Journal of
eISSN: 2374-6947


Research Article Volume 9 Issue 2
1University Hospital of Libreville, Gabon
2University Hospital of Owendo, Gabon
Correspondence: Annick Flore Mfoumou Essono, University Hospital of Libreville, Gabon
Received: September 30, 2022 | Published: October 31, 2022
Citation: Essono AFM, Essone JFN, Mbina E, et al. Anemia in hospitalized diabetics: experience of the Libreville Chu. J Diabetes Metab Disord Control. 2022;9(2):77-80. DOI: 10.15406/jdmdc.2022.09.00241
Background: Anemia is the most common hematological abnormality in diabetes. Understanding the pathogenesis of anemia associated with diabetes may help optimize its management. We conducted a study to determine the biological and etiopathogenic features that may be associated with anemia in Gabonese diabetic patients.
Patients and method: Retrospective descriptive study of diabetic patients hospitalized in the endocrinology department of the University Hospital of Libreville during the year 2017 was included: any hospitalized patient with a hemoglobin (Hb) level less than: 13g/dl (men), 12g/dl (women). Anemia was mild if Hb in women between10.9 and11.9g/dl and in men between 10.9 and 12.9 g/dl Hb, moderate if Hb between 8 and 10.9 g/dl and severe if Hb< 8g/dl. Data analysis: EPI-INFO version 3.5.
Results: 153 cases included/782 hospitalizations: prevalence 19.56%.mean age 54.4 years (±11.1), sex ratio: 1.4(88men/65 women).probable type 2 diabetes (92.20%) probable type 1 diabetes (6.5%).mean duration of diabetes: 9years. Mild anemia: 34.6% with mean Hb 11.98g/dl; moderate: 49% with mean Hb 9.65g/dl and severe 16.3% with mean Hb 6.76g/dl. Microcytic hypochromic anemia (30.7%), normocytic hypochromic anemia (18.3%), normocytic normochromic anemia (27.5%), microcytic normochromic anemia (20.9%) and macrocytic anemia (2.6%). Etiology: Probable inflammatory origin (50.3%) Renal insufficiency (24.1%) Martial deficiency (3.4%) Etiological factor not found (22.2%) Martial assessment, at the patient's expense, not performed (96%).
Conclusion: Anemia is a frequent biological abnormality in diabetics in Gabon. It is most often moderate, and most often related to infectious and renal causes.
Keywords: anemia, diabetes, inflammation, renal failure
CHUL, libreville hospital; eGFR, estimated glomerular filtration rate; Hb, hemoglobin; HbA1c, glycated hemoglobin; MCHC, corpuscular hemoglobin concentration; MCV, average corpuscular volume
A deficiency in the oxygen-carrying capacity of the blood due to a decrease in erythrocyte mass or a decrease in blood hemoglobin (Hb) concentration may indicate anemia.1 Developing countries are experiencing an increase in the prevalence of diabetes,2 associated with a high risk of microvascular complications. The prevalence of diabetes in Gabon has increased from 0.7% in 19943 to an estimated 10.5.9% in 2013.2 The prevalence of long-term complications of diabetes is expected to increase accordingly due to the difficulty of the disease2 and suboptimal management of people with diagnosed diabetes.4 Some complications of diabetes may be accompanied by anemia. For example, anemia is common in diabetes, with a prevalence of 13% in a European population,5 23% in an Australian population6 and up to 46.5% in a Caribbean population.7
Chronic kidney disease does not explain all cases of anemia in diabetes, which resign from an interaction between several factors: renal function, functional deficiency in erythropoietin, nutritional deficiencies, chronic inflammation, iatrogenic causes and infectious diseases.8 As a result, the development of the tendency in diabetic patients, even in the absence of overt nephropathy, and it is more severe9 negatively impacting the quality of life of diabetic patients.10 Anemia is also an important prognostic factor for cardiovascular disease and all-cause mortality in people with diabetes.11 Early identification and correction of anemia has been shown to reduce the rate of progression and even delay the onset of some microvascular complications12 as well as improve the quality of life of diabetic patients.13
Current guidelines for the management of diabetes do not recommend routine screening for anemia. Although reports on the prevalence and predictors of anemia in people with diabetes exist.
Moreover, such information is scarce in sub-Saharan Africa where other potential contributing factors such as infectious diseases and genes as well as nutritional deficiencies are very common and may aggravate the burden of anemia. This study aimed to estimate the pathogenesis of anemia associated with patients hospitalized for diabetes in Gabon.
Study design, setting and population
We conducted a descriptive retrospective study involving all consenting patients who had been hospitalized for diabetes in the endocrinology department of the University Hospital of Libreville (CHUL), and covered a one-year activity period: 01 January to 31 December 2017. CHUL is a tertiary care hospital located in Libreville, the capital of Gabon (about 703940 inhabitants).14 The endocrinology department of CHUL is the main referral center for endocrine diseases and diabetes in Libreville. Data were sought from the records of patients hospitalized for diabetes during this period and collected on a form. Patients with diagnosed type 2 diabetes, regardless of gender and aged 20 years or older, were included. All patients with known hematologic disease, any diagnosis of diabetes less than 1 year old, or those who had received a blood transfusion in the previous 4 months were excluded.
Data collection
The demographic characteristics of the patients, the type of diabetes, the diabetes treatments received were studied.
The hemoglobin level was obtained from the complete blood count. Mean corpuscular volume (MCV), mean corpuscular hemoglobin concentration (MCHC) and reticulocytes were used to characterize the anemia. The etiological factors of anemia were selected from the analysis of clinical and para-clinical signs. Complementary examinations analyzed to orient to one cause or another of the anemia were: C-reactive protein; serum iron, transferrinemia, ferritinemia, iron saturation coefficient, creatinemia, glomerular filtration rate.
Definitions
Patients were classified as anemic according to the World Health Organization (WHO) criteria (Hb <12 g / dl for women and <13 g / dl for men).15 On the basis of mean corpuscular volume (MCV), the anemia was classified as microcytic (MCV <80 fl), normocytic (MCV between 80 and 100 fl) or macrocytic (MCV> 100 fl). Mean corpuscular hemoglobin concentration (MCHC) was used to characterize anemia as hypochromic (MCHC <32 g / dl) or normochromic (MCHC≥32 g / dl). Anemia was central if the reticulocyte count was < 120,000. Platelets
> 350,000/mm3, C-reactive protein > 10 mg/l were in favour of an inflammatory origin, the ferriprive character was retained if the serum iron< 100mg/l. The estimated glomerular filtration rate (eGFR) (ml / min / 1.73 m2) was calculated using the abbreviated formula Modification of diet in kidney disease as eGFR = 186 × [serum creatinine (mg / l)] - 1.154 × [age (years)] - 0.203 × 0.192 × (0.742 for women).16
Was included: any hospitalized patient with a hemoglobin (Hb) level less than: 13g/dl (men),12g/dl(women).Anemia was mild if Hb in women between10.9 and11.9g/dl and in men between10.9and12.9 g/dl , moderate if Hb between 8 and 10.9 g/dl and severe if Hb<8g/dl.
Statistical analysis
Data were presented as mean and standard deviation for continuous variables and as numbers and percentages for categorical variables. Data were tested for normality using histograms, comparison of means and medians. Data were analyzed with SPSS for Windows:EPI-INFO version 3.5.
We did not include patients with missing data in the statistical analysis.
Of the 782 records of patients hospitalized in the CHUL Endocrinology Department, 153 (19.6%) met the criteria of our study and 12 were excluded (3 had hematological disease and 9 were children). The average age of these patients, aged between 20 and 89 years, was 54.4 years (±11.1). The age group most concerned was 45-60 years and represented 62 cases or 40.5% (Figure 1).
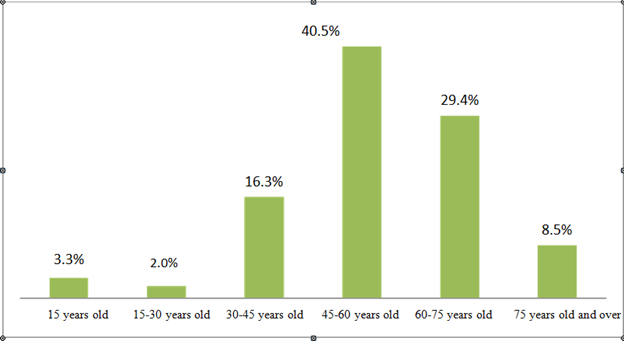
Figure 1 Distribution of patients according to age. univariate analysis, study of 153 patients from a group hospitalized for diabetes.
Sex
The male sex was the most representative with 57.5% of the patients registered giving a sex ratio of 1.4 (88 males/65 females) (Figure 2).
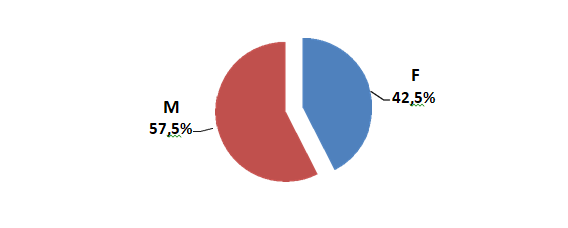
Figure 2 Distribution of patients according to gender. Univariate analysis, study of 153 patients from a group hospitalized for Diabetes.
Type of diabetes
Probable type 2 diabetes with 141 (92.2%) cases remains the most recurrent. Average duration of diabetes: 9 years (Figure 3).

Figure 3 Distribution of patients by type of diabetes. Univariate analysis, study of 153 patients from a group hospitalized for Diabetes.
Form of anemia
Anemia was mild in 34.6% with mean Hb 11.98g/dl; moderate in 49% with mean Hb 9.65g/dl and severe in 16.3% with mean Hb 6.76g/dl (Figure 4) (Table 1).
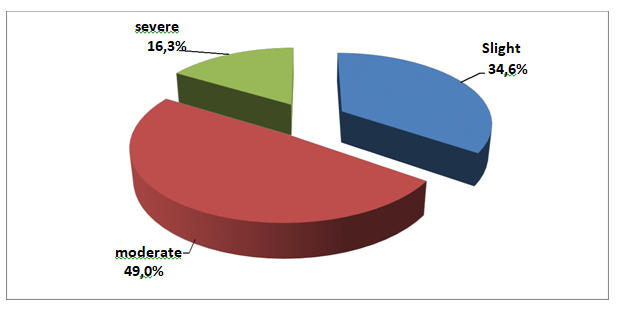
Figure 4 Distribution according to the forms of anemia. Univariate analysis, study on 153 patients from a group hospitalized for Diabetes.
Anemia |
Workforce |
Average Hb in |
|
% |
g/dl |
||
Slight |
53 |
34,64% |
11,98 |
moderate |
75 |
49,02% |
9,65 |
severe |
25 |
16,34% |
6,76 |
TOTAL |
153 |
100,0% |
|
Table 1 Forms of anemia
The above table shows that moderate anemia was predominant75 (49.0%) cases with an average of 9.65 g/dl followed by mild anemia 53 (34.6%) cases with an average of 11.98 g/dl. And finally severe anemia with 25 (16.3%) cases with an average of 6.76 g/dl (Figure 5).
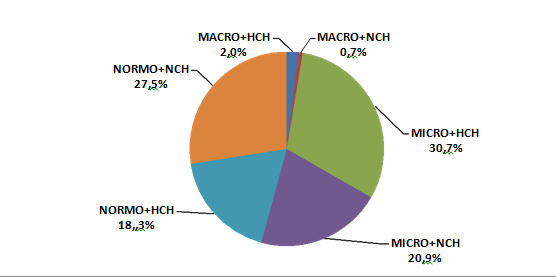
Figure 5 Distribution according to the type of anemia. Univariate analysis, study of 153 patients from a group hospitalized for Diabetes.
Classification of anemia
Hypochromic microcytic anemia was predominant with 47 (30.7%) cases, followed by normocytic normochromic anemia 42 (27.5%) cases. In terms of etiology, inflammatory origin was in the majority (50.3%), followed by renal failure (24.1%). Martial deficiency accounted for only 3.4% of the patients and in 22.2% of cases no etiological factor was identified. Martial assessment, at the patients' expense, was not available in 96% of cases (Figure 6).
In this study, the prevalence of anemia is estimated to be 19.6%. We also observed that the age group most affected is 45-60 years.
Anemia is common in diabetic patients and has a negative impact on patient well-being. It also impairs the ability to work, reduces quality of life17 and worsens cardiovascular health.11 The prevalence of anemia in our study (19.6%.) was relatively close to that reported Moroccans (22.59%).18The prevalence of anemia in diabetic patients reported elsewhere is higher than our results, 41% in Cameroon population,19 40% in Nigeria20 and 30.4%21 in Tehran. This is due to the difference in the quality of our samples. Our study is conducted on a population of hospitalized diabetics while theirs are done from patients followed in ambulatory.
The improvement of the management of the diabetic patient as a whole (through the popularization of management and the training of health professionals) could explain, among other things, the lower prevalence in our population compared to studies conducted a few years ago. However, other
Research is needed to investigate this prevalence of anemia in a broad spectrum of African populations with diabetes.
The high prevalence of inflammatory causes found in our study (50.3%) is comparable to several others in the literature18,22 and can be explained by the choice of our population (hospitalized patients), infection being one of the most frequent causes of diabetic imbalance. The renal cause (24.1% in our study) is the one that is more frequent in other populations made of patients followed in ambulatory.
The predominance of the microcytic form in our population, which is consistent with other populations,19,21 suggests the importance of deficiency causes, particularly martial deficiency, which is probably underestimated in our population (3.4%). This low proportion results from the inaccessibility of patients to all complementary examinations despite the availability of health insurance which only partially covers the costs of medical care in Gabon. This also explains the absence of etiology in several cases in this work (22.2%).
Our study shows that anemia was rather moderate in most cases (49%), which is also consistent with the population of Morocco22-25 and this can be explained by the improvement in the awareness of patients who no longer hesitate to go to hospitals in case of health problems as demonstrated by a similar work done a few years later in the same country18 where the mild form of anemia is dominant.
We acknowledge the following potential limitations of our study. Despite being conducted in a tertiary care hospital, the results may underestimate some of the actual causes of anemia in diabetic inpatients. In addition, this study did not include non-diabetic patients to identify causes that would be specific to diabetes, indicating the need for further research in this area. Reticulocyte counts and vitamin (vitamin B12 and folic acid) determinations were not assessed, nor was the search for hemoglobinopathies performed. However, we had a relatively large sample of diabetic patients and used reliable statistical tests to identify determinants.
In conclusion, the prevalence of anemia in the population of hospitalized diabetics in Gabon is high. Inflammatory cause and decreased renal function appear as the main determinants. Our results suggest that diabetic patients should be systematically screened for anemia, and other causes should be checked. Furthermore, the results raise questions regarding the additional economic burden for diabetic patients attributable to anemia, and the careful interpretation of HbA1c levels in sub-Saharan Africans.
None.
None.

©2022 Essono, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.