Journal of
eISSN: 2377-4312


Case Report Volume 9 Issue 1
1College of Veterinary Medicine, Iowa State University, USA
2Veterinary Diagnostic and Production Animal Medicine, Iowa State University, USA
3Lloyd Veterinary Medical Center, Iowa State University, USA
4Veterinary Clinical Sciences, Iowa State University, USA
5Systems Modelling and Reverse Translational Pharmacology, Iowa State University, USA
Correspondence: Joe Smith, Iowa State University, 1809 S. Riverside Dr, Ames, Iowa, USA
Received: December 08, 2019 | Published: January 15, 2020
Citation: Cain A, Kirkpatrick J, Breuer R, et al. A case of a linear foreign body removal in a miniature companion pig. J Dairy Vet Anim Res. 2020;9(1):6?9. DOI: 10.15406/jdvar.2020.09.00271
Despite the recent rise in popularity of miniature pigs as companion animals, there are few published reports available regarding gastrointestinal surgery in these animals. This case report describes a 4-year-old castrated male companion potbellied pig who was diagnosed with a small bowel linear foreign body and associated pyloric outflow obstruction. A gastrotomy and three enterotomies involving the proximal and mid-jejunum and proximal centripetal loop of the spiral colon were performed to remove the linear foreign body. The surgical techniques and post-operative care described in this case report provided effective treatment of the linear foreign body and adequately prevented clinical evidence of post-operative complications in the companion potbellied pig. Follow-up information was obtained via telephone interviews and a recheck appointment one year later revealed a healthy animal with no abdominal radiographic or ultrasonographic abnormalities.
Keywords: Potbelly pig, pig, foreign body, surgery
A 4-year-old, 27 kg, castrated male potbelly pig with a 24 hour history of anorexia, decreased water intake, vomiting, decreased fecal production, and shivering was presented to the Food Animal and Camelid Hospital, Iowa State College of Veterinary Medicine for evaluation. These clinical signs were noticed shortly after the pig was found to have consumed a portion of a blanket used as bedding. Upon presentation, the patient was bright, alert, responsive, and inquisitive of the environment, although demonstrated several indicators of pain including postural changes.1 The pig had an ideal (2.5/5) body condition score based on a scoring system for commercial pigs.2 The patient was sedated with intramuscular midazolam (0.5mg/kg) and ketamine (1mg/kg), and maintained under general anesthesia with 2% isoflurane inhalant and oxygen (2L/min) via mask to facilitate physical examination. Incidental physical examination findings included oral malocclusion due to an elongated permanent lower right canine tooth as well as moderate alopecia over the dorsum and bilateral dark brown ocular discharge with mild conjunctivitis. The remainder of the physical examination was unremarkable. Whole blood was collected from an auricular vein for a complete blood count (CBC) and serum chemistry. The pig’s CBC revealed hemoconcentration with a hematocrit of 56% (normal 28.2-42.6%) and remaining CBC parameters were otherwise unremarkable. The pig’s serum chemistry revealed hypokalemia (2.8mEq/L, normal 4.0-7.0) and azotemia (creatinine 3.0mg/dl, normal 0.5-2.7mg/dL) but was otherwise unremarkable. Reference ranges from the Iowa State University Clinical Pathology laboratory were utilized. While under general anesthesia, three-view abdominal radiographs were obtained and revealed linear soft tissue opaque material in the proximal duodenum as well as a severely gas distended stomach (Figure 1). The remainder of the gastrointestinal tract was moderately diffusely dilated with gas and regions of heterogeneous soft tissue material. Differentials for this moderate diffuse dilation included severe enteritis or secondary to additional site(s) of small intestinal mechanical obstruction. Isoflurane was discontinued and the patient was allowed to recover from general anesthesia.
Anesthesia
Exploratory celiotomy was elected to relieve the obstruction. Vascular access was secured in the left auricular vein. The patient was pre-medicated with hydromorphone (0.05mg/kg IV) and induced with ketamine (1.5 mg/kg IV) and propofol (1.5 mg/kg IV). A total of 4 mg of 2% lidocaine solution was applied to the arytenoids and focal folds with an atomizer to prevent laryngospasm and an 8mm endotracheal tube was placed as previously described by Smith et al.3 Due do dehydration and hypokalemia, a 1L Lactated Ringers Solution bolus followed by 25mL LRS supplemented with KCl was initiated through the auricular IV catheter prior to anesthesia (at a rate not to exceed 0.5 mEq KCl/kg/hr). General anesthesia was maintained with 1.5-2.5% sevoflurane inhalant and oxygen (1L/min). Post-induction SpO2 ranged from 95-100%, and the patient was placed on intermittent positive pressure ventilation (IPPV) to maintain normocapnea. Intraoperatively, a ketamine (600mcg/kg/hr) and lidocaine (50mg/kg/min) IV CRI was provided. The right auricular artery was catheterized to monitor blood pressure. The patient was monitored using capnography, pulse oximetry, electrocardiography, temperature probe, Doppler blood pressure and invasive blood pressure. Warming therapy included a hot air warmer and circulating warm water mat to minimize intraoperative hypothermia. Intraoperative anesthetic complications included hypotension, and hypothermia. The patient received an additional dose of hydromorphone at 0.05 mg/kg IV prior to recovery for post-operative analgesia and recovered unremarkably from general anesthesia and surgery.
Surgery
An approximately 20cm ventral midline abdominal incision from the xyphoid to the pubis traversing to the left of the prepuce was performed. The fat and subcutaneous tissue were dissected down to the linea alba. A stab incision through the linea alba was made using an inverted #10 blade to enter the abdomen. A medium Balfour retractor was inserted to allow exploration of the abdomen. Foreign material was palpated within the stomach, duodenum, jejunum, spiral colon, and descending colon. There was a moderate degree of plication and gas distension in the proximal jejunum. No areas of serosal erosion or perforation were noted. Moistened laparotomy sponges were used to protect the abdominal cavity and isolate the stomach. Two stay sutures were placed in the body of the stomach towards the cardia and pylorus using 3-0 polydioxanone in a cruciate pattern. An approximately 5 cm incision was made in the body of the stomach between the stay sutures. Suction was used to remove liquid gastric contents. A small amount of fabric foreign material was exteriorized and cut at its attachment as it entered the pylorus using Mayo scissors. The gastrotomy site was closed in two layers using 3-0 polydioxanone in a simple continuous pattern and oversewn with a cushing pattern. The plicated and gas distended portion of the jejunum was exteriorized and measured approximately 20 cm. Moistened laparotomy sponges were placed around the exteriorized jejunum. A ¼ inch penrose drain was placed in the avascular portion of the jejunal mesentary orally and aborally to the palpable foreign material and loosely tied around the jejunum to prevent leakage of jejunal contents. The proximal aspect of the foreign body was isolated in the proximal jejunum. Fingers were used to manipulate and occlude the section of jejunum both oral and aboral to the planned enterotomy incision site. An approximately 2 cm enterotomy was made on the anti-mesenteric surface of the jejunum. A small amount of cloth fabric was removed from the jejunal lumen and cut at its attachment to adjacent bowel. The enterotomy incision was closed in one layer with 3-0 polydioxanone in a simple interrupted pattern centrally and simple continuous with full thickness bites on either side. The integrity of the incision closure was tested by injecting saline into the lumen of the jejunum, no areas of leaking were present. A second enterotomy measuring 1.5 cm was made 10 cm aboral and in a similar fashion to the first enterotomy site. A small amount of foreign cloth material was easily removed from the jejunal lumen; alleviating tension placed on remaining plicated jejunum. The enterotomy site was closed using 3-0 polydioxanone in a simple continuous pattern. The integrity of the incision closure was tested by injecting saline into the lumen of the jejunum, no areas of leaking were present. The ¼ inch penrose drains were removed and the hole left in the jejunal mesentery was closed using 3-0 polydioxanone in a cruciate pattern. Several large, firm regions of foreign material were noted within the proximal centripedal loop of the spiral colon. That section of spiral colon was isolated and the packed off using moistened laparotomy sponges. Fingers were used to manipulate and occlude the section of proximal spiral colon both oral and aboral to the planned enterotomy incision site. An approximately 2 cm enterotomy was made on the anti-mesenteric surface of the spiral colon. A moderate amount of cloth fabric was removed from the spiral colon lumen. The enterotomy incision was closed in one layer with 3-0 polydioxanone in a simple continuous pattern. Following foreign body removal, gloves were changed and a new instrument pack was used for closure of the abdomen. A rent measuring approximately 4cm was noted within the omentum adjacent to the pancreas and closed in a simple continuous pattern using 3-0 polydioxanone. A mild amount of bleeding in the craniodorsal abdomen, adjacent to the liver, was appreciated but could not be localized. The abdomen was copiously lavaged with 4 liters of warm saline. The linea alba was closed using a simple continuous suture pattern with 0 polydioxanone suture. The subcutaneous layer was closed with 2-0 polyglactin 910 using a simple continuous pattern. The dermal layer was closed in a simple continuous pattern using 2-0 poliglecaprone 25. The skin incision was covered with an aluminum-based aerosol bandage after closure.
Post-operative management
The pot bellied pig was hospitalized for a total of six days. Post-operatively, the patient was administered hydromorphone (0.5 mcg/kg IV every four hours for the first night), flunixin meglumine (1.1 mg/kg IV once), gentamicin (5 mg/kg IM every 24 hours for three doses), sucralfate (3.7 mg/kg PO every 6 hours for five days), and IV LRS supplemented with potassium chloride (50 ml/kg/day for two days). Due to the inflammation noted in the mucosal surface of the bowel the pig was administered ceftiofur (5 mg/kg, SQ, once) post operatively. The pot bellied pig was provided a soft diet of pelleted feed moistened with canned pumpkin, apple sauce, and fruit juice. The patient’s appetite was mildly decreased 48 hours after surgery, prompting provision of grass hay, cantaloupe, and a variety of nuts. 48 hours post-operatively, the patient was sedated with midazolam (1 mg/kg IM) to facilitate venipuncture for a complete serum chemistry and an abdominal focused assessment with sonography for trauma, triage, and tracking (AFAST). The pot bellied pig’s serum chemistry revealed static hypokalemia (3.5 mEq/L) and hypomagnesemia (1.70 mEq/L), prompting oral supplementation of an electrolyte solution in the patient’s water for the remainder of hospitalization. No overt evidence of abdominal effusion, fibrin, or adhesion formation was appreciated during the abdominal ultrasonographic examinations. Additionally, an absence of fecal production 48 hours following surgery, prompted performance of a fleet enema during the same sedation event. Oral administration of carprofen (2 mg/kg) was initiated two days post-operatively with improved appetite. On the sixth and final day of hospitalization, the patient was sedated with ketamine (1mg/kg IM) and midazolam (1mg/kg IM) to facilitate venipuncture for a complete blood count (CBC) and serum biochemistry panel. The patient’s CBC was unremarkable except for a mild eosinophilia (2.38 1x103/ul) while the serum chemistry was unremarkable. A modified McMaster’s fecal egg count was also performed which was negative for evidence of intestinal parasites. At discharge, the pot bellied pig was eating well with appropriate fecal production. The patient was discharged with carprofen (2 mg/kg PO every 12 hours for two days) and instructions for incision care, activity restriction, and monitoring for evidence of abdominal pain. Information regarding long-term (>6 months after hospital discharge) survival was obtained via phone and email. The owner reported no complications following hospital discharge and was satisfied with the surgical outcome.
Pot bellied pigs have become popular companion animals in recent years, with the total North American population thought to be close to one million animals,3 tasking a growing number of veterinarians with their medical care.4 Among the most frequently reported reasons for companion pot bellied pigs to present to a veterinarian are generalized gastrointestinal clinical signs including anorexia, vomiting, decreased fecal production, abdominal distension, and abdominal pain.5 Gastrointestinal diseases previously reported in companion pot bellied pigs include intestinal obstruction, gastric ulceration, intestinal torsion or volvulus, endoparasitosis, and neoplasia.5,6 Additionally, companion pot bellied pigs are liable to dietary indiscretion resulting in foreign body ingestion and subsequent intestinal obstruction.6 Despite the recent rise in popularity of potbellied pigs as pets and their propensity for gastrointestinal obstructions requiring surgical correction, little published information is available regarding gastrointestinal surgery in these animals.4 Among the companion pig literature, several cases of gastrointestinal surgeries are described. Spiral colon bypass has been utilized for stricture of the spiral colon in an 8 year old potbellied pig.7 For a 7 month old miniature pig with megacolon, subtotal colectomy and ileocolonic anastomosis was successful,8 suggesting that porcine megacolon may be managed in a comparative manner to that of the feline. In addition, the observed complications to gastrointestinal tract surgery in the pet pig have been described.6
A retrospective study of gastrointestinal tract surgery in pet pot bellied pigs described the most significant post-operative complication to be peritoneal adhesion formation and potential maturation into a restrictive adhesion formation resulting in intestinal narrowing and obstruction.6 However, in the absence of peritoneal adhesions, the prognosis for survival following surgical foreign body removal was excellent.6 Published recommendations to avoid such adhesion formation include atraumatic surgical technique, intra-abdominal lavage, omentectomy, use of protective tissue-coating solutions such as sodium carboxymethylcellulose, as well as antimicrobial and anti-inflammatory administration.6,9 Antimicrobial coverage for this case was achieved by gentamicin and ceftiofur. Anti-inflammatories administered included flunixin meglumine initially, as well as carprofen. When using multiple anti-inflammatories, clinicians should be aware of adverse effects such as gastric ulceration. However, the authors have found that administration of an initial dose of flunixin meglumine transitioned to carprofen afterwards to be a convenient way to administer a nonsteroidal prior to surgery and then continue coverage afterwards, as reflected in another miniature pig case report (Figure 1).3
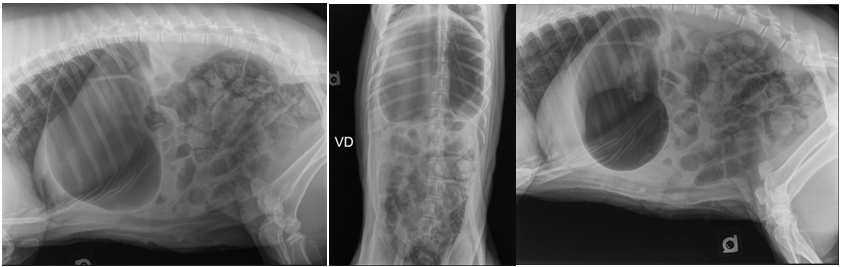
Figure 1 Right lateral (A), ventrodorsal (B), and left lateral (C) abdominal radiographs showing severe gas dilation of the stomach and moderately to severely diffusely dilated intestines with gas and soft tissue opaque material. In the left lateral projection (C), an amorphous and heterogenous soft tissue and gas opaque feature is noted in the proximal duodenum.
An additional consideration of this case is the unique position of the miniature pig as both a companion and food animal in the United States. As such, clinicians need to be aware of this when considering drug selection. While it is not a common occurrence, there have been reports of companion miniature pigs entering the food chain,10 and caution should be exercised with extra-label drug use in the species. For example, the use of gentamicin in this case would be extralabel use in a food animal, as the use of this drug in an adult pig could lead to extremely extended slaughter withdraw periods. Similarly, in the United States currently ceftiofur usage in major food animal species is limited, and in this case while it was used to treat an enteritis, which would be an off label indication, the appropriate label dose, route, and frequency was used for permissible extralabel use.11 While it was understood that the animal was a companion, and not a production pig, the owner was counseled as to what the drugs administered to their animals meant from a regulatory perspective. This was done by providing the following statement “While we understand that (name redacted) is a companion animal, we are legally obligated to inform you that the drugs administered to your animal carry a withdraw period. Please contact us if you need this information” in the discharge instructions, and then explaining to the client what the responsibilities for a veterinarian in the United States are with respect to extralabel drug use. The authors have found this strategy to be effective in communicating this responsibility, as it relays the message without implying the client will be using their pet for food. Currently, in the United States, there is no regulatory exception for drug use in companion pigs compared to commercial pigs, so clinicians should be aware of appropriate extra-label drug usage with this species.
This report describes a small bowel linear foreign body and associated pyloric outflow obstruction in a pet potbellied pig and the surgical technique with and post-operative care utilized to successfully relieve the obstruction while preventing clinical evidence of post-operative complications.
The authors wish to recognize Dr. Morgan Murphy for her anesthetic planning and care of this patient under anesthesia.
No conflicts of interest exist.

©2020 Cain, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.