Journal of
eISSN: 2373-4345


Research Article Volume 15 Issue 2
1Clinical faculty in prosthodontics, School of Dentistry, Université de Montréal, QC, Canada
2Biostatistical Design and Analysis Center, Clinical and Translational Science Institute, University of Minnesota, USA
3Associate Professor, Division of Prosthodontics, Department of Restorative Sciences, School of Dentistry, University of Minnesota, USA
Correspondence: Dr. WookJin Seong, 9-470 Moos Tower, 515 Delaware St SE, Division of Prosthodontics, Department of Restorative Sciences, School of Dentistry, University of Minnesota, Minneapolis, MN 55455, USA
Received: April 05, 2024 | Published: April 29, 2024
Citation: Chea Y, Evans MD, Seong W. The effect of splinting crowns on multiple adjacent implants: a retrospective study. J Dent Health Oral Disord Ther. 2024;15(2):81-91. DOI: 10.15406/jdhodt.2024.15.00618
Purpose: The purpose of this study was to retrospectively evaluate the effects of splinting implant crowns against nonsplinted crowns on the failures and complications of multiple adjacent implants.
Material and methods: A retrospective chart review was conducted of all registered implant patients treated at the University of Minnesota School of Dentistry from 1988 to 2018. A total of 2738 implants within 1171 sections of 890 patients were examined retrospectively using an inclusion criteria of (1) two or more adjacent implants (section) present and (2) implants were restored by splinted crowns (Splinted group) or nonsplinted (individual) crowns (Nonsplinted group).
Results: An average follow-up interval was significantly longer (p < 0.0001) for Splinted (median 5.52 [IQR 1.97, 9.67] years) compared to Nonsplinted (3.76 [1.49, 6.54] years). Splinted group’s Hazard ratio (HR) for implant failure was 0.67 (95% CI 0.35–1.31, p = 0.24) relative to Nonsplinted, and estimated 5- and 10-year failures rates were 2.5 (1.3–3.7) vs. 3.0 (1.9–4.0)% and 8.7 (6.1–11.3) vs. 8.6 (5.7–11.3)%, respectively. Splinted group’s HR for total complication relative to Nonsplinted was 0.98 (95% CI 0.71–1.36, p = 0.92) and estimated 5- and 10-year complication rates were 24.7 (21.7-27.5) vs. 23.7 (21.1-26.3)% and 38.1 (34.2-41.7) vs. 42.1 (37.2-46.6)%, respectively. Three most common complications (Splinted/Nonsplinted, 10-year estimates) were crown decementation/dislodgement (20.8/13.0%), peri-implantitis (12.2/13.1%), and screw loosening (5.9/12.8%), while 3 failure causes (5-year estimates) were peri-implantitis (1.8/1.3%), implant fracture/metal collar flowering (0.3/1.1%), and soft tissue encapsulation (0.1/0.2%). When 380 Lifecore implants with higher failure rates (8.4% in 7.2 years) were excluded, the implant failure HR became lower 0.46 (0.22–0.99, p = 0.05) indicating significantly lower implant failure risk in Splinted compared to Nonsplinted, while the total complication HR did not change much 0.95 (0.64–1.40, p = 0.79). When compared per section, Splinted total complication HR went down to 0.75 (0.55–1.02, p = 0.07), indicating lower risk for complication in Splinted sections compared to Nonsplinted sections.
Conclusion: The trends of implant therapy of multiple adjacent implants have changed over the last three decades. The effects of splinting crowns of multiple adjacent implants were not significant in reducing implant failures or total complications. However, when the Lifecore implants mainly used in Splinted group during earlier phase (1988 – 2003) were excluded, the Splinted group showed significantly lower implant failure risk than Nonsplined group.
Keywords: multiple adjacent implants, splinted crowns, nonsplinted (individual) crowns, implant failures and complications
The development and advancement of dental implants have grown exponentially in the past 30 years and made possible the esthetic and functional replacement of natural teeth. Improvements have been made in design, materials, surface coatings, surgical and prosthetic techniques to decrease the healing time for osseointegration and concurrently to enhance the long-term outcomes.
Although they have shown high survival rates and long-term success, dental implants are susceptible to biological and prosthetic complications. Overload may cause mechanical complication/failure of the restoration and/or implant and biological failure of the surrounding bone.1–4 In order to minimize those complications, some authors recommended splinting implant restorations where biomechanical risks are high, such as posterior region in an attempt to distribute the occlusal forces over a bigger resistance area.5–7 A split-mouth prospective study of splinted ipsilateral implants and nonsplinted contralateral implants showed that all screw loosening complications occurred on the nonsplinted side for 5 of 15 patients.8 Studies have suggested that splinted prostheses can help decrease the harmful stress and strain on the peri-implant bone.9–11 A retrospective study found a higher survival rate for splinted posterior implants shorter than 8.5 mm compared to nonsplinted implants after an average follow-up time of 9.7 ± 3.7 years.7 A recent systematic review and meta-analysis concluded that there was no difference in the marginal bone loss and prosthetic complications of splinted and nonsplinted implant restorations but splinted restorations were associated with decreased implant failure.12
Poor plaque control and inability to clean is one of the risk factors of peri-implantitis.13 The 9th European Workshop on Periodontology stated that peri-implant mucositis is the precursor to peri-implantitis, as is gingivitis for periodontitis,14 even though peri-implant mucositis does not necessarily progress to peri-implantitis, similar to the causal relationship between gingivitis and periodontitis.13 With the onset of peri-implantitis, the pattern of bone loss can accelerate15 and lead to complete loss of osseointegration and implant failures if undiagnosed.16 A well-designed restoration with adequate accessibility for oral hygiene is an essential consideration to avoid the incidence of peri- implant mucositis and peri-implantitis.17 The rationale for designing individual implant restorations is that they allow for easier access to maintain proper and optimal hygiene,17 allow a better emergence profile18 and passive fitness.8,19 Nonsplinted restorations provide improved passivity of the framework, emergence profile and facilitate oral hygiene8,20 whereas splinted restorations require large quantities of metal and ceramic that increases the risk of veneer and framework fracture.21
The decision whether or not to splint adjacent implants in partially edentulous dentition has always been a source of controversy and there is currently no consensus regarding which prosthetic design is superior. Minimal and confusing clinical evidence with limited historic perspectives is available to help clinicians make the decision to splint or to restore independently.8,12,22,23
Therefore, the purpose of this long-term large-sample size retrospective clinical study is to evaluate the effects of splinting implant crowns against the nonsplinted (individual) crowns on the failure and complications of multiple adjacent implants. The null hypothesis is that implant failure and complications are not affected by splinting crowns (vs. nonsplinted individual crowns) of multiple adjacent implants.
In this retrospective study, data were collected from the clinical charts of patients who underwent dental implant therapy at the University of Minnesota School of Dentistry in the period of 1988 to 2018.
The study protocol was reviewed and approved by the Institutional Review Board of the University of Minnesota. By using implant placement and failure information from the implant office at the school and American Dental Association codes of dental implant crowns (D6058, D6059, D6061, D6062, D6064), a cohort of patients who have received dental implant crown treatment have been identified using paper charts (1988 to 2010) and an electronic chart system (axiUm) (2010 to 2018). From those cohorts, a subset of patients who had two or more adjacent implants being crowned individually or splinted in a group (defined as a ‘section’) has been identified (Figure 1). The implant-supported fixed complete or partial dentures with pontics, including cantilevered pontics, were excluded from this study. Implants that were placed outside of the school and that failed before the restorations were delivered were also excluded in this study.
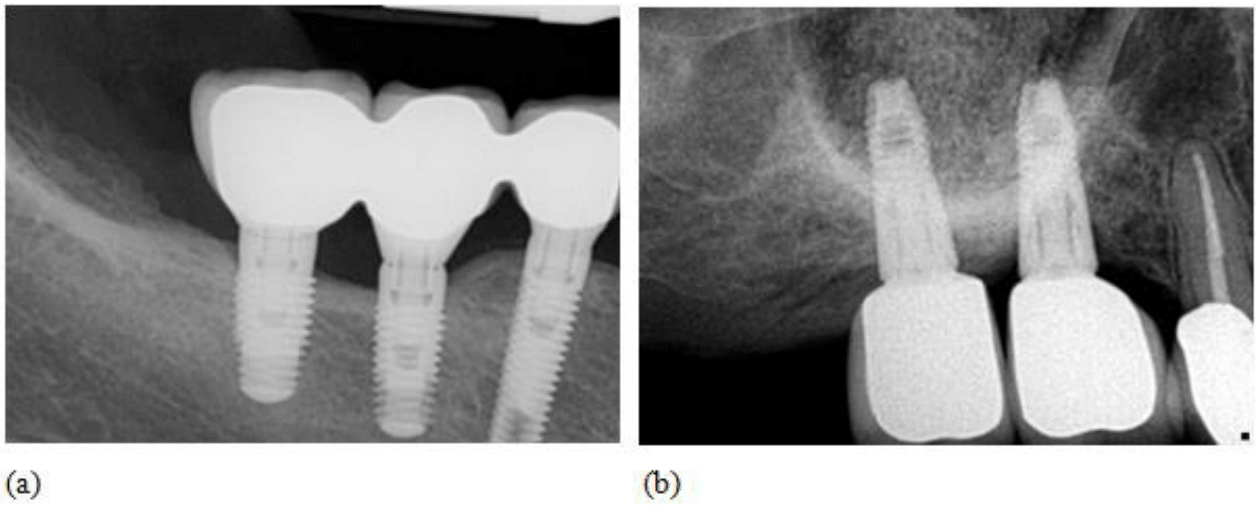
Figure 1 Radiographs showing (a) 3 adjacent implants in a Splinted group (splinted crowns) section and (b) 2 adjacent implants in a Nonsplinted group (individual crowns) section. A section is defined as two or more adjacent implants being crowned individually or splinted.
The charts were reviewed and data were collected and cross-checked by three examiners. Patients’ demographic data, including age, gender, medical history (diabetes, periodontitis), and habits such as smoking and bruxing or clenching were obtained from the patient’s records. Information about implant system used, length and diameter, implant-abutment connection type, additional surgical procedures (including sinus floor elevation and bone graft procedures), type of restorations, torque wrench use, and the presence of surgical or prosthetic complications and/or implant failures were also recorded. When any of this information was not available in the patient charts, it was recorded as “unknown”.
From the database (Splinted: 1113 implants vs. Nonsplinted: 1625 implants), the implant complications and failures rates were analyzed. Implant failures refer to implants that were removed from the patient’s mouth (e.g., severe bone loss, metal collar flowering) while implant complications refer to the implants that remain in patient’s mouth even with the complications such as screw loosening/fracture, crown decementation/dislodgement, porcelain fracture of crown, remade crowns, food impaction, and peri-implantitis. The follow-up duration was calculated from the date of crown delivery to the date of either implant failure (removal) or the last appointment date recorded.
After identifying a subset of Lifecore external hex implants with hydroxyapatite (HA) coating, which were used mainly between 1988 to 2003 and showed a high percentage of implant failure from peri-implantitis, subsequent analyses (Splinted: 776 implants vs. Nonsplinted: 1578 implants) were performed excluding all 380 Lifecore implants whether they were external hex or not, HA coated (67%) or not (33%). Further analyses on data of 6/1988 to 6/2003 (Splinted: 462 implants vs. Nonsplinted: 114 implants) and 7/2003 to 3/2018 (Splinted: 651 implants vs. Nonsplinted: 1511 implants) were performed to see how implant therapy trend has changed (data not shown).
Participant characteristics were compared among groups (those with splinted implant crowns, nonsplinted implant crowns, or both types of crowns) using the chi-square test for association or analysis of variance, and summarized using counts and proportions or means and standard deviations, for categorical and numeric characteristics respectively. Implant characteristics were compared between Splinted and Nonsplinted groups using similar tests and summaries. Time-to-event analyses were used to examine time from crown delivery to failure and time from crown delivery to complication, and compare risk of failure and complication between groups; specifically, mixed effects Cox proportional hazards models were fit using implant as the unit of observation, with a fixed effect term for splinted status, random effect intercept terms for participant and for section within participant to account for within-participant and within-section correlation of implant outcomes, and stratification by calendar year of crown placement. Similar models were fit using section as the unit of observation that included a random effect intercept terms for participant; these compared nonsplinted sections to splinted sections and excluded 36 mixed-type sections containing both nonsplinted and splinted crowns. The relationships between other factors (location, internal or external hex, torque wrench, screw or cement-retained, crown material type) and time to failure and time to complication were examined using similar Cox models. Results are summarized using hazard ratios (HR) with 95% confidence intervals. Survival curves and five- and ten-year failure and complication rates were estimated using the Kaplan-Meier estimator. Times from implant placement to crown delivery and follow up time intervals were compared by splinted status among all implants, and time to complication or failure among only those implants experiencing complications or failure, using the Wilcoxon rank-sum test and summarized using medians and first and third quartiles. Analyses were conducted using R version 4.0.324 including the coxme package version 2.2-16.25
A total of 2738 implants (1517 Zimmer, 394 Astra, 380 Lifecore, 268 3i, 115 Nobel Biocare, 64 others including Straumann, BioHorizons, Imtec) grouped in 1171 sections of 890 patients were included in this study. The number and distribution of Splinted and Nonsplinted group implants over the 1988-2018 are presented in Figure 2. An average follow-up interval was significantly longer (p < 0.0001) for Splinted group (5.52 year [1.97, 9.67]) compared to Nonsplinted group (3.76 year [1.49, 6.54]). Both crown delivery to 1st complication interval (2. 92y [0.92, 6.54] vs. 1.96y [0.62, 4.72], p = 0.002) and crown delivery to failure interval (7.28y [4.35, 8.83] vs. 4.24y [1.78, 5.98], p = 0.0001) were significantly longer in Splinted group (vs. Nonsplinted).
Out of total 890 patients, 73 patients (with 151 sections) had either 36 mixed-type sections (for example, 2 splinted crowns and one individual crown are next each other on 3 adjacent implants in a section) or both Splinted and Nonsplinted sections in their mouth. No significant differences of patient characteristics such as age, gender, medical history (diabetes, periodontitis), and habits such as smoking and bruxing or clenching were found among 3 (Splinted, Nonsplinted, Both) patient groups (data not shown).
When implant characteristics of Splinted and Nonsplinted groups are compared, no significant splinting patterns per anatomic locations (p = 0.99) were found (Table 1). For example, data did not support the notion that more splinted (against nonsplinted) crowns are used for posterior maxillary implants while more nonsplinted crowns are fabricated for maxillary anterior implants. External hex implant-abutment connection was used significantly higher percentages (p <0.01) in Splinted group (32.6%) compared to Nonsplinted group (4.2%). Screw-retained crowns were used significantly higher percentages (p < 0.01) in Nonsplinted (17.7%) compared to Splinted group (9.3%).
|
Variable |
Splinted |
Non splinted |
All |
p-value |
|
Number of total patients (n) ǂ |
319 |
498 |
890 |
|
|
Number of total sections (n) ǂ |
443 |
692 |
1171 |
|
|
Number of total implants (n) |
1113 |
1625 |
2738 |
|
|
Number of implants/section |
2.34 (±0.59) |
2.29 (±0.62) |
2.34 (±0.63) |
0.01* |
|
Number of total Lifecore implants (n) |
335 |
45 |
380 |
|
|
Average placement - exit period (year) |
6.45 (±4.98) |
4.57 (±3.77) |
5.33 (±4.40) |
<0.01* |
|
Location |
|
|
|
0.99 |
|
=Mn Ant |
11 (1.0%) |
16 (1.0%) |
27 (1.0%) |
|
|
=Mn Post |
541 (48.6%) |
799 (49.2%) |
1340 (48.9%) |
|
|
=Mx Ant |
110 (9.9%) |
159 (9.8%) |
269 (9.8%) |
|
|
=Mx Post |
451 (40.5%) |
651 (40.1%) |
1102 (40.2%) |
|
|
Implant diameter |
4.14 (±0.58) |
4.30 (±0.57) |
4.24 (±0.58) |
<0.01* |
|
Implant length |
12.5 (±1.9) |
11.9 (±1.6) |
12.1 (±1.7) |
<0.01* |
|
Implant-abutment connection |
|
|
|
<0.01* |
|
=Internal hex/Morse taper implants |
748 (67.2%) |
1551 (95.4%) |
2299 (84.0%) |
|
|
=External hex implants |
363 (32.6%) |
69 (4.2%) |
432 (15.8%) |
|
|
=Unknown |
2 (0.2%) |
5 (0.3%) |
7 (0.3%) |
|
|
Torque wrench (=Yes) |
627 (56.3%) |
1124 (69.2%) |
1751 (64.0%) |
<0.01* |
|
Crown retention |
|
|
|
<0.01* |
|
=Cement-retained |
957 (90.2%) |
1281 (82.1%) |
2238 (85.4%) |
|
|
=Screw-retained |
99 (9.3%) |
276 (17.7%) |
375 (14.3%) |
|
|
=Unknown |
5 (0.5%) |
3 (0.2%) |
8 (0.3%) |
|
|
Crown type |
|
|
|
<0.01* |
|
=All ceramic |
14 (1.3%) |
89 (5.5%) |
103 (3.8%) |
|
|
=Gold |
59 (5.3%) |
57 (3.5%) |
116 (4.2%) |
|
|
=PFM |
1032 (92.7%) |
1477 (90.9%) |
2509 (91.9%) |
|
|
=Unknown |
8 (0.7%) |
2 (0.1%) |
2 (0.1%) |
|
|
Opposing dentition (=Yes) |
1081 (97.1%) |
1578 (97.1%) |
2659 (97.1%) |
1.00 |
Table 1 Implant characteristics of two study groups. Displayed values are mean (±SD) for numeric variables and n (%) for categorical variables. All statistics are calculated excluding missing values
* indicates statistically significant differences.
ǂ Out of total 890 patients, 73 patients had either 36 mixed-type sections (for example, 2 splinted crowns and one individual crown are next each other on 3 adjacent implants in a section) or both Splinted and Nonsplinted sections in their mouth. The total of 1171 sections includes 443 splinted-only sections, 692 nonsplinted-only sections, and 36 mixed-type sections.
Hazard ratio (HR) for implant failure was 0.67 (95% CI 0.35–1.31, p = 0.24) for Splinted relative to Nonsplinted group and HR for total complication in Splinted group relative to Nonsplinted was 0.98 (95% CI 0.71–1.36, p = 0.92) (Table 2). Three most common complications (Splinted/Nonsplinted, 10-year estimates) were crown decementation/dislodgment (20.8/13.0%), peri-implantitis (12.2/13.1%), and screw loosening (5.9/12.8%). Splinted group implants had significantly more crown decementation/dislodgment (HR = 1.76, p = 0.004) while significantly less screw loosening (HR = 0.25, p = 0.001). When a crown decementation/dislodgment incidence occurs, it inevitably involves two or more implants in Splinted group whereas only one implant in the Nonsplinted group is involved. When 380 Lifecore implants were excluded, the implant failure HR of Splinted group became lower 0.46 (0.22–0.99, p = 0.05) indicating significantly lower failure risk in Splinted group compared to Nonsplinted, while the total complication HR of Splinted group did not change much 0.95 (0.64–1.40, p = 0.79). Kaplan-Meier survival curves for implant failure and complications of all 2738 implants and 2354 implants excluding Lifecore implants are presented in Figure 3.
|
|
|
|
Hazard ratio |
|
5-year rates |
10-year rates |
|||
|
|
Event |
Group |
Est |
95% CI |
p |
Est (%) |
95% CI |
Est (%) |
95% CI |
|
All implants
-2738 imp (1113 spl / 1625 nonspl) -1171 sec (443 spl / 692 non / 36 both) |
Implant failure |
Nonspl |
1 |
- |
- |
3.0 |
1.9-4.0 |
8.6 |
5.7-11.3 |
|
Splinted |
0.67 |
0.35-1.31 |
0.24 |
2.5 |
1.3-3.7 |
8.7 |
6.1-11.3 |
||
|
Total complications |
Nonspl |
1 |
- |
- |
23.7 |
21.1-26.3 |
42.1 |
37.2-46.6 |
|
|
Splinted |
0.98 |
0.71-1.36 |
0.92 |
24.7 |
21.7-27.5 |
38.1 |
34.2-41.7 |
||
|
Peri-implantitis |
Nonspl |
1 |
- |
- |
4.8 |
3.4-6.2 |
13.1 |
9.6-16.5 |
|
|
Splinted |
1.03 |
0.56-1.92 |
0.92 |
6.1 |
4.4-7.8 |
12.2 |
9.3-14.9 |
||
|
Crown decementation/dislodgement |
Nonspl |
1 |
- |
- |
7.5 |
5.9-9.1 |
13.0 |
10.1-15.7 |
|
|
Splinted |
1.76 |
1.20-2.58 |
0.004* |
13.7 |
11.4-16.0 |
20.8 |
17.7-23.9 |
||
|
Screw loosening |
Nonspl |
1 |
- |
- |
6.9 |
5.3-8.4 |
12.8 |
9.5-15.9 |
|
|
Splinted |
0.25 |
0.12-0.54 |
0.001* |
2.8 |
1.7-3.9 |
5.9 |
3.8-7.9 |
||
|
Excluding lifecore implants -2354 impǂ (776 spl / 1578 nonspl) -1007 sec (304 spl / 673 non / 30 both) |
Implant failure |
Nonspl |
1 |
- |
- |
3.0 |
1.9-4.1 |
8.9 |
5.9-11.8 |
|
Splinted |
0.46 |
0.22-0.99 |
0.05* |
1.6 |
0.4-2.7 |
7.7 |
4.5-10.8 |
||
|
All complications |
Nonspl |
1 |
- |
- |
24.1 |
21.4-26.8 |
42.4 |
37.3-47.1 |
|
|
Splinted |
0.95 |
0.64-1.40 |
0.79 |
23.9 |
20.4-27.3 |
35.5 |
30.8-39.8 |
||
|
Peri-implantitis |
Nonspl |
1 |
- |
- |
5.0 |
3.6-6.5 |
13.8 |
10.0-17.4 |
|
|
Splinted |
0.73 |
0.34-1.55 |
0.41 |
3.5 |
1.9-5.1 |
7.4 |
4.7-10.0 |
||
|
Crown decementation/dislodgement |
Nonspl |
1 |
- |
- |
7.7 |
6.0-9.4 |
12.2 |
9.5-14.8 |
|
|
Splinted |
1.84 |
1.24-2.74 |
0.003* |
14.3 |
11.4-17.1 |
21.5 |
17.6-25.2 |
||
|
Screw loosening |
Nonspl |
1 |
- |
- |
6.8 |
5.2-8.3 |
12.9 |
9.4-16.2 |
|
|
Splinted |
0.20 |
0.08-0.50 |
0.001* |
2.4 |
1.1-3.6 |
4.5 |
2.3-6.7 |
||
Table 2 Time to Event (TTE) Hazard Ratio (HR) and the estimate (%) analysis of per implant failure and total and 3 most common complications (95% Confidence Interval (CI))
*indicates statistically significant differences.
ǂ2354 implants were analyzed instead of 2358 (2738 total implants – 380 Lifecore implants) because 4 implants lacked implant brand information.
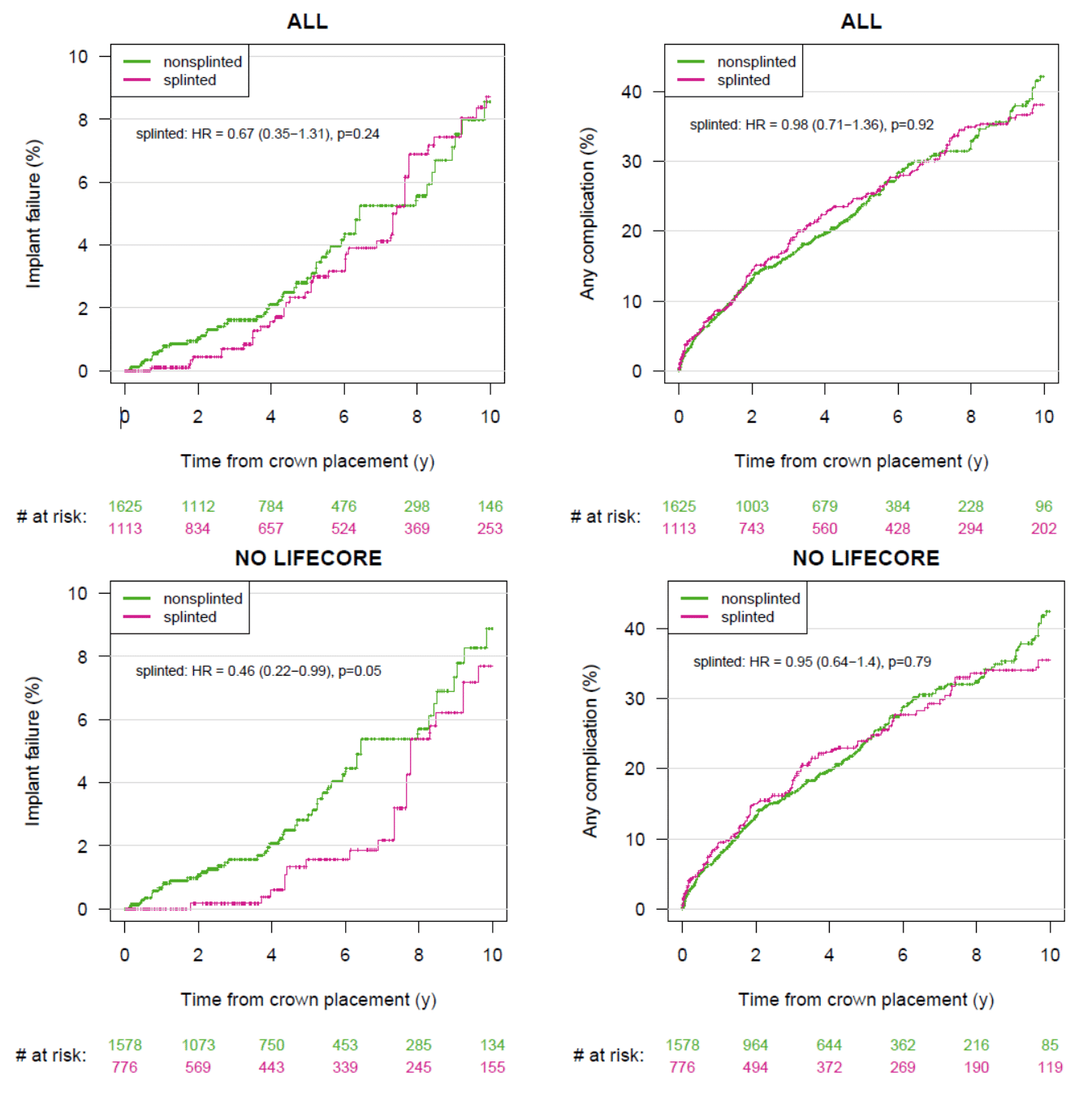
Figure 3 Kaplan-Meier survival curves for implant failure and complication of (a) all implants and (b) implants without 380 Lifecore implants.
When compared per section (grouped two or more adjacent implants) as a unit for analyses, Splinted group’s total complication HR went down to 0.75 (0.55–1.02, p = 0.07) compared to per implant HR of 0.98, indicating lower risk for complication in Splinted sections compared to Nonsplinted sections (Table 3). The estimated 10-year failures and total complication rates for Splinted vs. Nonsplinted sections were 13.6 (8.6-18.3) vs. 16.9 (10.7-22.6) and 41.4 (35.0-47.2) vs. 55.9 (48.0-62.5)%, respectively. Three common complications (Splinted/Nonsplinted 10- year estimates) were crown decementation/dislodgement (21.7/22.4%), peri-implantitis (14.8/17.9%), and screw loosening (8.0/21.4%). From the data excluding 380 Lifecore implants, Splinted sections showed lower HRs for implant failure (0.49, 0.23-1.04, p = 0.06), total complications (0.74, 0.53-1.02, p = 0.06), and peri-implantitis (0.56, 0.14-2.26, p = 0.42) among all analyses. Interestingly, analyses done on early era (1988 to 2003) vs. late era (2003 to 2018) (data not shown) indicated more Splinted section implant failures during early era but less failures during late era, compared to Nonsplinted section. This finding can be explained by that Lifecore implants had higher failure rates (8.4% = 32/380 over 7.2 year) compared to non-Lifecore implants (3.1% = 73/2354 over 4.9 year) (Table 4) and the majority of Lifecore implants belonged to Splinted group (88% = 335/380) (Table 1) and used during early era (1988 to 2003) (83.7% = 318/380).
|
|
|
|
Hazard ratio |
|
5-year rates |
10-year rates |
|||
|
|
Event |
Group |
Est |
95% |
p |
Est (%) |
95% |
Est (%) |
95% |
|
All implants (1135 sec 2620 imp) -Nonsplint 692 sec 1583 imp -Splinted 443 sec 1037 imp |
Implant failure |
Nonspl |
1 |
- |
- |
6.5 |
4.0- 8.9 |
16.9 |
10.7-22.6 |
|
Splinted |
0.66 |
0.35-1.24 |
0.20 |
4.5 |
2.1- 6.9 |
13.6 |
8.6-18.3 |
||
|
Total complications |
Nonspl |
1 |
- |
- |
36.0 |
31.3-40.3 |
55.9 |
48.0-62.5 |
|
|
Splinted |
0.75 |
0.55-1.02 |
0.07 |
25.6 |
20.8-30.0 |
41.4 |
35.0-47.2 |
||
|
Peri-implantitis |
Nonspl |
1 |
- |
- |
7.8 |
5.1-10.5 |
17.9 |
11.3-24.1 |
|
|
Splinted |
0.90 |
0.49-1.64 |
0.72 |
6.2 |
3.5- 8.9 |
14.8 |
9.8-19.6 |
||
|
Crown decementation/dislodgement |
Nonspl |
1 |
- |
- |
14.1 |
10.7-17.4 |
22.4 |
16.8-27.7 |
|
|
Splinted |
1.04 |
0.68-1.60 |
0.84 |
12.6 |
9.0-16.1 |
21.7 |
16.3-26.7 |
||
|
Screw loosening |
Nonspl |
1 |
- |
- |
12.7 |
9.5-15.8 |
21.4 |
15.1-27.2 |
|
|
Splinted |
0.26 |
0.14-0.48 |
<0.001* |
3.9 |
1.8- 6.0 |
8.0 |
4.3-11.5 |
||
|
Excluding lifecore implants (977 sec 2249 imp) -Nonsplint 673 sec 1540 imp -Splinted 304 sec 709 imp |
Implant failure |
Nonspl |
1 |
- |
- |
6.5 |
3.9- 9.0 |
17.3 |
10.9-23.3 |
|
Splinted |
0.49 |
0.23-1.04 |
0.06 |
3.5 |
0.7- 6.3 |
9.6 |
4.0-14.8 |
||
|
All complications |
Nonspl |
1 |
- |
- |
36.5 |
31.7-40.9 |
56.9 |
48.6-63.8 |
|
|
Splinted |
0.74 |
0.53-1.02 |
0.06 |
25.9 |
20.0-31.4 |
39.7 |
31.7-46.8 |
||
|
Peri-implantitis |
Nonspl |
1 |
- |
- |
8.1 |
5.3-10.8 |
18.8 |
11.7-25.3 |
|
|
Splinted |
0.56 |
0.14-2.26 |
0.42 |
4.0 |
1.4- 6.6 |
10.9 |
5.5-16.0 |
||
|
Crown decementation/dislodgement |
Nonspl |
1 |
- |
- |
14.2 |
10.7-17.6 |
22.1 |
16.4-27.3 |
|
|
Splinted |
1.07 |
0.68-1.68 |
0.76 |
12.7 |
8.2-16.9 |
22.7 |
15.6-29.2 |
||
|
Screw loosening |
Nonspl |
1 |
- |
- |
12.5 |
9.3-15.7 |
21.7 |
15.1-27.8 |
|
|
Splinted |
0.24 |
0.11-0.49 |
0.0001* |
3.6 |
1.1- 6.1 |
5.4 |
1.8- 8.9 |
||
Table 3 Time to Event (TTE) Hazard Ratio (HR) and the estimate (%) analysis of per section implants failures and total and 3 most common complications (95% Confidence Interval (CI)). The 36 mixed-type sections (for example, 2 splinted crowns and one individual crown are next each other on 3 adjacent implants in a section) were excluded in this analysis
*indicates statistically significant differences.
Table 4 shows estimated implant failure rates with time to failure and the 3 most common failure types (5-year estimates) for Splinted/Nonsplinted groups; peri-implantitis (1.8/1.3%), implant fracture/metal collar flowering (0.3/1.1%), and soft tissue encapsulation (0.1/0.2%). Radiographic examples of different implant failure types are presented in Figure 4.
|
Variable |
Splinted |
Nonsplinted |
All |
|
Number (N) of implants |
1113 |
1625 |
2738 |
|
N of implants with failures |
55 |
50 |
105 |
|
Number (N) of Lifecore implants |
335 |
45 |
380 |
|
N of Lifecore implants with failures |
31 |
1 |
32 |
|
Total implant failure rates |
105/2738 = 3.8%; time to failure 5.2 [2.4, 8.6] years |
||
|
- Splinted implant failure rates |
55/1113 = 4.9%; time to failure 6.4 [2.9, 10.4] years |
||
|
- Nonsplinted implant failure rates |
50/1625 = 3.1%; time to failure 4.7 [2.3, 7.4] years |
||
|
Lifecore implant failure rates |
32/380 = 8.4%; time to failure 7.2 [3.7, 11.7] years |
||
|
- Splinted implant failure rates |
31/335 = 9.3%; time to failure 7.2 [3.7, 12.1] years |
||
|
- Nonsplinted implant failure rates |
1/45 = 2.2%; time to failure 6.0 [3.6, 11.4] years |
||
|
Non-Lifecore implant failure rates |
73/2354 = 3.1%; time to failure 4.9 [2.4, 8.3] years |
||
|
- Splinted implant failure rates |
24/776 = 3.1%; time to failure 6.1 [2.7, 10.0] years |
||
|
- Nonsplinted implant failure rates |
49/1578 = 3.1%; time to failure 4.6 [2.3, 7.3] years |
||
|
Variable |
Splinted |
Nonsplinted |
All |
|
Failed Implant numbers (Lifecore Imp) |
55/1113 (31/335) |
50/1625 (1/45) |
105/2738 (32/380) |
|
Mn Ant |
0/11 (0/2) |
0/16 (0/1) |
0/27 (0/3) |
|
Mn Post |
23/541 (14/179) |
31/799 (0/18) |
54/1340 (14/197) |
|
Mx Ant |
0/110 (0/38) |
1/159 (1/13) |
1/269 (1/51) |
|
Mx Post |
32/451 (17/116) |
18/651 (0/13) |
50/1102 (17/129) |
|
Implant failure types |
5-year est (%) |
5-year est (%) |
5-year est (%) |
|
Peri-implantitis |
1.8 |
1.3 |
1.5 |
|
Implant fracture/metal collar flowering |
0.3 |
1.1 |
0.7 |
|
Soft tissue encapsulation |
0.1 |
0.2 |
0.1 |
Table 4 Implant failure rates (%) and time to failure (median [Q1, Q3]) from the crown delivery. All statistics are calculated excluding missing values
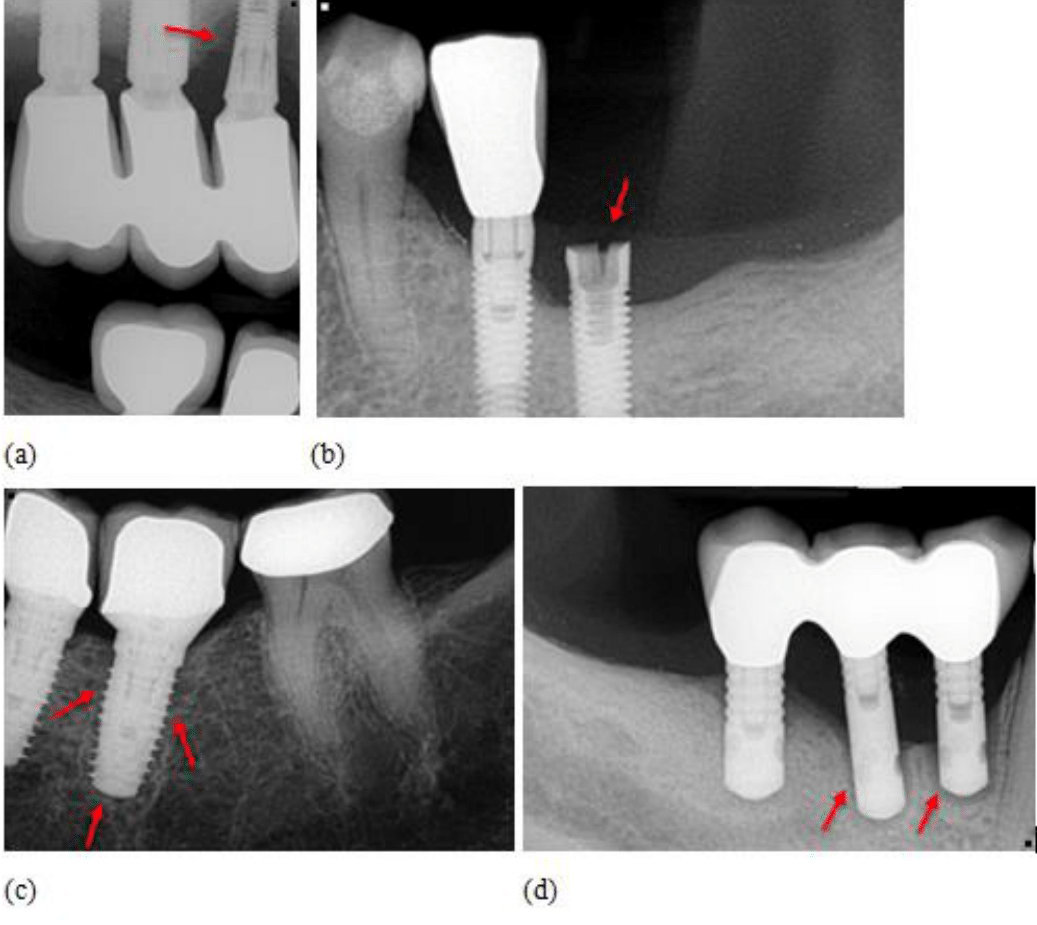
Figure 4 The examples of different implant failure types; (a) Peri-implantitis induced #5 implant failure of Splinted group, (b) Metal collar fracture induced #19 implant failure of Nonsplinted group, (c) Soft tissue encapsulation induced #19 implant failure of Nonsplinted group, (d) Lifecore HA-coated (Sustain) implant failure from the peri-implantitis bone loss of Splinted group.
Risk factors on implant failure and complication for the Splinted and Nonsplinted groups over the entire follow-up period are presented in Figure 5. A multivariate Cox regression model for time to implant failure showed that in Splinted group, maxillary posterior implant anatomical location (vs. mandibular posterior) had 2.57 HR (CI: 1.45- 4.56, p = 0.001) and external hex abutment-implant connection (vs. internal hex/Morse taper) had 4.4 HR (CI: 2.02- 9.58, p = 0.0002) (Figure 5). The time to implant complication model indicated that, in Nonsplinted group, maxillary anterior anatomic location (vs. mandibular posterior) had 0.55 HR (CI: 0.35-0.87, p = 0.01) and screw- retained restoration (vs. cemented-retained) had 1.65 HR (CI: 1.24-2.19, p = 0.0006).
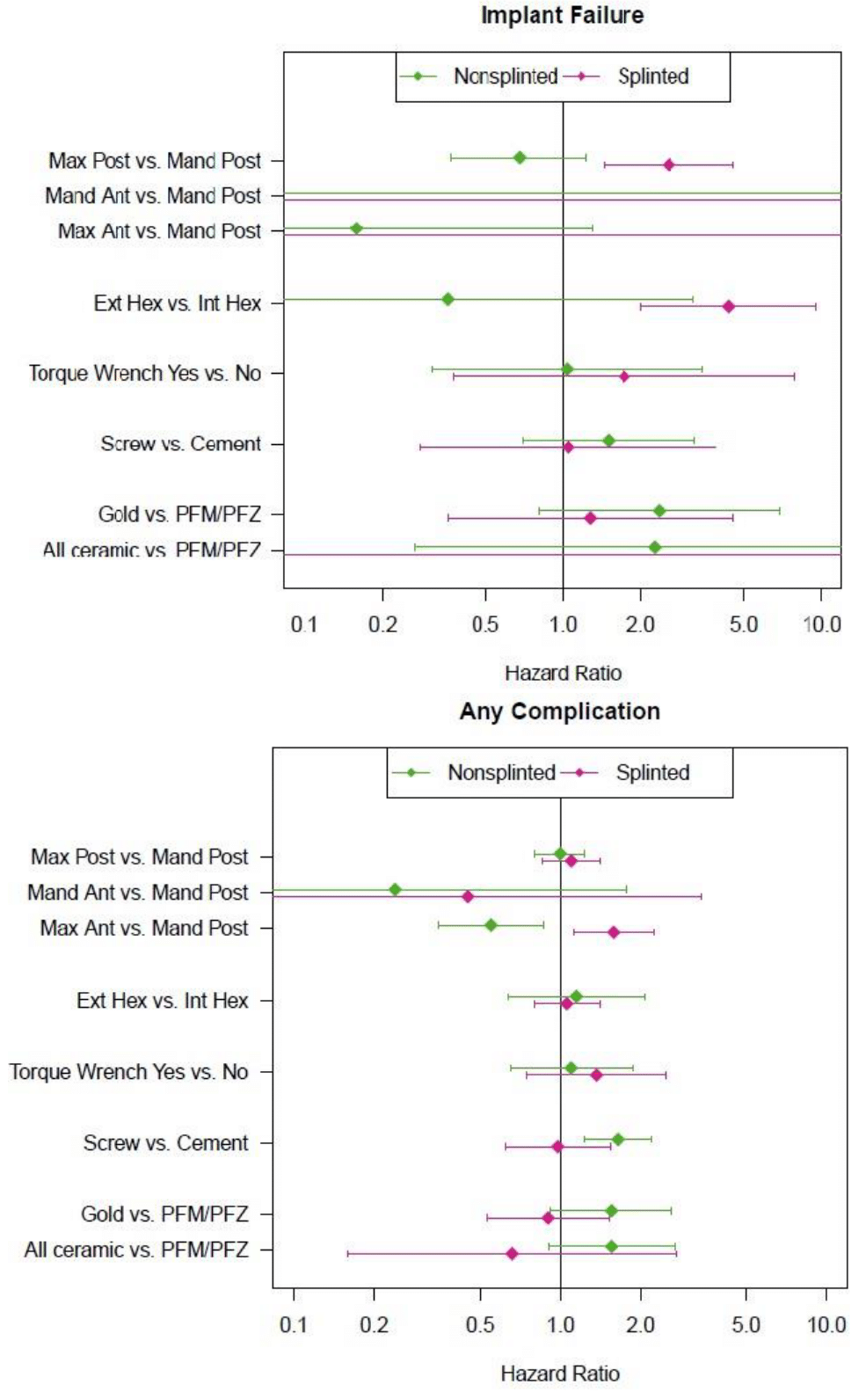
Figure 5 Forest plot showing risk factors for implant failure and complication in the Splinted and Nonsplinted groups. Hazard ratios from multivariable Cox models are shown with 95% confidence intervals. Intervals that do not cross 1 indicate p<0.05.
Obviously, higher implant failures and complications were estimated when the data were reviewed per section rather than per implant because in each section there are two or more adjacent implants present. Follow-up time compensated estimated 10-year rates of any complication for Nonsplinted (vs. Splinted) section were 55.9% (CI: 48.0-62.5) vs. 41.4% (35.0-47.2) (Table 5), which means more than half of Nonsplinted implant sections will experience/experienced implant complications at 10-year mark. The 10-year implant failure estimates of Splinted (vs. Nonsplinted) were 10.8/2.7% in Lifecore implant-only data, in contrast to 7.7/8.9% in Non-Lifecore implant data, indicating Splinted Lifecore implants failed in higher percentage while Splinted non-Lifecore implants failed in lower percentage in comparison to Nonsplinted corresponding implants.
|
|
|
|
|
|
Hazard ratio |
|
5-year rates |
10-year rates |
|||
|
Cohort |
Observation unit |
Event |
Group |
nǂ |
Est |
95% CI |
p |
Est (%) |
95% CI |
Est (%) |
95% CI |
|
All implant |
Per implant |
Implant failure |
Nonspl |
1625 |
1 |
- |
- |
3.0 |
1.9- 4.0 |
8.6 |
5.7-11.3 |
|
Splinted |
1113 |
0.67 |
0.35-1.31 |
0.24 |
2.5 |
1.3- 3.7 |
8.7 |
6.1-11.3 |
|||
|
All Com plication |
Nonspl |
1625 |
1 |
- |
- |
23.7 |
21.1-26.3 |
42.1 |
37.2-46.6 |
||
|
Splinted |
1113 |
0.98 |
0.71-1.36 |
0.92 |
24.7 |
21.7-27.5 |
38.1 |
34.2-41.7 |
|||
|
Per section |
Implant failure |
Nonspl |
692 |
1 |
- |
- |
6.5 |
4.0- 8.9 |
16.9 |
10.7-22.6 |
|
|
Splinted |
443 |
0.66 |
0.35-1.24 |
0.20 |
4.5 |
2.1- 6.9 |
13.6 |
8.6-18.3 |
|||
|
All Com plication |
Nonspl |
692 |
1 |
- |
- |
36.0 |
31.3-40.3 |
55.9 |
48.0-62.5 |
||
|
Splinted |
443 |
0.75 |
0.55-1.02 |
0.07 |
25.6 |
20.8-30.0 |
41.4 |
35.0-47.2 |
|||
|
Lifecore implant |
Per implant |
Implant failure |
Nonspl |
45 |
1 |
- |
- |
2.7 |
0.0- 7.8 |
2.7 |
0.0- 7.8 |
|
Splinted |
335 |
3.06 |
0.20-47.06 |
0.42 |
4.5 |
1.8- 7.1 |
10.8 |
6.3-15.2 |
|||
|
All Com plication |
Nonspl |
45 |
1 |
- |
- |
16.9 |
4.6-27.6 |
43.5 |
18.0-61.0 |
||
|
Splinted |
335 |
1.54 |
0.38- 6.26 |
0.55 |
26.2 |
20.7-31.2 |
42.5 |
35.4-48.7 |
|||
|
Per section |
Implant failure |
Nonspl |
19 |
1 |
- |
- |
7.1 |
0.0-19.7 |
7.1 |
0.0-19.7 |
|
|
Splinted |
139 |
2.06 |
0.24-17.97 |
0.51 |
6.5 |
1.7-11.1 |
20.4 |
10.8-29.0 |
|||
|
All Com plication |
Nonspl |
19 |
1 |
- |
- |
23.5 |
0.3-41.3 |
38.8 |
0.0-63.3 |
||
|
Splinted |
139 |
0.94 |
0.31- 2.85 |
0.91 |
24.5 |
16.2-32.0 |
43.4 |
32.1-52.7 |
|||
|
Non-Lifecore implant |
Per implant |
Implant failure |
Nonspl |
1578 |
1 |
- |
- |
3.0 |
1.9- 4.1 |
8.9 |
5.9-11.8 |
|
Splinted |
776 |
0.46 |
0.22-0.99 |
0.05* |
1.6 |
0.4- 2.7 |
7.7 |
4.5-10.8 |
|||
|
All Com plication |
Nonspl |
1578 |
1 |
- |
- |
24.1 |
21.4-26.7 |
42.4 |
37.3-47.1 |
||
|
Splinted |
776 |
0.95 |
0.64-1.40 |
0.79 |
23.9 |
20.4-27.3 |
35.5 |
30.8-39.8 |
|||
|
Per section |
Implant failure |
Nonspl |
673 |
1 |
- |
- |
6.5 |
3.9- 9.0 |
17.3 |
10.9-23.3 |
|
|
Splinted |
304 |
0.49 |
0.23-1.04 |
0.06 |
3.5 |
0.7- 6.3 |
9.6 |
4.0-14.8 |
|||
|
All Com plication |
Nonspl |
673 |
1 |
- |
- |
36.5 |
31.7-40.9 |
56.9 |
48.6-63.8 |
||
|
Splinted |
304 |
0.74 |
0.53-1.02 |
0.07 |
25.9 |
20.0-31.4 |
39.7 |
31.7-46.8 |
|||
Table 5 Follow-up time compensated per implant and per section failure and complication hazard ratio (95% CI) and 5-year & 10-year estimates (95% CI) from different sample cohort groups
*indicates statistically significant differences.
ǂOut of total 2738 implants, 4 implants (2 each in Splinted and Nonsplinted groups) lacked implant brand information. Therefore only 1623 (instead of 1625) Splinted implants and 1111 (instead of 1113) Nonsplinted implants were analyzed for Lifecore implant and Non-Lifecore implant cohorts.
A lot more nonsplinted crowns were fabricated on posterior maxillary and mandibular implants during Era 2 (7/2003 to 3/2018) compared to Era 1 (6/1988 to 6/2003) (Table 6). During the Era 1, about 88.7% (165/186) & 82.8% (240/290) of posterior maxillary & posterior mandibular implants were restored with splinted crowns while only 31.2% (286/916) & 28.7% (301/1050) were with splinted crowns during Era 2. For both Splinted and Nonsplinted groups, the trends of using wider implant and shorter implant were observed from Era 1 to 2. The 72.2% (312/432) of all external hex implants included in this study were restored with splinted crowns during Era 1, while only 3.3% (71/2156) implants used during Era 2 was external hex implants, regardless of splinted or nonsplinted status.
|
Variable\n |
Level |
Splinted |
Nonsplinted |
All |
Missing |
||||
|
Era 1 |
Era 2 |
p |
Era 1 |
Era 2 |
p |
N (%) |
(%) |
||
|
462 |
651 |
113 |
1511 |
2738 |
|||||
|
Location (%) |
Mn Ant |
7(1.5) |
4(0.6) |
0.026 |
5(4.4) |
11(0.7) |
<0.001* |
27(1.0) |
0 |
|
Mn Post |
240(51.9) |
301(46.2) |
50(43.9) |
749(49.6) |
1340(48.9) |
||||
|
Mx ant |
50(10.8) |
60(9.2) |
38(33.3) |
121(8.0) |
269(9.8) |
||||
|
Mx Post |
165(35.7) |
286(43.9) |
21(18.4) |
630(41.7) |
1102(40.2) |
||||
|
Imp diameter (mean (SD)) |
3.93(0.48) |
4.29(0.60) |
<0.001* |
3.90(0.52) |
4.33(0.57) |
<0.001* |
4.24(0.58) |
0.3 |
|
|
Imp length |
12.71(1.94) |
12.32(1.78) |
0.001* |
12.84(2.00) |
11.82(1.57) |
<0.001* |
12.13(1.75) |
0.3 |
|
|
(mean(SD)) |
|||||||||
|
Imp-Abut connection (%) |
Internal hex/ |
150(32.5) |
598(92.1) |
<0.001* |
64(56.6) |
1487(98.7) |
<0.001* |
2299(84.2) |
0.3 |
|
Morse taper |
|||||||||
|
External Hex |
312(67.5) |
51(7.9) |
49(43.4) |
20(1.3) |
432(15.8) |
||||
|
Torque wrench |
No |
16(9.1) |
55(10.5) |
0.686 |
3(12.5) |
95(7.9) |
0.662 |
169(8.8) |
29.9 |
|
Yes |
160(90.9) |
467(89.5) |
21(87.5) |
1103(92.1) |
1751(91.2) |
||||
|
Crown retention (%) |
Cement-retained |
371(85.5) |
586(94.2) |
<0.001* |
88(88.9) |
1193(81.8) |
0.1 |
2238(85.6) |
4.6 |
|
Screw-retained |
63(14.5) |
36(5.8) |
11(11.1) |
265(18.2) |
375(14.4) |
||||
|
Crown type (%) |
All ceramic |
2(0.4) |
12(1.8) |
<0.001* |
4(3.5) |
85(5.6) |
0.63 |
103(3.8) |
0.4 |
|
Gold |
39(8.6) |
20(3.1) |
4(3.5) |
53(3.5) |
116(4.3|) |
||||
|
PFM/PFZ |
413(91.0) |
619(95.1) |
106(93.0) |
1371(90.9) |
2509(92.0) |
||||
Table 6 Implant characteristics comparison between two periods (Era 1: 1988/6/23 - 2003/6/30 vs. Era 2: 2003/7/1 – 2018/3/9) of two study groups. Displayed values are mean (±SD) for numeric variables and n (%) for categorical variables. All statistics are calculated excluding missing values
*indicates statistically significant differences.
Splinting crowns of multiple adjacent implants did not significantly reduce the risk for implant failures or total complications in either per implant or per section analyses (Tables 2, 3, & 5). However, among implants that did fail or experience complication, it took significantly longer time to develop prosthetic and implant complications or implant failures in the Splinted group. The recent systematic review and meta-analysis (total 4215 implants [2768 splinted and 1447 nonsplinted] in 2185 patients from 19 studies) by Batista et al.,12 showed statistically significant higher implant survival rates for splinted restorations (99.1%) than nonsplinted restorations (96.5%) (P<.001). Our results generally agreed in that the Splinted group showed lower chance (HR = 0.67, p = 0.24) for implant failure than Nonsplinted group, though the difference was not statistically significant. However, when all Lifecore implants were excluded this difference did reach significance (HR = 0.46, p = 0.05).
Prior studies reported a significantly higher occurrence of screw loosening with single implant crowns compared to the splinted implant crowns.1,8 The data from this study shows that screw loosening tends to occur significantly less in Splinted group compared to the Nonsplinted (HR = 0.25, p < 0.001, 10 year estimated rates, 5.9% vs. 12.8%, respectively). These results are in line with a 10.1 year follow-up retrospective study that reported that prosthetic complication rates of splinted restorations supported by narrow implants were significantly lower than those of single crowns (15.4% vs 39.4% respectively, p = .04).26
Unlike screw loosening, Splinted group did not show lower crown decementation/dislodgement HRs. The occurrence of decementation in Splinted crowns is comparable to Nonsplinted crowns (per section HR = 1.04, p = 0.84) and when that happens, 2 or more implants were affected (per implant HR = 1.76, p = 0.004). The 85.4% of all crowns included in this study were cement-retained, splinted or not and the default cements were temporary luting cement or elastomeric implant resin cement. Difficulty of achieving framework passivity of splinted restorations27 and the common use of weaker provisional cements in those implant-supported restorations28 might explain why the Splinted sections’ decementation occurred as often as Nonsplinted sections, even though the Splinted crowns’ total cement surface area might have been more than the double of the Nonsplinted crowns’.
The prevalence of peri-implant mucositis and marginal bone loss were not evaluated in this retrospective study. Prior studies reported greater crestal bone loss in splinted implants than non-splinted implants due to less hygienic prosthetic design29 and stress-shielding of crestal bone.30 More recent studies found that splinting implants, whether they’re recently placed or surviving implants, have a high implant survival rate, low incidence of complications and an acceptable bone marginal level. Other studies using finite element analysis suggested that splinting prostheses helps decrease the harmful stress and strain on the peri-implant bone, thereby preserving the crestal bone.5,10,11 Some studies supported that the marginal bone levels can be maintained in nonsplinted implants even though the implant is subjected to higher forces of different vectors.31,32 Recently, two systematic reviews agreed that there is no difference in the crestal bone loss between splinted and nonsplinted implants.12,22
The sixth European workshop on periodontology reported that the interproximal area in a splinted fixed prosthesis is an area difficult to clean which can act as a food trap for plaque and bacterial accumulation. This may lead to peri- implant mucositis, peri-implantitis and subsequently bone loss around the implant.33 Interestingly, we found that Splinted group’s peri-implantitis risks were not higher than Nonsplinted group’s except Era 1 (6/1988 to 6/2003) when the majority of Lifecore HA coated implants were used in Splinted group. The Splinted group’s peri-implantits HR over Nonsplinted was 1.03 (p = 0.92) and 10-year estimated peri-implantitis rates were 12.2% (Splinted) and 13.1% (Nonsplinted). Once all Lifecore implants were excluded, the Splinted group’s peri-implantits HR over Nonsplinted was 0.73 (p = 0.41) and 10-year estimated peri-implantitis rates were 7.4% (Splinted) and 13.8% (Nonsplinted). Several studies reported the prevalence of peri-implantitis in splinted implants to be between 3.2% and 6%, similar to our study. (Vigolo, Hsu, Vladimir 2022). This finding refutes Lee et al.’s retrospective study (408 implants in 234 patients) reported significantly elevated incidence rates of peri-implant mucositis (P = .002) and peri-implantits (P = .046) in the 2 implant splinted group compared to single implant group.1 A cross-sectional retrospective study with 349 implants found that the over-contoured restoration and splinting to both mesial and distal adjacent implants had a high risk of peri-implantitis.35 It is not clear why our study did not agree with above clinical studies. A systemic review showed that the included animal studies36 did not reveal an association between overload and peri-implant bone loss in the absence of peri-implant inflammation, whereas in its presence, overload seemed to aggravate the peri-implant tissue breakdown.37,38 In this study, the implant restorations in the nonsplinted group implants showed a higher incidence of screw loosening (12.8% of 10 year estimates) and this combined with the higher risk of overloading on the nonsplinted implant might have contributed to the onset of peri-implantitis, in the presence of peri-implant inflammation. Even though it is difficult to conclude whether the inability to clean or overloading in the presence of peri-implant inflammation is the more prominent factor on the onset of bone loss leading to the peri-implantitis, it is clear that the posterior region has higher parafunctional forces as well as difficult oral hygiene access. This might explain why more implant failures with majority from peri-implantitis were reported in posterior region, especially in posterior maxilla than the anterior region (Table 4). Studies reported that maxillary implants were 2.98 times more likely to develop peri-implantitis (P < .05)39 and insertion in the maxilla and less occlusal support of natural teeth correlated with peri-implantitis development.40 Research is needed to determine whether splinting over the individual restorations will make plaque control significantly more difficult so that the prevalence of peri-implantitis can happen more. In this study, splinting did not induce more peri-implantitis. This study collected data retrospectively therefore data can portray the reality in the university clinical setting. Generally low timely-maintenance and low compliance of daily quality oral hygiene seen on university patients might explain why peri-implantitis risk were not different, splinted or nonsplinted.
The forest plot suggests that maxillary anterior adjacent implants (compared to mandibular posterior implants) had significantly fewer complications (HR = 0.55, p = 0.01) with Nonsplinted crowns and more complications (HR = 1.59, p = 0.009) with Splinted crowns (Figure 5). These data suggest that fabricating nonsplinted individual crowns might induce less implant and prosthetic complications when multiple adjacent implants are located in the maxillary anterior region. Despite the lack of statistical significance describing the association between the implant survival and the anatomic location of the implant, most of the implant fractures were clinically seen in the posterior maxilla and mandible (Table 4), where bite forces are estimated to be 300% greater compared to anterior jaw segments.41 Another interesting finding was that there were no significant splinting patterns found per anatomic locations (p = 0.99) and around 59% of implants were restored by Nonsplinted crowns across the all 4 anatomic regions (Table 1). This might indicate that dentists practiced either Splinted or Nonsplinted crowns exclusively based on their belief and preferences, regardless of the anatomic locations of multiple adjacent implants.
Over the last three decades, several trends of implant therapy have been observed. The biggest trend is that higher percentages of Nonsplinted crowns were used in Era 2 (69.9% = 1511/(651+1511)) compared to Era 1 (19.8% = 114/(462+114)) (Table 6). This nonsplinted crown use trend was even more prominent in posterior mandible (Era 1: 17.2% à Era 2: 71.3%) and posterior maxilla (Era 1: 11.7% à Era 2; 67.8%). For both Splinted and Nonsplinted groups, implant diameter became larger, and length become shorter. Also, external hex implant use percentage has been significantly reduced from Era 1 (Splinted 67.5%, Nonsplinted 43.4%) to Era 2 (Splinted 43.4%, Nonsplinted 1.3%). Although external hex connection implants are still used today in the European and United States markets,42 single restorations with internal connection implants have become the primary choice for implant-supported restorations. With its self-locking characteristics,43 the internal connection helps to overcome the abutment and prosthesis-retaining screw loosening problem seen when using external hex prosthesis connection systems.44
Per section analyses can infer how many clinic visits were needed to address the implant and prosthetic complications or failures. For example, when crown dislodgement complication happens in a three implant splinted section, this can be recorded as one complication in ‘per section’ analysis and this complication can be addressed at one clinic visit. However, it is recorded as three separate complications happening on three implants in ‘per implant’ analysis, even though this complication can be handled at one clinic visit. Three common complications per section (Splinted/Nonsplinted, 10-year estimates) were crown decementation/dislodgement (21.7/22.4%), peri-implantitis (14.8/17.9%), and screw loosening (8.0/21.4%) (Table 3). All 3 major complications were estimated to happen more frequently in Nonsplinted sections. Follow-up time compensated estimated 10-year rates of any complication for Nonsplinted (vs. Splinted) section were 55.9% (CI: 48.0-62.5) vs. 41.4% (35.0-47.2) (Table 5), which means more than half of Nonsplinted implant sections will experience implant complications and clinic visits at the 10-year mark.
The limitations of this study are (1) results might have been affected by institution-specific variables such as frequent use of Lifecore HA-coated external hex implants during Era 1 (6/1988 to 6/2003) and (2) the implants were placed and restored mainly by residents and dental students. Lifecore HA-coated implants showed higher failure rates (8.4%) compared to non-Lifecore implants (3.1%) in our study. The detachment and degradation of HA- coating from chemical, cellular activities, and functional stresses over time have been reported to increase the susceptibility to bacterial colonization and peri-implantitis.45,46
The effects of splinting crowns of multiple adjacent implants were not significant in reducing implant failures or total complications. However, among implants that developed complications or failures, these took significantly longer time to develop in the Splinted crown group. When compared per section, Splinted total complication HR went down to 0.75 (0.55–1.02, p = 0.07), indicating lower risk for complication in Splinted sections compared to Nonsplinted sections. When subgroup of Lifecore implants with higher failure rates were excluded, the implant failure HR of Splinted became lower 0.46 (0.22–0.99, p = 0.05), indicating significantly lower implant failure risk in Splinted compared to Nonsplinted. The trends of fabricating more nonsplinted crowns on wider and shorter implants were observed, even in posterior maxilla and mandible. With this new trend, a future study on this topic is warranted.
Research reported in this publication was supported by the National Center for Advancing Translational Sciences of the National Institutes of Health Award Number UL1TR002494. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. The authors gratefully acknowledge Dr. Nathan Hanson, Mr. Brad Sukut, Ms. Kriti Bagdi, and Dr. Jan Groth for collecting and organizing data.
The authors declare that there are no conflicts of interest.

©2024 Chea, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.