Journal of
eISSN: 2373-4345


Review Article Volume 12 Issue 2
Oral Medicine and Diagnostic Sciences, King Saud University, Saudi Arabia
Correspondence: Ameera Alabdulwahid, Lecturer, Oral Medicine and Diagnostic Sciences Department, King Saud University, Saudi Arabia, Riyadh
Received: April 21, 2021 | Published: April 27, 2021
Citation: Alabdulwahid A. Cone beam computed tomography: still a blessing for maxillofacial imaging. J Dent Health Oral Disord Ther. 2021;12(2):33-39. DOI: 10.15406/jdhodt.2021.12.00546
In this period of advanced technology, cone beam computed tomography (CBCT) was embraced into the dental settings very rapidly and has gained popularity in the field of oral radiology due to its advantages over conventional two-dimensional (2D) radiography, such as its relatively compact size, low cost, low ionizing radiation exposure when compared to multi detector computed tomography (MDCT). This paper provides an overview of the basic principles of CBCT technology and reviews its current advances on the specific application to the oral and maxillofacial region.
Keywords: Cone‐beam computed tomography, dentistry, diagnostic imaging, clinical applications, principles
CBCT, cone beam computed tomography; 2D, two dimensional; MDCT, multi detector computed tomography; 3D, three dimensional; CCD, charged couple device; MPR, multiplanar reformatting; CMS, complete mouth survey; FOV, field of view; MAR, metal artifact reduction algorithms; TMJ, tempromandibular joint
Dental sciences have been contentiously in high demand to improve the performance of all diagnostic aids. Since the first intraoral radiograph was obtained in 1896, two-dimensional (2D) imaging modalities have been used in dentistry. A While after that, dental radiography has evolved with the introduction of panoramic imaging and tomography. Tomography made it possible to get rid of superimposition by isolating the area of interest. On the other hand, panoramic radiography uses the tomography principle to picture the maxillofacial region in a single image.1 Lowering the radiation dose and decreasing the examination time without affecting the diagnostic quality of the intraoral or panoramic images was always a challenge and a wide area of advancement. However, this 2D imaging modality has a significant limitation as distortion, magnification, and superimposition. Cone beam computed tomography (CBCT) does not have these limitations and can produce three-dimensional (3D) images that can easily guide the diagnosis, treatment options, and follow-up protocol of disorders in the maxillofacial region.
History
CBCT was developed for angiography in 1982 and subsequently applied to dental imaging. It uses a divergent shaped source of x-rays and a 2D area detector supported on a rotating gantry to acquire multiple projection images in one full scan around the area being imaged. In 1994, Feldkamp developed an algorithm that reconstructs the images into a 3D data set.2 CBCT has gained broad acceptance in dentistry. Devoted CBCT scanners for the maxillofacial region were established in the late 1990s by Mozzo et al. in Italy and4 Arai et al.3 in Japan. After that, there has been an outburst of interest in this imaging modality in the field of dentistry by many research groups.
Principle of CBCT
The major innovation of CBCT compared to 2D imaging techniques is that it provides thin sliced images with high quality. The beam exiting the patient is captured on a 2D planar detector, usually a flat panel or an image intensifier/CCD (charged couple device) detector. While the x-ray source moves around the head of the patient, the sensor captures 160 to more than 600 basis images. These images are used to produce a tube-shaped volume, including all, or part of, the skull. In this volume, the densities at all locations (voxels) are calculated from the basis images. Voxels are isotropic and range in size; the smaller the voxel size, the higher image resolution, and relatively higher radiation dose.5
Several cross-sectional views are made in different planes (axial, sagittal, and coronal). From this data set, the operator can extract thick or thin planar or curved reconstructions in any orientation. Additionally, true 3D images of bone or soft tissue surfaces can be generated.6,7
Steps of CBCT image creation:
Advantages of CBCT in dentistry
The essential principle of using CBCT for diagnosis and treatment planning in dentistry is to acquire the maximum benefits from a radiological examination while minimizing the risk from ionizing radiation to the patient. CBCT imaging modality offers different utility but should be used carefully with the relationship between dose and image quality.8 The use of CBCT imaging modality in the dental field provides several benefits for maxillofacial imaging.1
Scanning time in CBCT is comparable to panoramic radiography, which is desirable. It acquires all projection images in a single rotation. Scanning time varies from 5-40 seconds. However, reconstruction time is considerably lengthier. It differs depending on reconstruction algorithm, FOV, resolution, and the number of basis images acquired.
Thanks to the collimation feature of the CBCT, the radiation beam allows restriction of the ionizing radiation to the area of interest. Therefore, an ideal field of view can be chosen for each patient according to the region of interest and disease presentation.1
All produced images (axial, coronal, sagittal, and multiplanar reformation (MPR)) have a high level of spatial resolution precise enough for linear measurement where precision is essential, such as in implant site assessment and orthodontic analysis.1 That is because the originally captured images are with a very small isotropic voxel resolution.
CBCT radiation doses differ significantly according to the machine itself and the imaging protocol. With the continuing development of newer technologies, gradually, lower doses from CBCT imaging are becoming achievable. As such, effective doses produced by a CBCT examination may be comparable to a complete mouth survey (CMS).9
Limitations of CBCT imaging
As the applications of CBCT have increased, CBCT technology still has limitations related to some issues as detector sensitivity, projection geometry, and contrast resolution, which produces images that lack the clearness of conventional CT images.1 The clarity of CBCT images is affected by:
An artifact is any alteration in the image that is irrelevant to the matter being imaged. According to their cause, artifacts can be classified.1
Noise is defined as an unwanted distributed disturbance of a signal that obscures the signal's information content from the observer 10. The primary cone-beam projection acquisitions produce a huge number of basis images. Therefore, a large amount of photons engages in interactions by way of attenuation. Most of which produce scattered radiation. Most of this scattered radiation travels in all directions and is recorded by pixels on the cone-beam area detector. Much of the nonlinear attenuation is recorded and contributes to image degradation or noise due to the use of an area detector.1
The contrast resolution is the ability to distinguish different densities in the image. CBCT units have less soft tissue contrast compared to conventional CT machines. Three factors were found to limit the contrast resolution of CBCT, which include increased image noise, the divergence of the x-ray beam, and numerous inherent flat-panel detector-based artifacts.10,11
Applications
The clinical applications of CBCT in dentistry are enormous. CBCT has offered a valuable oral and maxillofacial radiologist technique to diagnose any bone pathology and developmental anomaly in the maxillofacial region. Although it was discovered years ago, this technique is still a blessing for oral and maxillofacial radiologists. CBCT is preferred for object localization, assessing the relation of supernumerary teeth to surrounding vital structures, impactions, cleft palate, inflammatory bone lesions, developmental anomalies, soft-tissue calcifications, pre-surgical planning, and postoperative evaluation.
Implantology
CBCT imaging is becoming increasingly popular and universally used in dentistry, especially in the assessment for dental implant placement. This is due to its ability to visualize anatomical landmarks and vital structures around the implant site (Figure 1). The wide use of computer-guided surgery, which depends on high-quality CBCT images, is another reason for the increased reputation of the rising use of CBCT in the field.12 It may also include the addition of selected intraoral scans as well as extraoral face scans to create a 3D virtual dental patient.13,14 The concept of a virtual patient is indicating the need for standardization of image data formats to enable smooth incorporation of all available datasets into a craniofacial virtual reality model.
Oral surgery
The ability to illustrate all anatomic structures without superimposition makes CBCT a useful guide in the oral and maxillofacial field. It has an advantage over panoramic imaging in the localization of an impacted third molar to the inferior alveolar canal (Figure 2).15 Likewise, interpreting the buccolingual relationship of a supernumerary tooth to the adjacent structures is much easier with CBCT, which previously required multiple obliquely angled scans as well as occlusal scans (Figure 2).16 The Ankylosis of an impacted tooth is also more reliably pictured on CBCT, and therefore, the treatment difficulties can be predicted and avoided.17
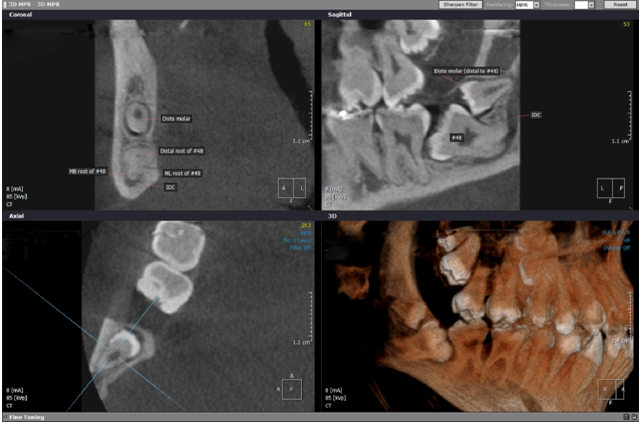
Figure 2 Sectional images showing that roots of impacted #48 are possibly inside the inferior alveolar canal. Distomalar behind tooth #48 is horizontally impacted with its root tip in a close proximity to the inferior alveolar canal and possibly perforating it.
CBCT also provides essential details on the detection, size, and site of cysts and other lesions (Figure 3). The related changes like the existence of bone resorption and its extent, calcifications, cortical expansions can also be visualized more precisely with sectional imaging than conventional 2D images (Figure 4).18 The absence of superimposition makes the adjacent structures better visualized, resulting in improved interpretation. CBCT is, therefore, a valuable imaging modality for pre-surgical planning of such cases, as full visualization and relative closeness to different vital anatomic structures are evaluated.19
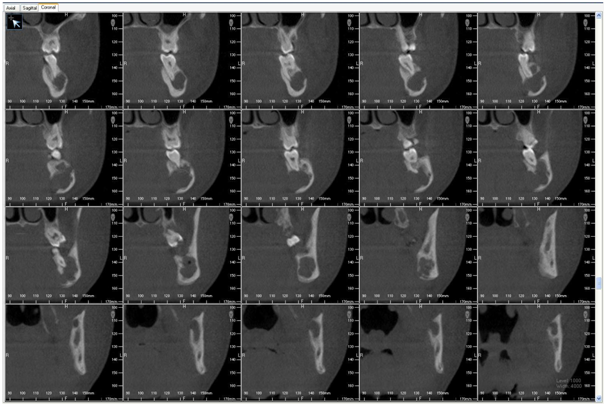
Figure 3 Multiple cross sectional images for a radiolucent lesion showing its effects of surrounding vital structures.
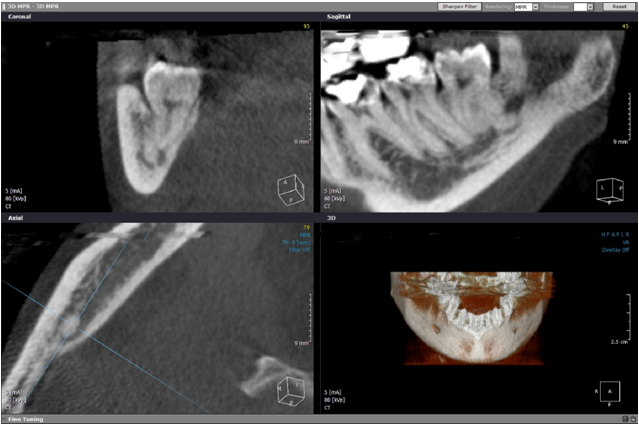
Figure 4 ImplantAxial, coronal and sagittal views showing a round phlebolith inside the inferior alveolar canal apical to tooth #48.
Furthermore, malignancies can be distinguished from benign lesions by cautiously assessing the periphery and boney invasion pattern.20 However, MRI remains a better tool for soft tissue tumors. CBCT also provides a better vision of periosteal bone reaction in chronic inflammatory lesions compared to panoramic and occlusal radiographs.21 CBCT is a reliable alternative imaging modality compared to MDCT for complex jaw fractures.22 It also provides a close vision into the cleft defect in cleft palate patients showing the cleft relation to the maxilla and nasal cavity.23 Accordingly, the amount of graft material needed to reconstruct the alveolus can be assessed.24
Endodontics
Structures superimposition has always been a challenge in endodontics. Multiple radiographs with different angulations are always needed to obtain the required information resulting in increasing chair side time, radiation dose, and patient discomfort, and in many situations, the interpretation still uncertain. Hence, cone beam CT was accepted rapidly by endodontics shortly after its introduction to the dental field.25 CBCT in endodontics requires exceptionally images with high resolution and details to visualize the details of the root canal system and its surrounding periodontium (Figure 5). Since high resolution images come at the expense of increased radiation dose, only small field of view CBCT scans are suggested for the diagnosis and management of endodontic lesions. The small FOV scan decreases the amount of irradiated tissues, and therefore, the effective radiation dose.26 However, The existence of metallic restorations such as amalgam restorations, metal posts, crowns, implants, and even gutta percha can cause a significant amount of radiographic artifact just enough to compromise the detailed anatomy of the root canal and relevant pathosis such as root fractures and root resorption. However, metal artifact reduction algorithms (MAR) are becoming more popular in operating and viewing software to overcome this disadvantage.27
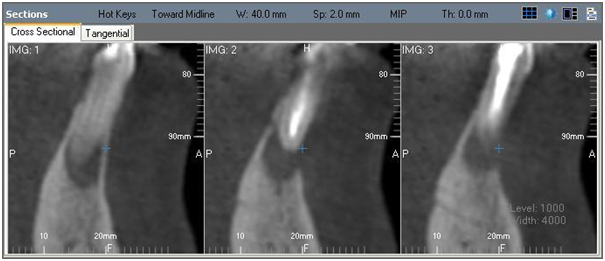
Figure 5 Cross sectional images showing a pathological lesion periapical to an endodontically treated tooth.
Periodontics
It was found that CBCT is very helpful and accurate in the diagnosis of furcation involvement and infra-bony defects. Likewise, it is a reliable tool in the assessment of the outcomes of regenerative therapy and periodontal surgery. It also showed that the CBCT images have significant advantage over conventional 2D in pre-surgical assessment methods about the root morphology and residual attachment of maxillary molars.28
Tempromandibular joints
CBCT can identify early osteoarthritic changes in TMJ as erosions, osteophyte formation, flattening of articular surfaces, irregular cortical outlines, subchondral cyst formation, narrowing of joint space, subchondral sclerosis, and even the location of the condylar head in relation to the temporal complex (Figure 6).29,30 Comparable changes can also be seen in inflammatory disorders but to a more significant extent. CBCT is progressively being used as a standard tool for cases of TMJ ankylosis and trauma. The location of the fracture and the displacement of the fracture, and the relation of the fracture line to the joint capsule can be well demonstrated. On the other hand, when malignancy is suspected on CBCT, CT, MRI, and PET scans are found to have more advanced diagnostic measures to be used.25
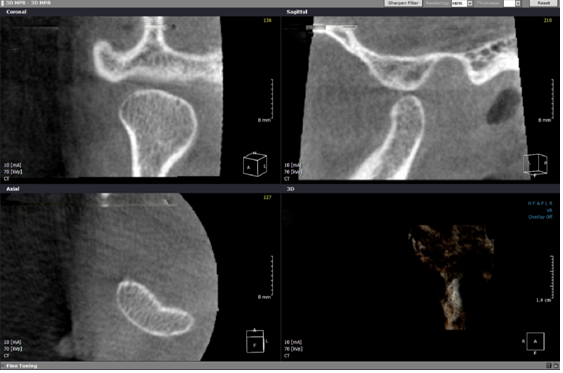
Figure 6 Examination of TMJ showing that the right condyle is anteriorly displaced in the closed mouth position. It reaches the tip of the articular eminence.
Forensic dentistry
Dental age estimation of living or dead individuals is considered a fundamental aspect of forensic science. CBCT can be applied in forensic dentistry for accurate age estimation for every individual, including those who have passed away. Numerous dental age estimation approaches were reported in the literature.31–34 One way to estimate exact age, where a tooth has to be sectioned to recognize morphological changes; as with age, the tooth's internal layers always illustrate the physiological and pathological changes.35 However, such aggressive methods are not required when CBCT is used.36 CBCT serves as a non-invasive technique for dental age assessment. Studies showed that CBCT images of the face could be used for measuring soft tissue thickness in the facial region.37
CBCT approves to overcome several limitations of conventional 2D imaging modalities. The profound use of CBCT technology has made complex craniofacial structures more accessible, which helped for accurate diagnosis and treatment planning in dentistry. CBCT has reduced the use of CT and super specialty setups for 3D imaging of the oral and maxillofacial region in dental clinics 38. However, Potential benefits must outweigh the radiation hazards involved and, the physicians must be defined keeping the above considerations in mind.39
No conflict of interest exists.

©2021 Alabdulwahid. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.