Journal of
eISSN: 2376-0060


Case Report Volume 10 Issue 3
1Department of Pulmonary Medicine, Government Medical College, India
2Department of Radiodiagnosis, Adesh Medical College, India
Correspondence: Harveen Kaur, Senior resident, Department of Pulmonary Medicine, Government Medical College Amritsar, Punjab, India
Received: December 10, 2023 | Published: December 20, 2023
Citation: Harveen K, Arora J, Naveen P, et al. A case of tuberculous meningitis complicated by large cerebral infarcts. J Lung Pulm Respir Res. 2023;10(3):79-80. DOI: 10.15406/jlprr.2023.10.00307
There is a substantial morbidity and fatality rate associated with tuberculosis meningitis (TBM). A severe consequence of tuberculosis meningitis is cerebral infarction (CI). It can be asymptomatic or symptomatic, causing stroke. In this case, large cerebral infarcts, an uncommon complication of TBM, is presented.
Keywords: MRI brain, CECT chest, tuberculosis
TBM, tuberculosis meningitis; CI, cerebral infarction; CVCs, cerebrovascular complications
Among chronic CNS infections, TBM is the most prevalent in underdeveloped nations.1 cerebrovascular complications of tuberculosis meningitis (TBM) are associated with increased morbidity and mortality.
One of the most severe forms of extra pulmonary tuberculosis is TBM. The real burden of TBM is unknown due to underreporting and diagnostic challenges, although it is assumed to be correlated with the general prevalence of tuberculosis.2
Owing to the involvement of major arterial branches, the majority of cerebral infarcts seen in TBM are small and asymptomatic. Diffusion-weighted imaging is the preferred investigation for large infarcts caused by posterior, middle, and anterior cerebral artery blockage, which are uncommon. They frequently happen in the region known as the "tuberculosis zone," which is the region supplied by the medial striate and thalamo-perforating arteries.3,4
Cerebrovascular complications (CVCs) of TBM have been reported as a predictor of poor prognosis with adverse outcomes.
A 32-year-old male presented with high-grade fever and headache for the last 4 months; followed by left-sided bodily weakness and difficulty in speaking, for a week. On examination, he was conscious with findings of neck rigidity, and positive Kernig's sign.
Chest X ray PA view showed micro nodular shadows scattered throughout the lung fields bilaterally (Figure 1). CECT Chest revealed multiple small nodules randomly scattered in bilateral lung parenchyma with associated interlobular and interlobular septal thickening, along with few subcentimetric lymph nodes in bilateral paratracheal regions, with one of them measuring 18 x 8 mm in size in right paratracheal region, (Figure 2) suggesting the diagnosis of Miliary tuberculosis.
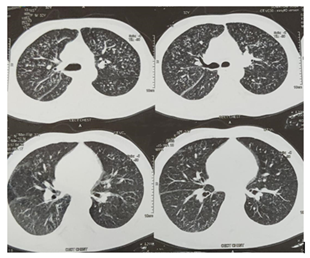
Figure 2 CT chest with contrast revealed multiple small nodules of average size 4mm, randomly scattered throughout bilateral lung parenchyma with associated interlobular and intralobular septal thickening.
Brain MRI showed multifocal areas of diffusion restriction T2, FLAIR hyperintense signal and few hyperintense areas involving bilateral frontal, capsulo-ganglionic regions, right parietal region and thalamus, alongwith incomplete suppression of CSF signal on FLAIR images in basal cisterns, s/o Subacute infarcts (Figure 3). CSF analysis revealed protein 3.8 g/L, glucose 1.7 mmol/L (blood glucose 7.6 mmol/L), leukocyte count of 267 with lymphocytosis, and positive Gene Xpert MTB/RIF assay.
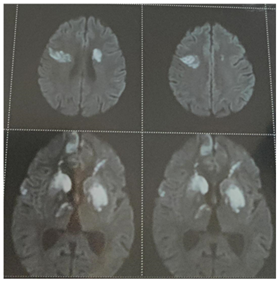
Figure 3 MRI brain revealed multifocal subacute infarcts involving bilateral frontal, capsule-ganglionic regions, right parietal region and thalamus.
He was started on first-line anti-tuberculosis therapy (ATT), comprising of isoniazid, rifampicin, pyrazinamide, ethambutol, along with steroids, and aspirin. After 3 months, his fever and headache improved significantly but left sided body weakness and difficulty in speaking persisted, confirming the diagnosis of TBM. After 12 months of ATT completion and follow-up, his motor functions improved with only some residual deficits.
TBM is the most severe form of extra pulmonary tuberculosis, with mortality of 25% and long-term neurological disability of 50%.5 TBM kills or seriously disables over half of those affected, although only accounting for 1% of the 9 million tuberculosis cases that occur each year worldwide.1 The main complications of TBM include cerebral stroke, hydrocephalus and tuberculoma formation. Between 15–57% of TBM cases have infarcts, which are typically related to advanced illness.3
The mortality is about 3 times higher in TBM patients with stroke compared to those without. However, the infarction mechanisms in TBM patients are poorly understood. They have been linked to a variety of pathogeneses, such as vasculitis, arterial thrombosis, and vascular proliferation.3
Additionally, some regions of the brain are more prone to develop infarctions than others. These regions are known as TB zones, and they include the thalamus, internal capsule, and basal ganglia. This region of the circle of Willis typically has the most severe TBM exudates, which is responsible for this pattern of involvement.6
In the study by Hsieh et al, only 11% of infarcts occurred in the "ischaemic zone" supplied by the lateral lenticulostriate, anterior choroidal, and thalamogeniculate arteries, while 75% of infarcts occurred in the "TB zone" supplied by the medial lenticulostriate and thalamoperforating arteries.6
The common clinical presentations of patients of TBM with stroke include fever, neck stiffness, headache, altered sensorium, focal weakness or hemiplegia, cranial nerve palsy, and seizures. Despite numerous previous attempts to develop established clinical diagnostic criteria, it is still difficult, particularly in regions with low prevalence, to conclusively determine or rule out the diagnosis of TBM using signs, symptoms, and routine examinations.1 thus, lumbar puncture is typically done despite the possibility of herniation. Currently, the WHO recommends using the GeneXpert MTB/RIF assay for confirmation in such cases. It is crucial that this quick diagnosis technique spreads throughout underdeveloped nations because failure to start treatment right away is the biggest predictor of death.1
Isoniazid, rifampicin, pyrazinamide, and ethambutol are the first-line ATT medications that should be administered for 9–12 months. Given that multidrug-resistant tuberculosis is prevalent in many places, regional treatment standards must be followed; which makes the GeneXpert very useful.
A variable proportion of TBM cases are complicated by cerebral infarctions, which can additionally have a negative impact on the prognosis. MR is the imaging modality of choice for early diagnosis and timely management. The correct and prompt identification of cerebral infarcts in TBM is important so that appropriate treatment can be started early.
None.
There are no conflicting interests declared by the authors.
None.

©2023 Harveen, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.