Journal of
eISSN: 2373-4345


Clinical Paper Volume 11 Issue 5
1Postgraduate Program in Dentistry, Federal University of Sergipe, Brazil
2School of Dentistry, Federal University of Pelotas, Brazil
3Postgraduate Program in Health and Behavior, Catholic University of Pelotas, Brazil
Correspondence: Vanessa dos Santos Viana, Postgraduate Program in Dentistry, Federal University of Sergipe, Brazil
Received: June 25, 2020 | Published: September 10, 2020
Citation: Viana VS, Fernandez MS, Nunes FS, et al. Parental caregivers perceptions of oral health-related quality of life in children with autism spectrum disorder. J Dent Health Oral Disord Ther. 2020;11(5):132-137. DOI: 10.15406/jdhodt.2020.11.00531
The aim of this study is to assess the impact of oral conditions on the quality of life (QoL) of children and adolescents with autism spectrum from the perspective of their parent-caregivers. A convenience sample, including 40 children and adolescents with autism, aged 6 to 14, attended in seven institutions for people with special health care in the state of Sergipe, Brazil. It was used the Brazilian version of the Parental-Caregivers Perceptions Questionnaire (P-CPQ) and the Family Impact Scale (FIS), which are applied to evaluate the perception of parents or caregivers on oral health-related quality of life (OHRQoL) of children and adolescents. The clinical oral examination was performed for the prevalence of dental caries and assessment of oral hygiene. The global score for the P-CPQ in the sample ranged from 0 to 63, with a mean of 13.52 (9.05). 97.5% of mothers reported that oral conditions had an impact on OHRQoL. The increase in years of schooling (p=0.016) of caregivers was associated to greater perception regarding their child's OHRQoL. Most children and adolescents with autism had no caries experience and presented good to moderate oral hygiene. We did not find differences in OHRQoL scores according to the oral hygiene status and prevalence of dental caries. This study suggested that caregiver literacy has played a role in OHRQoL in children and adolescents with autism. Further studies with a larger sample size are needed to assess the influence of other oral health measures on QoL in this population.
Keywords: Autism spectrum disorder, quality of life, oral health
ASD, autism spectrum disorders; QoL, quality of life; OHRQoL, oral health-related quality of life; ISHCN, individuals with special health care needs; P-CPQ, parental-caregivers perceptions questionnaire; FIS, family impact scale; dmft/DMFT, the decayed, missing, and filled teeth index; OHI-S, oral hygiene index; OS, oral symptoms; FL, functional limitations; E-WB, emotional well-being; S-WB, social well-being
Autism spectrum disorders (ASD) are a group of neurodevelopmental disorders characterized by impairments in social interaction and communication, as well as repetitive behaviors and restricted interests.1 The ASD encompasses autism, pervasive developmental disorder not otherwise specified, and Asperger's syndrome.2 The heterogeneous nature of ASDs suggests that multiple etiologic factors can be involved, but it has been proposed that genetics is related to the 25% of cases.3
The global prevalence estimates of ASD is 62/10.000.4 The increase in prevalence rates of ASD observed in the last decades has been associated to the changes in the diagnostic criteria, improved identification and public awareness, and access to health services.5 The age at diagnosis ranges from 3 to 6 years, but there is increasing evidence that diagnosis in the second year of life is possible in some children.2 Because of the lifelong nature of autism symptoms, co-occurring behavior problems, and health concerns, individuals with ASD commonly continue to live with parents into adulthood,6 which may affect parenting behavior and later outcomes of individuals with this condition.7
In recent years, quality of life (QoL) has increasingly been studied in individuals with ASD, especially among children and adolescents with classic autism. It has been found large differences in QoL between people with and without autism across the lifespan,8 and the level of independence in daily activities seems to be a significant predictor of QoL domains, including physical and psychological health, and social relationships.9 Moreover, the family QoL of children with autism seems to be strongly influenced by the health of child, severity of the child’s needs, and access and engagement in recreation activities.10 QoL seems to be an useful index of parents' adjustment to their child's need and is an important component in obtaining a full understanding of the experiences of children with autism and their families.11
Children and adolescents with autism are extremely dependent on their caregivers to perform basic health care and oral hygiene.12 The most common oral problems found in these patients are dental hygiene, dental caries and gingivitis,13 which may be related to the difficulty of dealing with the prevention of biological and social etiological factors of dental caries in early childhood and its development over time.14,15 Recently, it was shown that problems related to cognitive function or communicational skills may prevent any child from expressing oral pain and discomfort, thereby challenging their caregivers to detect, interpret and communicate the child’s needs to the dental staff.16 In addition, the stressful life experience may compromises the individual’s stability and ability to cope of function.10
Studies evaluating the caregiver’s perception of oral health-related quality of life (OHRQoL) in children and adolescents with autism are needed to improve care for this population. To the best of our knowledge, only two studies were performed to use the parental/caregiver perception to assess the OHRQoL of children with autism.12,17 The aim of this study is to evaluate the impact of oral health conditions on the QoL of children and adolescents with autism, from the caregivers’ perspective.
Study design
This is a cross-sectional study, in which data collection was carried out through dialogued interviews with the heads of children with ASD and oral clinical examination in them. The survey was carried in two institutions to support individuals with special health care needs (ISHCN) in the state of Sergipe, Brazil. The variables related to the social context of the guardians were age, marital status, education and the number of children. The independent variables studied were dichotomized according to the median or were grouped into categories according to homogeneity or frequency distribution to verify the association between the outcomes.
Sample and recruiting
The study consisted of a convenience sample, formed by pairs of children with ASD and their mothers, duly registered and attended at the institutions supporting the ISHCN in the municipality of Aracaju (Sergipe, Brazil) selected for this study.
The choice of support units for ISHCN in the respective municipalities occurred due to the social representativeness of these institutions since they serve a large part of the disabled population of the municipalities included in this study, as well as the lack of health information in this group in Brazilian computerized databases. Those responsible for the children were contacted by phone, informed about the study and, upon acceptance, a meeting was held with those who spent the most time taking care of the children to present the research objectives.
Inclusion and exclusion criteria
To be eligible for the study, participants had to meet the following inclusion criteria: be registered in the institutions covered by the study, be included in the age group between 6 and 14 years old, present a medical diagnosis of ASD (International Classification of Diseases and Related Health Problems code: F84.0) and not have any other type of disability. The medical diagnosis was obtained through the medical records provided by the institutions. Also, guardians should spend at least 12 hours a day with the child. Participants were excluded due to the lack of information in the clinical record, the inability to attend the place where the study was being conducted, and the refusal to participate.
Data collection
On the day of the data collection, the caregiver was invited to answer two questionnaires, one related to the demographic and socioeconomic characteristics and another on the children’s OHRQoL. The questionnaires were collected in face-to-face interviews by one research assistant blind to the oral examinations and impairment characteristics of the child. The interviews were performed before the oral clinical examination of the children and adolescents. Research organizers were blinded from results until the end of the study to avoid social responsibility bias and reporting bias associated with confidentiality.
Oral health related quality of life (OHRQoL)
Data on quality of life and impact on the family were collected using the Brazilian versions of the Parental-Caregiver Perceptions Questionnaire (P-CPQ) and the Family Impact Scale (FIS).18,19
The P-CPQ is a reliable measure that assesses the parent caregiver's perception of the quality of life about children's oral health. In general, it consists of an automatic questionnaire, composed of 33 questions, using the 5-point Likert-type answer options, which assess the perceptions of parents-caregivers about the impacts of oral diseases on the quality of life of children and adolescents from 6 to 14 years. The 33 items of the P-CPQ are distributed in different subscales, which are: "oral symptoms" (OS), "functional limitation" (FL), "emotional well-being" (E-WB) and "social well-being" (S-WB).19
For the P-CPQ scale, the final score ranges from 0 to 132, with high scores indicating a greater negative perception of caregivers concerning the quality of life-related to their children's oral health.19 The FIS is an evaluation scale that analyzes the effects of children's oral disorders on the functioning of their family, referring to the frequency of events in the previous three months. The instrument consists of 14 items divided into four domains: parent/family activity, parent/family emotions, family conflict, and financial burden. The final score for the FIS scale ranges from 0 to 56, where the highest score means the greatest impact of the child's oral condition on the family's quality of life.18
Oral clinical examination and measures
The oral clinical examination was carried out by the evaluators of the Postgraduate Program in Dentistry at the Federal University of Sergipe, in an environment with natural lighting, with the use of an odontoscope, spherical tip probe (0.5mm), cotton and surgical gloves. According to the criteria established by the World Health Organization, the verification of the experience of dental caries and oral hygiene was measured through the Index of Decayed, Lost and Filled Teeth for primary dentition (dmft) and permanent dentition (DMFT), and Oral Hygiene Index (OHI-S), respectively.
For children with mixed dentition, the caries index was assessed by the sum of the components d +m /D+M+F. The dmft/DMFT was categorized according to the experience of dental caries: dmft/DMFT 0=caries-free; 1 to 2=low experience; from 3 to 4=moderate experience and ≥5=high experience.20
The condition of oral hygiene, assessed by the OHI-S index, is based on the amount of debris (DI-S) and dental calculations (CI-S) that affect the six representative surfaces of the teeth in the mouth. The surfaces examined for OHI-S were selected from four posterior and two anterior teeth (first right upper molar, right upper central incisor, first left upper molar, lower left central incisor, first left lower molar, and first left lower molar). The vestibular surfaces were examined for all teeth, with the exception of the lower molars, where the lingual surfaces were examined.
The OHI-S value was organized from the sum of DI-S and CI-S. The oral hygiene index can vary between 0 to 3.0 and be classified as good oral hygiene (0 to 0.6), regular oral hygiene (0.7 to 1.8) or poor oral hygiene (1.9 to 3.0), according to the model suggested by Greene and Vermillion.21
Statistical analysis
Statistical analysis was conducted using SPSS 25.0. Data were expressed as means and standard deviation (SD). Inferential statistics was tested using Mann-Whitney U test and the Kruskal-Wallis, followed by Student-Newman-Keuls multiple comparisons test. The level of significance was considered when p <0.05.
Ethical aspects
This study was carried out by the principles of the Declaration of Helsinki and with Resolution 196/1996 of the National Health Council of Brazil, receiving a favorable opinion from the Research Ethics Committee of the Federal University of Sergipe, under the number of order approval protocol 1.639.022.
The mean (SD) age of guardians was 42.2 (7.3) years. Most of caregivers were mothers (100%), married (70%), and had more than 9 years of schooling (57.5%), a mean of 2 children. We found that the increase in years of schooling (p= 0.016) of caregivers was associated to greater perception regarding their child's OHRQoL (Table 1). Thirty-nine (97.5%) families received financial support from the government.
|
Variables |
N |
Overall P-CPQ |
P-value |
FIS |
P-value |
|
Age |
|||||
|
<40 years |
12 |
12.08 (7.26) |
0.575£ |
1.33(2.99) |
0.302£ |
|
≥40 years |
28 |
14.14 (9.77) |
0.36 (1.89) |
||
|
Marital status |
|||||
|
Single |
9 |
18.56 (17.38) |
0.172§ |
0.21 (0.83) |
0.726§ |
|
Married |
28 |
11.46 (3.36) |
2.22 (4.41) |
||
|
Separated/divorced/widowed |
3 |
17.67 (6.03) |
0 (0) |
||
|
Years of schooling |
|||||
|
5–9 |
17 |
11.76 (3.51) |
0.016£ |
0.70 (2.22) |
0.722£ |
|
≥9 |
23 |
14.82 (11.49) |
0.59 (2.42) |
||
|
Number of children |
|||||
|
One |
10 |
14.30 (5.65) |
0.051§ |
1.00 (3.16) |
0.998§ |
|
Two |
20 |
10.70 (3.64) |
0.30 (0.97) |
||
|
Three or more |
10 |
18.40 (15.81) |
1.00 (3.16) |
||
Table 1 Mean difference between demographic and socioeconomic characteristics of caregivers for P-CPQ and FIS (n= 40)
The mean age (SD) of children was 11.1 (2.7) years and most of them were male (65%). Most children and adolescents (97%) did not perform daily self-care activities of oral hygiene, had history of breastfeeding (90%) and bottle-feeding (97%), and all of them reported daily consumption of sugary drinks and foods, including sweet soda, cakes and biscuits. The median tooth brushing frequency with fluoride toothpaste was 2 times per day. Most children and adolescents (95%) had regular dental consultation in the public healthcare services.
The global score for the P-CPQ in the study population ranged from 0 to 63, with a mean of 13.52 (9.05). Overall, 97.5% of mothers reported that oral conditions had an impact (P-CPQ scores >0) on the health-related quality of life of children and adolescents. Of them, 37mothers (94.8%) reported experiencing oral symptoms and functional limitations in the previous 3 months, but only 2 (5.1%) reported emotional well-being impacts. One mother reported social well-being impact (2.6%). Only 4mothers (10%) reported any impact of oral health of children and adolescents with autism on the family quality of life. The mean scores for P-CPQ and FIS are detailed shown in Table 2.
|
Scale |
Number of items |
Possible range |
Observed range |
Mean (SD) |
|
P-CPQ |
||||
|
Total scale |
33 |
0-132 |
0-63 |
13.52 (9.05) |
|
Subscales |
||||
|
Oral symptoms |
6 |
0-24 |
0-13 |
8.95 (3.35) |
|
Functional limitations |
8 |
0-32 |
0-16 |
3.50 (3.76) |
|
Emotional well-being |
8 |
0-32 |
0-21 |
0.77 (3.64) |
|
Social well-being |
11 |
0-44 |
0-17 |
0.42 (2.68) |
|
FIS |
14 |
0-56 |
0-10 |
0.65 (2.28) |
Table 2 Descriptive data of overall OHRQoL and its subscales (n= 40)
Oral health of children and adolescents was described as “fair” by 42.5% of mothers, “good” or “very good” by 22.5% and “poor” by 35%. On the question whether the overall well-being of their children is affected by the oral/orofacial conditions, 67.5%, 10%, 10%, and 12.5% reported “a lot”, “some”, “not at all”, and “very little”, respectively.
Higher scores were observed in the subscales related to the functional limitation, emotional well-being and social well-being for mothers with higher years of schooling; the results were not statistically significant (Figure 1).
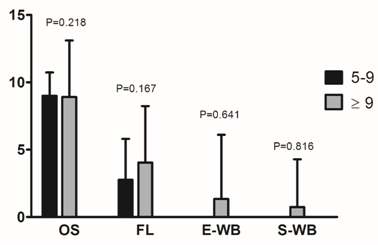
Figure 1 Subscales mean scores for P-CPQ in relation to years of schooling. Different letters mean statistically different results (p < 0.05; Student-Newman-Keuls multiple comparisons test).
Twenty-three (57.5%) children and adolescents had no caries experience. Of the 15 (42.5%) children and adolescents with experience of dental caries (dmft/DMF≥1), only 2 (11.8%) were classified as high prevalence (dmft/DMFT≥5). The mean of dmft/DMFT index was 1.25 (2.44). Twenty-six (65%) children and adolescents presented good to moderate oral hygiene (OHI-S=0.0-1.8). The mean of OHI-S index was 1.34 (0.94). We did not find differences in OHRQoL scores according to the oral hygiene status and prevalence of dental caries in children and adolescents with autism (Table 3).
|
Clinical condition |
n |
Overall P-CPQ |
OS* |
FL* |
E-WB* |
S-WB* |
FIS |
|
Severity of dental caries |
|||||||
|
Caries free, dmft+DMFT=0 |
23 |
11.30 (3.61) |
8.60 (4.12) |
2.70 (2.09) |
0 (0) |
0 (0) |
0.26 (0.91) |
|
Low prevalence, dmft+DMFT=1-2 |
11 |
13.45 (4.10) |
9.55 (2.20) |
3.45 (3.88) |
0.90 (3.01) |
0 (0) |
1.81 (4.04) |
|
Moderate prevalence, dmft+DMFT=3-4 |
4 |
23.00 (26.73) |
8.50 (1.00) |
5.00 (7.39) |
5.25 (10.5) |
4.25 (8.5) |
0 (0) |
|
High prevalence, dmft+DMFT≥5 |
2 |
20.50 (5.00) |
10.50 (0.70) |
10.00 (5.65) |
0 (0) |
0 (0) |
0 (0) |
|
P-value§ |
0.138 |
0.539 |
0.141 |
0.866 |
0.883 |
0.927 |
|
|
Oral hygiene |
|||||||
|
Good, OHI-S = 0.0-0.6 |
7 |
11.57 (2.93) |
7.85 (4.52) |
3.71 (3.40) |
0 (0) |
0 (0) |
0 (0) |
|
Fair, OHI-S = 0.7-1.8 |
19 |
14.05 (12.81) |
8.21 (3.60) |
3.57 (4.35) |
1.63 (5.21) |
0.89 (3.9) |
0.84 (2.43) |
|
Poor, OHI-S = 1.9-3.0 |
14 |
13.78 (3.42) |
10.50 (1.50) |
3.28 (3.29) |
0 (0) |
0 (0) |
0.71 (2.67) |
Table 3 Distribution of the P-CPQ and FIS scores in relation to dental caries and oral hygiene (n= 40)
*OS, oral symptoms; FL, functional limitations; E-WB, emotional well-being; S-WB, social well-being; § kruskal-wallis
In the present study, we found a low prevalence of dental caries and a satisfactory oral hygiene between children and adolescents with autism, and a positive association between mothers’ education and better scores of child's OHRQoL. Furthermore, the median tooth brushing frequency was 2 times per day and most children and adolescents had regular dental consultation in the public healthcare services. Twice daily tooth brushing is recommended by the American Dental Association, the American Academy of Pediatric Dentists and the American Academy of Pediatrics as a low-cost strategy to reduce risk of childhood caries. Although there are reasons to expect mothers may find twice daily tooth brushing difficult to achieve due to increased demands on time and resources associated with the child’s behavior or medical conditions,22 the findings of this study suggest that good oral hygiene in children and adolescents with autism can be achieved through a combination of regular professional dental services, parents' perceived skill to carry out tooth brushing as the part of their child's daily routines and knowledge that oral health problems may have negative effects on QoL.
There are few studies describing oral health and dental needs of children and adolescents with autism and the evidences of an increased risk of oral health problems among these subjects are conflicting,13,23 which may be related to the differences in oral health knowledge, attitude, and skills of the caregivers, the level of independency of children, and socioeconomic factors. In addition, it has been shown that caregiver literacy has potential implications for the pediatric population.24–26 Health literacy is defined as “the capacity to obtain, process, and understand basic health information and services needed to make appropriate health decisions” and has recently emerged as an important determinant of health and related outcomes.27 Evidence suggests that low caregivers’ health literacy is associated with poor children’s health outcomes,28 including oral health status29 and QoL.30
Although we found a good oral health between children and adolescents with autism and a positive association between caregiver literacy and OHRQoL, most children were bottle-fed and consumed cariogenic foods and beverages. Evidence is known about the role of non-milk extrinsic sugars in the etiology of dental caries,31–33 but the effects of cariogenic diet might be weaker for children who brush their teeth with fluoride toothpaste or who have greater exposure to fluoridated water.34 In addition, the children and adolescents included in this study may have consumed acceptable levels of sugar over the lifetime, which may have contributed to the low prevalence of dental caries. Unfortunately, we were unable to provide a dose-response relationship between sugar intake and dental caries for these children. Since there is a progressive linear increase in dental caries throughout life due to the cumulative nature of disease,35,36 nutrition education and counseling are necessary for these mothers in order to reduce the frequency exposure to cariogenic foods, maintaining the use of fluoride toothpaste, and encouraging uptake of dental services.
To our knowledge, only two studies performed in Saudi Arab12 and India17 were conducted to assess the OHRQoL of children with autism by using the P-CPQ questionnaire. In both studies, scores of P-CPQ were higher than found in our study, which may be related to the socioeconomic characteristics and oral health of the study population. However, only the study performed in India17 evaluated the oral health status and its correlation with QoL. A significant correlation was found between dental caries indices and oral symptoms in children with autism, in contrast to the observed in the present study. Higher scores of functional limitation were also found among children with autism in both studies,12,17 which may be related to self-inflicting habits, eating disorders, and sleep disturbances commonly found in these children.
It was demonstrated that the integrated performance of health professionals and teachers in family dynamics results in improved QoL and in the capacity of caregivers to cope with the symptoms of children with autism.37 Living with a child with autism requires restructuring of family arrangements, which may lead in parental emotional and physical overload and reduction of family QoL.37 Although the effects of autism on family QoL have been well described,10,38,39 we found low scores of FIS and a lack of association between oral health status and family QoL among children and adolescents with autism in the present study, which may related to the positive parental adjustment to the condition of the child. It has been suggested that parents of children with autism who possess indicators of resilience are better able to manage the adversity associated with caring for children.40
Our study has some limitations. First, the convenience sample used for this study may lead in selection bias and lack of generalizability (external validity). Second, parent’s perception of their child’s QoL may not accurately reflect this reality. Third, the lack of a multidimensional analysis to evaluate the influence of a cultural background, comorbidities, and other socio-behavioural risk factors in the OHRQoL in children witha autism. Furthermore, longitudinal studies are needed to evaluate how parents/caregivers perceived OHRQoL over time.
This study suggested that the caregiver literacy has play a role on the OHRQoL in children and adolescents with autism. Further studies with larger sample size are needed to evaluate the influence of other oral health measures on the QoL in this population.
None.
None.
The authors declare that there is no conflict of interest.

©2020 Viana, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.