Journal of
eISSN: 2376-0060


Case Report Volume 4 Issue 3
1Department of Surgery & Division of Thoracic Surgery, University Hospital of Ampefiloha, Madagascar
2Department of Surgery & Division of Urology, University Hospital of Ampefiloha, Madagascar
Correspondence: Razafimanjato Narindra Njarasoa Mihaja, Department of Surgery & Division of Thoracic Surgery, University Hospital of Ampefiloha, Madagascar
Received: February 09, 2017 | Published: June 21, 2017
Citation: Razafimanjato NNM, Ravoatrarilandy M, Ralijaona HS, Rakototiana AF, Rakotovao HJL (2017) A Pseudo-Mesothelioma Pleural Revelant an Carcinoma Urothelial Metastatic: About a Case and Review of the Literature. J Lung Pulm Respir Res 4(3): 00125. DOI: 10.15406/jlprr.2017.04.00125
The authors illustrate through an observation of an aggressive and exceptional pleural evolution metastatic of a carcinoma urothelial of the upper urinary tract at the origin of an atypical radiological aspect and rarely described of pseudo-mesothelioma. In our case, the instillation with the BCG Pasteur by the percutaneous nephrostomy and the pleur X with the profit of a heavy chemotherapy enabled us to in fact circumvent the evolution towards the acute complications related to this pathology, the malignant pleuresis.
Keywords: BCG, chemotherapy, differential diagnosis, mesothelioma, radiotherapy, surgery, urothelial carcinoma
Urothelial carcinomas occur in over 90% in the bladder, but can also affect the pan (about 5% of all kidney tumors), ureter and urethra.1 They give exceptionally pleural metastasis since in more than 75%, it is secondary to primary malignancies of pulmonary origin, gynecological diseases and lymphoma.2 The authors describe here the first Malagasy case of urothelial carcinoma of the upper urinary tract radiological discovery late in pleural metastatic and discuss differential diagnoses of the image and the evolution of this tumor treated with topical agent adjuvant through review of recent literature.
Mr RAV. 53 years old, no smoking was hospitalized for progressive worsening of dyspnea lasting for 6 months, accompanied by chest pain basi-left. In the interview we noted a notion regularly taking a decoction of clinical médicinales. L'examen virtues plants entering found an alteration of the general status (PS=3 according to WHO), a left pulmonary syndrome without condensation fever. Radiography of thorax face showed pleural thickening picture left scalloped. Chest CT (Figure 1) confirmed the pleural lesions secondary look and abdominopelvic CT scan for staging (Figure 2) found a retroperitoneal mass compatible of renal tumor primitive right. Biologically, there was a LDH assay was raised to 1423 IU/ml (5 times normal). Histological examination of a biopsy transthoracic puncture confirmed the location of a secondary urothelial carcinoma at the pleura (pT4N2M1) (Figure 3). Our patient had received a course of BCG instillation Pasteur by percutaneous nephrostomy and the tear-X (thoracic drainage system) and died after three months of decline following the natural evolution of the tumor.
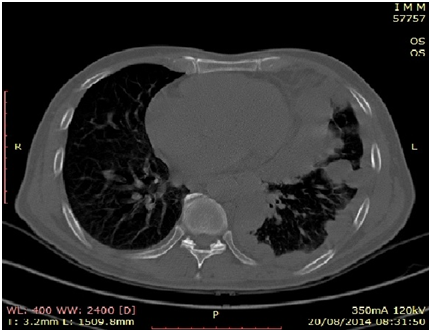
Figure 1 Chest CT scan showing regular pleural thickening withscalloped aspect of pleura revealing pleural malignant mesothelioma.
Tumors of upper tract (TVES)
The TVES entities are rare and account for about 5% of urothelial carcinomas all reported worldwide.3 The incidence of TVES peak between 70 and 80 years with an average age of diagnosis is between 65-70 years.3 The young age of discovery in our case is explained by the youth of our population. They most commonly affect men with a sex ratio of 1.5 to 2, 8en Europe and the United State between the period of 1997 to 2010.3,4 Our observation is the first case reported in Madagascar and no similar study is found in the Malagasy literature where the incidence of TVES unknown in our country.
TVES of risk factors are common to those of bladder tumors or smoking is widely incriminated with RR 2 or 3 compared to non-smokers.4 The decoction of plants is the etiologic agent found in our observation and could be the source of our sporadic cases. A risk factor similar to those found in the Balkan nephropathy and Chinese herbs recognized and reported in the literature since 1950.3 The discovery of TVES is happy chance in 10 to 16% of cases depending on the series with the waning of abdominal imaging performed for another reason.5 A pleurisy operating in a context of an impaired general condition us discover renal tumor after scannographic etiologic. Our case is a circumstance of discovery rarely reported in the literature and demonstrates advanced or metastatic TVES.6 Other more specific functional signs are indicative of these tumors such as hematuria (68-82%), pain (20-30%) or lumbar mass (10%).3 According to the recommendation of the AFU and the UAE (grade C), the USSR (flexible ureterorenoscopy) allows both to make the diagnosis (biopsy, cytology in situ) and conservative treatment of TVES in a time.7 Morphologically, the uro-scanner potentiated by furosemide injection is the reference imaging modality with a sensitivity and specificity of around 96% and 99% as against 50 to 60.5% for IVU.8 MRI can replace the uro-scanner but is not realized as first-line diagnosis or staging as if our observation.8
Pleural metastasis of urothelial carcinoma
If the bladder carcinomas are known to provide multiple forms of thoracic metastatic disease: solitary or multiple nodules, infiltrates segmental, or more rarely, Pancoast syndrome, acute respiratory distress syndrome, sarcoidosis pseudo-appearance, or excavations lung.9 Pleural metastatic location is very unusual and rarely indicative of the disease. Rare clinical cases are reported in the literature.10 Odier et al.,9 reported a similar observation with unilateral pleural involvement, of pseudomésothéliomateux appearance.9 Post mortem studies suggest that pleural carcinomatosis lesions are secondary to lymphatic or blood-borne spread or mixed tumor emboli. These attacks carry an aspect of pleural thickening ensheathing scalloped tumor or associated with pleurisy.4,9 These radiological lesions pose a differential diagnosis problem with mesothelioma and other pleural metastatic affected (adenocarcinoma, squamous cell carcinoma, sarcoma, melanoma, lymphoma).2 The diagnosis of these disorders is based on immunohistochemical examination of a pleural biopsy and has a prognostic value, therapeutic and forensic importance for patients exposed to asbestos.
Management of metastatic urothelial carcinoma
The treatment of metastatic urothelial carcinoma is based on the instillation of topical agents adjuvants (BCG or mitomycin C), chemotherapy (MVAC: Methotrexate, Vinblastine, Cisplatin Adriamycinand) and/or external beam radiation therapy.10 These treatments are mainly based on the transposition of the management principles of bladder tumors. We decided, in our case, the BCG instillation Pastor by percutaneous nephrostomy and the tear-X in favor of heavy chemotherapy before the alteration of the general state of our patient and the absence of technical platform radiotherapy in our center.
This case illustrates a rare and fatal pleural metastasis of urothelial carcinoma of the upper tract manifested by atypical radiological appearance of pseudomésothéliome. Nevertheless, we consider that our choice of therapy is judiciable in a developing country with a fragile health system given the prognosis of metastatic urothelial carcinoma according to the EBA report 2014.11
None.
None.
Authors declare that there is no conflict of interest.

©2017 Razafimanjato, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.