Journal of
eISSN: 2373-6453


Case Report Volume 10 Issue 3
1DM Infectious Disease Resident, Department of Infectious Diseases, Christian Medical College, India
2Infectious Disease Faculty, Department of Infectious Diseases, Christian Medical College, India
Correspondence: Dipankar Pal, MD (DM Infectious Disease Resident), Infectious Disease Resident, Department of Infectious Diseases, Christian Medical College, Vellore, Tamil Nadu, India, Tel 9432113713
Received: August 22, 2023 | Published: September 6, 2023
Citation: Dipankar P, Kundakarla BP, Prasannakumar P, et al. Primary mandibular mucormycosis without para nasal sinus involvement following SARS CoV-2 infection – a series of four cases and review of literature. J Hum Virol Retrovirol. 2023;10(3):59-63. DOI: 10.15406/jhvrv.2023.10.00268
The increased incidence of mucormycosis in post covid-19 is due to steroid induced diabetes mellitus. The commonest presentation is acute invasive fungal sinusitis involving maxillary sinus most commonly followed by invasion to local soft tissues and bone structures. It also involves orbit and brain extending from sinuses. Mandible has no direct communication with any of the para nasal sinuses and involvement is extremely rare and seldom reported. We came across four such cases during post covid-19 mucormycosis epidemic. Poor dentitions, ulcerated mucosa, inoculation during dental procedures are the proposed mode of entry of the fungi into the mandible.
Keywords: Covid 19, steroids, diabetes, mandibular mucormycosis
Mucorales are a group of filamentous fungi classified under zygomycetes with worldwide distribution. It commonly presents as rhino-orbito-cerebral disease in diabetic patients.1 In other types of immunosuppression e.g solid organ transplant, hematopoietic stem cell transplant it presents as predominant pulmonary and disseminated disease.2,3 In post Covid-19 era many patients developed diabetes mellitus due to steroid overuse or abuse. Covid-19 associated mucormycosis (CAM) predominantly involves paranasal sinuses with extensive soft tissue disease and subsequent bony and angioinvasion.4,5 Maxillary sinus is the most commonly affected as the spores are directly inhaled into it and start disease.
Mandible is non-contiguous bony structure to para nasal sinuses and its involvement by mucorales is extremely rare. Dental procedures and extraction along with poor oral hygiene initiate inoculation of mucor sp. spores and subsequent mandibular osteomyelitis. Isolated mandibular mucormycosis without sinus involvement following Covid-19 disease is extremely rare and seldom reported.
In this series, we present four post Covid-19 patients with isolated mandibular mucormycosis without any sinus, orbit or brain involvement.
Case 1: He was a 39 year old male presented with left jaw pain for two months. He was diagnosed with Covid-19 pneumonia and required oxygen with dexamethasone at a dose of 6mg twice a day followed by once a day for total 14 days eight months ago. Due to his jaw pain he consulted dentist before coming to our instituition and underwent left 3rd molar extraction. Following the procedure his symptoms did not improve rather worsened. Pain and swelling increased gradually and there was oozing from the tooth extraction site. He did not have any sinus symptoms and underwent CT scan which revealed left mandibular osteomyelitis (Figure 1). No sinus tenderness was present and sinus endoscopy showed normal mucosa. HbA1C was 9.2%. Debridement of left mandible with extraction of corresponding molars was done. Histopathology from the debrided tissue showed aseptate, broad fungal hyphae with obtuse angle branching with bony and angioinvasion characteristic of mucorales (Figure 2). However fungal culture was negative. He was treated with 2 weeks injection amphotericin - b lipid emulsion which he tolerated well without any toxicity.
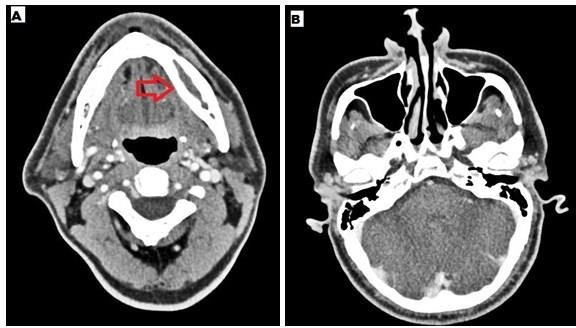
Figure 1 A- CT mandible - left mandibular osteomyelitis with expansion of the cortex, B- CT paranasal sinuses – normal.
Symptoms resolved and wound became healthy. He was started on tablet posaconazole. Trough level was done after 7 days and it was 1606 ng/ml. Total 3 months of oral therapy was completed and he did well on follow up.
Case 2: He is a 46 years old male presented with pain and swelling of bilateral jaw. He was diagnosed with mild Covid-19 five months ago and received dexamethasone 6mg twice a day followed by once a day for 10 days. There was no history of prior dental procedures. No sinus pain or discharge was present. Sinus endoscopy was unremarkable. HbA1C was 11.2%. Imaging showed bilateral mandibular osteomyelitis (Figure 3) and underwent debridement. Histopathology from the debrided tissue showed broad aseptate fungal hyphae with obtuse angle branching associated with bony and angioinvasion suggestive of mucorales. Few actinomycotic colonies are also found interspersed in the tissue biopsied. Culture was negative for fungal organisms. He was started on injection amphotericin b deoxycholate due to cost constraints and developed acute kidney injury after 5 days. As the disease was limited to bone and he could not tolerate injection amphotericin b for more than 5 days we switched him to tablet posaconazole. Trough concentration was measured after 7 days and found to be 1308 ng/ml. He did well with oral therapy and completed 3 months of posaconazole.
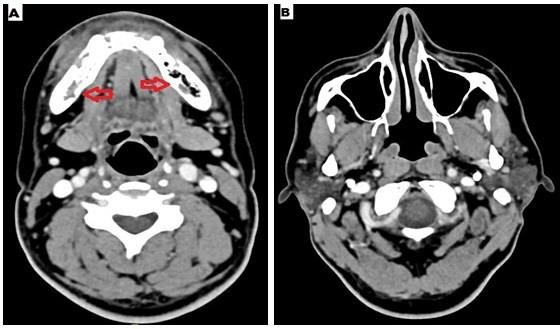
Figure 3 A - CT mandible- bilateral mandibular osteomyelitis with erosion of the cortex, B - CT paranasal sinuses- normal.
Case 3: A 51 year old lady presented with left sided jaw pain for 1 month. She is a known patient of hypertension and diabetic nephropathy. She was admitted with moderate Covid- 19 pneumonia and received dexamethasone 6mg twice a day followed by 6mg once a day for total 21 days, remdesivir and supplemental oxygen 6 months before presentation. There was no prior dental procedure or tooth extraction before her symptoms started. All para nasal sinuses were normal clinically. Sinus endoscopy was normal. HbA1C was 10.3%.
Z-orthopantomogram showed left mandibular erosions with affected tooth had spontaneously fallen off (Figure 4). She underwent complete debridement and histopathology from the intra operative specimen showed broad aseptate fungal hyphae with obtuse angle branching alongwith bony and angioinvasion. Fungal culture was not sent from dental surgery where she was initially admitted. Due to multiple comorbidities she was not offered injection amphotericin b due to its known toxicities and treated with tablet posaconazole for 3 months. Her trough posaconazole concentration was found to be 1570 ng/ml and she did well with this therapy.
Case 4: A 49 year old lady with no prior co morbidity developed mild Covid-19 pneumonia 3 months ago and was treated with supplemental oxygen and steroids in the form of dexamethasone 6mg once a day for total 12 days. She did not require antivirals. She presented with bilateral jaw pain and numbness over the overlying skin for 3 weeks. She had no prior dental manipulation. There was no sinus symptom associated with jaw pain.
Sinus endoscopy did not reveal any mucosal disease, CT image of the sinus was also normal. HbA1C was 9.7%. Z-orthopantomogram showed bilateral mandibular erosions (Figure 5). CT showed bilateral mandibular osteomyelitis (Figure 6). Debridement was performed and histopathology revealed broad aseptate and pauciseptate fungal hyphae with obtuse angle branching. There was significant bony and angioinvasion; a characteristic feature of invasive mucormycosis. Fungal culture was negative. She was started on injection lipid emulsion amphotericin b and was continued for 2 weeks. She responded well and was switched to tablet posaconazole after 2 weeks. Serum trough level was performed after 7 days and was found to be 1483 ng/ml.
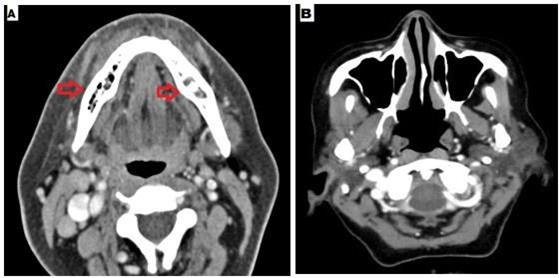
Figure 6 A- CT mandible revealed bilateral mandibular osteomyelitis with cortical expansion, B- CT paranasal sinuses – normal.
We have performed extensive literature search and there are heterogenous reports of mandibular mucormycosis in different patient population. Our cases are more homogenous and all had previous Covid-19 with steroid use followed by diabetes (Table 1).6–23
|
Case no. |
Authors |
Year of publication |
Type of Study |
Age |
Gender |
Underlying condition |
Outcome |
|
1 |
Brown OE et al. |
1986 |
Case report |
57 |
M |
DM, Chronic renal failure |
Death (due to cardiac arrest) |
|
2 |
Jones AC et al. |
1993 |
Case series |
43 |
M |
AML, Acute renal failure, Pancytopenia |
Clinically improved |
|
3 |
Salisbury et al. |
1997 |
Case report |
60 |
M |
AML, Prostate cancer, Heavy alcoholism, Hypertension |
Recovery satisfactory |
|
4 |
Lador et al. |
2006 |
Case report |
42 |
F |
Acute lymphoblastic leukemia |
Death (due to Leukemia) |
|
5 |
Bakathir AA et al. |
2006 |
Case series |
49 |
M |
DM with ketoacidosis, ALL, dental extraction |
Recovery satisfactory |
|
6 |
Dogan MC et al. |
2007 |
Case report |
7 |
M |
AML |
Incomplete healing (after 4 weeks of debridement and antifungal) |
|
7 |
Antonetti J et al. |
2009 |
Case report |
10 |
M |
Severe burns |
Recovery satisfactory |
|
8 |
Ojeda-Uribe M et al. |
2010 |
Case report |
55 |
F |
AML Decompensated DM |
Clinically improved |
|
9 |
Oswal NP et al. |
2012 |
Case series |
68 |
F |
DM, diabetic nephropathy, hypertension, sleep apnea,dental extraction |
Death (due to septicaemia with multiorgan failure) |
|
10 |
Aras MH et al. |
2012 |
Case series |
6 |
M |
Neuroblastoma AML |
Death (due to maligancy) |
|
15 |
M |
||||||
|
11 |
Mc Spadden RP et al. |
2016 |
Case report |
63 |
M |
CML, steroid and immunosupresive therapy |
Death (due to infection) |
|
12 |
Urs et al. |
2016 |
Case series |
26 |
M |
Dengue fever, dental extraction |
Clinically improved |
|
13 |
Cheong et al. |
2017 |
Case series |
38 |
F |
Chronic lymphocytic leukemia |
Death (due to pneumonia) |
|
14 |
Cohen et al. |
2019 |
Case series |
21 |
F |
ALL |
Clinically improved |
|
14 |
M |
ALL |
|||||
|
41 |
M |
AML |
|||||
|
15 |
Elitzur et al. |
2019 |
Multicentre study (4 cases of mandibular mucor) |
Not specified |
Not specified |
Acute Leukemias |
Death due to mucormycosis in 2 out of 4 cases |
|
16 |
Agarwal et al. |
2020 |
Case report |
37 |
M |
Chronic granulomatous disease, tooth extraction, kidney disease |
Recovery satisfactory |
|
17 |
Kwak et al. |
2020 |
Case report |
61 |
M |
AML, DM, hypertension, dental extraction |
Clinically improved |
|
18 |
Ambereen A et al. |
2021 |
Case report |
39 |
M |
SARS-CoV-2 infection |
Recovery satisfactory |
|
19 |
Bhanumurthy L et al. |
2022 |
Case report |
45 |
F |
DM, SARS-CoV-2 infection |
Clinically improved |
Table 1 Mandibular mucormycosis: reports in literature6–23
Isolated mandibular mucormycosis without sinus involvement is a rare clinical presentation of this ubiquitous filamentous fungus. There are only a few isolated case reports of Covid-19 associated mandibular mucormycosis in the literature.23,24 How mucorales gain access to mandible is not clear as it is not contiguous with para nasal sinuses. The portal of entry is probably due to direct inoculation during dental procedures or minor dental trauma. The disease is not at all well characterised and rather an extremely uncommon entity. The exact pathogenesis is also not known properly. We report the largest case series of mandibular mucormycosis till date; diagnosed and treated successfully in our institute. All of them are post Covid-19 who received systemic steroids with or without antivirals in recent past alongwith supplemental oxygen. Three of them became diabetic following steroid use post Covid-19. Case 3 lady was known to have diabetic nephropathy and on top of that she received systemic steroid during Covid-19 illness. Case 1 had prior dental extraction and rest 3 patients did not have any prior dental procedure. Probably poor dental hygiene with uncontrolled diabetes had initiated the disease process in them. Numbness of local skin, pain in the affected area and pus discharge following dental procedures are the usual presentation in our cases. Neither of the cases found to have sinus symptoms or disease on imaging. It further confirms the fact that mandibular mucormycosis is unrelated to invasive sinusitis. The pathogenesis here is different from that of usual mode of presentation ranging from sinusitis to ocular and brain extension.
Case 1 and 4 received two weeks of amphotericin b lipid emulsion, case 2 received it for 5 days with early switch to oral therapy due to amphotericin b induced acute kidney injury. We decided to give only oral posaconazole in case-3 as the disease was localised and she had multiple comorbidities.
Management of isolated mandibular mucormycosis is not standardised due to rarity of the disease. This approach may be recommended in centres dealing with mandibular mucormycosis
Posaconazole pharmacokinetics is a controversial matter worldwide and often enough trough concentration cannot be achieved in vivo. Dose and formulations also vary in different countries and have impact on overall outcome. We used 300mg oral posaconazole in capsule form without antacids and proton pump inhibitors. We used to test posaconazole trough concentration after 5-7 days of initiation to look for the adequacy. Recommended target trough concentration is more than 1000 ng/ml. It is evident from our series that this approach is effective to achieve adequate trough concentration in vivo and able to have a favourable impact on outcome. Our series also demonstrate the efficacy of lipid emulsion amphotericin B in invasive mucormycosis.
Majority of the studies done previously in different countries are either on deoxycholate or liposomal preparation. Lipid emulsion amphotericin b is a cheaper alternative to liposomal and has similar low toxicity profile. It can be used in low income countries successfully to treat mucormycosis. It will cut down the cost of therapy without increasing nephrotoxicity.
Actinomycotic colonies were found in case 2 in biopsy specimens. It is a coloniser of necrotic tissues of mandible. Actinomycetes are a common commensal of oral cavity. Any biopsy from the dental procedures or mandibular bone when diseased may show these colonies in the histopathology. As the culture was negative it should not be taken as pathogenic and does not warrant any therapy. It should be interpreted with caution just like other commensals. For a commensal to become a pathogenic organism it must show tissue invasion. In our case it was separately lying colonies resembling fungal ball like structures for which debridement was the management of choice which we performed during the initial surgery.
The present study showed the pharmacological potential of the ethanolic extract of Neem bark. Our findings demonstrated that the F-EtOAc, obtained after saponification of EtCNeem, showed to be rich in phenolic and flavonoid compounds with antioxidant potential, as well as a nontoxic.
None.
No funding was received from any organisation or individual for this case.
The author has no conflict of interest to declare.

©2023 Dipankar, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.