.15406/jlprr.2023.10.00298
Introduction: Multifocal tuberculosis (MT) is an uncommon presentation in immunocompetent patients. It’s associated more with an immune-depression like Human Immunodeficiency Virus infection. We report a case of MT with presternal cold abscess, mediastina and cervical adenopathy, bone, and vertebral location that occurred in an apparently immunocompetent patient.
Case presentation: A 19-year old woman with no previous history of tuberculosis (TB) exposure was admitted for chronic chest pain lasting for 13 months. She presented with a history of fever, night sweat and weight loss (09 kg). The first clinical examination noticed a voluminous presternal abscess. The chest X-Ray showed an enlargement of the middle mediastinum associated to pleural effusion opacity, but any active pulmonary lesions. A computed chest tomography revealed the presence of a parietal mass centered on the sternum, with extension in the soft parts, bone lies of the sternal manubrium, lies of the vertebral hemi-bodies of T10 and T11, cervical lymph nodes, phrenic mediastina and sub-pectoral nodes with peritoneal and mesenteric involvement. Magnetic resonance imaging of the spine showed tiered thoracic lumbar and sacral spondylitis with paravertebral and anterior epidural collections responsible for spinal cord compression next D10 without signs of spinal cord pain. The draining of the cold abscess revealed some whitish pus, in which acid-alcohol resistant bacilli were identified. There was no history of diabetes, renal failure, or long-term treatment with corticosteroids or immunosuppressant’s: HIV serology and viral hepatitis were negative. The blood glucose was normal. The patient was treated with anti-tuberculosis regimen based on: Ethambutol, Rifampicin, Isoniazid, and Pyrazinamide for two months, and then rifampicin and isoniazid for seven months. The outcome was good with the disappearance of the abscess and all the radiological signs. Conclusion: Multifocal TB such as the case reported are uncommon and confined mostly to immunocompromised patients especially those with HIV infection. Because of the clinical polymorphic features of multifocal TB, the diagnosis is usually difficult to make, resulting into delay before beginning of the adequate treatment.
Keywords: tuberculosis, multifocal tuberculosis, immunocompetent, osteoarticular tuberculosis
Tuberculosis (TB) is a major cause of morbidity and mortality in many countries.1,2 Human Immuno deficiency Virus (HIV) infection, malignancy, transplantation, chronic diseases, and aging are immunosuppressive conditions, leading to the increase of the disease.3,4 Tuberculosis may have atypically presentation that causes delays in diagnosis and treatment.5 Multifocal tuberculosis in immunocompetent patients is uncommon. We report an unusual case of multifocal osteoarticular and paravertebral tuberculosis involving skin, soft parts, cervical lymph nodes, mediastinal nodes, and peritoneal tuberculosis in an immunocompetent patient.
Case presentation
A 19-year-old woman without relevant pathological history and with no previous history of tuberculosis (TB) exposure was admitted for chronic chest pain lasting for 13 months. She presented with a history of recurrent vesper fever of 38 degrees, night sweat and weight loss (09 kg). There was no history of a chronic cough. The first clinical examination noticed a voluminous presternal abscess. Examination of the respiratory system was normal. The patient's body temperature was 37.3°C, and their general physical condition was normal. Normal chemistries were detected in the lab tests, including renal and hepatic function. Hemoglobin was 12.1 gm/L (reference value 12gm/L), platelets were 247,000/mm3 (reference value >150,000/mm3), white blood cells were 7350/mm3 (reference value >4500/mm3), and C-reactive protein (CRP) was 56 mg/L according to blood counts (reference values <8mg/L). The erythrocyte sedimentation rate (ESR), which ranges from 0 to 15 mm/h, was 52 mm/h, exceeding the average. Human immunodeficiency virus (HIV) and viral hepatitis serology were negative. The blood glucose was normal. Diabetes, renal failure, or long-term corticosteroid or immunosuppressant use were unreported.
The chest X-Ray showed an enlargement of the middle mediastinum associated to pleural effusion opacity, but any active pulmonary lesions (Figure 1). A computed chest tomography revealed the presence of a parietal mass centered on the sternum, with extension in the soft parts, bone lies of the sternal manubrium, lies of the vertebral hemi-bodies of T10 and T11, cervical lymph nodes, phrenic mediastinal and sub-pectoral nodes with peritoneal and mesenteric involvement (Figure 2). Magnetic resonance imaging of the spine showed tiered thoracic lumbar and sacral spondylitis with paravertebral and anterior epidural collections responsible for spinal cord compression next D10 without signs of spinal cord pain (Figure 3).
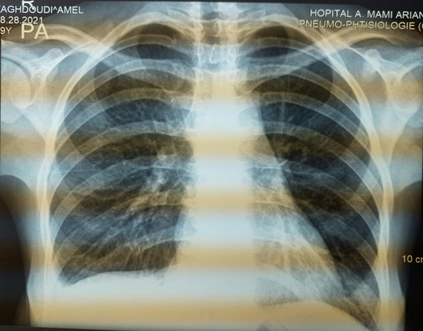
Figure 1 Chest X-ray showing an enlargement of the middle mediastinum associated to a pleural effusion opacity.
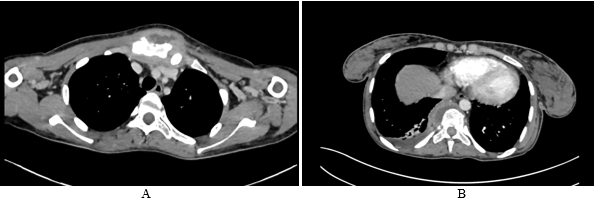
Figure 2 A-Chest computed tomography scan revealed a parietal mass centered on the sternum, with extension in the soft parts, bone lies of the sternal manubrium B- Mass centered on the right costovertebral gutters of the 10th and 11th ribs, lies of the vertebral homebodies of T10 and T11, right pleural effusion.
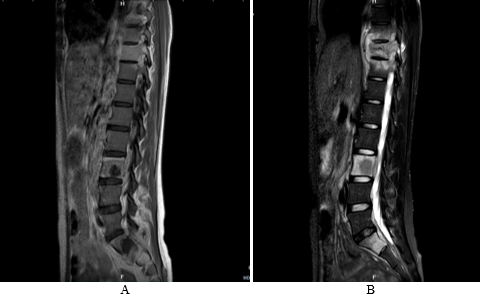
Figure 3 Magnetic resonance imaging scans in sagittal section showing multiple round ring signal shadows A- Vertebral body signal abnormalities extending to the posterior arches in hyposignal hypersignal T2 and FATSAT, enhancing after injection of Gadolinium B- tiered thoracic lumbar and sacral spondylitis with paravertebral and anterior epidural collections responsible for spinal cord compression next D10 without signs of spinal cord pain.
A diagnosis of tuberculosis spondylitis with osteitis was made and the differential diagnosis of metastatic malignancy, lymphoma, multiple myeloma, sarcoidosis, brucellosis, fungal disease and bacterial spondylitis were raised. Ultrasound guided draining of the sternal cold abscess associated to a CT-guided biopsy of paravertebral collections, revealed some whitish pus, in which acid-alcohol resistant bacilli were identified. Histopathological examination of the clod abscess revealed gaseous and granulomatous infection compatible with tuberculosis. The diagnosis of tuberculosis was confirmed. The seeding of the material on Lowenstein–Jensen medium identified Mycobacterium Tuberculosis. Accurate drug susceptibility testing was performed.
The patient was treated with anti-tuberculosis regimen based on Ethambutol (20mg/Kg/24h), Rifampicin (10mg/kg/24h), Isoniazid (5mg/Kg/24h), and Pyrazinamide (25mg/Kg/24h) for two months, and then rifampicin (10 mg/Kg/24h) and isoniazid (5mg/kg/24h) for seven months. After receiving anti-TB medication for a month, the patient's symptoms significantly improved.
TB is a major cause of mortality and morbidity worldwide and is responsible for 1.6 million deaths per year.6 According to the World Health Organization, 8.8 million new cases of TB occur every year world- wide.7,8 TB infection involves the lungs in about 90% of cases and can have many presentations.1,9 Clinical patterns of skeletal TB include spondylitis, osteomyelitis, peripheral joint infection, and soft tissue abscess.10 When there are two or more extra pulmonary locations, either with or without pulmonary involvement, the TB is considered multifocal.11 Our patient had osteoarticular and paravertebral tuberculosis involving skin, soft parts, cervical lymph nodes, mediastinal nodes and peritoneal tuberculosis. Our case had three particularities: first, the patient was immunocompetent. It is known that multifocal tuberculosis is extremely rare in immunocompetent patients. Second is the disseminated character of osteoarticular tuberculosis. Third, our patient presented with involvement of the sternal bone which is also very rare.12 Skeletal TB represents 10% of extra pulmonary tuberculosis.1 Among patients with skeletal TB, spinal and rib involvement accounts for approximately 50% and 5% of the cases, respectively.13,14 Typical chest X-ray in thoracic spinal tuberculosis shows a posterior mediastinal mass.15 Rib TB can mimic a metastatic tumor with bone destruction. In such cases, lung nodules can provide an indication for the diagnosis of TB. Computed tomography reveal the disco vertebral lesions and paravertebral abscesses. Magnetic resonance imaging is the appropriate imaging examination in TB spondylitis due to its superior soft tissue resolution and multiplanar capability.
In immunocompetent patients, multifocal TB is uncommon. Atypical sites and ability to mimic other diseases leads to diagnostic and therapeutic delays. Early diagnosis and well conducted treatment improves the prognosis.
None.
There is no conflicts of interest.
None.

©2023 Mansour, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.