Journal of
eISSN: 2373-4345


Review Article Volume 12 Issue 3
DDS. Pontifical Catholic University of Chile Orthodontist, Instructor in the Department of Children and Dentomaxillary Orthopedics, School of Dentistry, University of Chile
Correspondence: Francisca Durán. DDS Pontifical Catholic University of Chile. Chile
Received: June 09, 2021 | Published: June 30, 2021
Citation: Durán F, Hormazábal F. Ankylosis of the Temporomandibular Joint (TMJ) Update and its treatment. J Dent Health Oral Disord Ther. 2021;12(3):52-57. DOI: 10.15406/jdhodt.2021.12.00549
In dentistry, temporomandibular joint (TMJ) ankylosis is a rare pathology where no consensus of global population data has been found and therefore has presented a challenge for professionals, since there are no treatment sequence protocols standardized. The objective is to carry out a literature review and update of the diagnosis of ankylosis, considering its clinical characteristics, classification, etiology, and epidemiology. Giving special emphasis to the types of treatments used and concluding that GAP interpositional arthroplasty and TMJ reconstruction arthroplasty would be the best options to improve maximum oral opening in a patient with ankylosis, thus allowing him to recover function and aesthetics.
Keywords: temporomandibular disorders, ankylosis, interpositional GAP arthroplasty, reconstruction arthroplasty
Although ankylosis of the temporomandibular joint (TMJ) is an uncommon pathology, so much so that in the current literature there is no consensus of world population data,1 It is important since it is part of what the orthodontist and dentist do, and presents a difficulty for most because there are no standardized treatment sequence protocols.2
It is essential to know the etiology, pathophysiology, and mandibular biomechanics to perform an adequate treatment. This should be done early in the patient's life to prevent alterations in mandibular and maxillary growth and development.
The mandibular condyle is considered an important agent in mandibular development due to its secondary cartilage. As a consequence of the restriction of mandibular movement in this type of patients, craniofacial growth and development may be altered in the vertical, sagittal, and transverse direction of the mandible on the affected side. Atrophying and generating facial asymmetry.3 In addition to deformities of the mandible and maxilla, malocclusions can occur as a consequence.4
Within the classification used for the diagnosis of temporomandibular disorders, we have ankylosis that is classified within chronic mandibular hypomobility. This is a long-lasting, painless limitation of the jaw where pain only occurs when force is used to attempt an opening beyond the existing limitation. Hypomobility disorder can be classified according to its etiology as: ankylosis, muscle contracture and impedance of the coronoid process.5 In this review we will focus exclusively on ankylosis. Which is defined as abnormal immobility of the jaw. It is a disorder that leads to a restriction of the mouth opening with partial reduction of jaw movements or a complete immobility of the jaw.1 This is due to bony or fibrous adhesions between the condyle and the glenoid fossa, disc and/or eminence. It affects the quality of life of the patient by interfering with chewing, speaking and the maintenance of oral and aesthetic hygiene.6
According to a study by Panagiotis et al. The signs and symptoms of temporomandibular disorders (TMD) are more common and severe in women than men, and the severity of these is related to the degree of mouth opening and the number of aural symptoms. (tinnitus, earache, dizziness or vertigo, a sensation of otic fullness, hyperacouse or hypoacouse) Where the absence or presence of mid- level TMD is associated with normal audiograms, while moderate and severe level TMD are related to toned hearing loss medium and low respectively. Other common signs in patients with TMD are bruxism, joint ankylosis, joint pain, and itchy ear.7
When ankylosis is present, translation from the fossa is not possible by limiting the range of motion in all positions (i.e., opening, lateral, protrusion) and, if the ankylosis is unilateral, there will be a deflection of the midline path toward the affected side during opening.
To confirm that ankylosis exists, radiographs of the Temporomandibular Joint (TMJ) can be used. The condyle will not move significantly in protrusion or laterotrusion to the opposite side, so there will be no significant differences in these two plates.5
Computed tomography could also be used, where the characteristics of bone ankylosis can be summarized as follows:
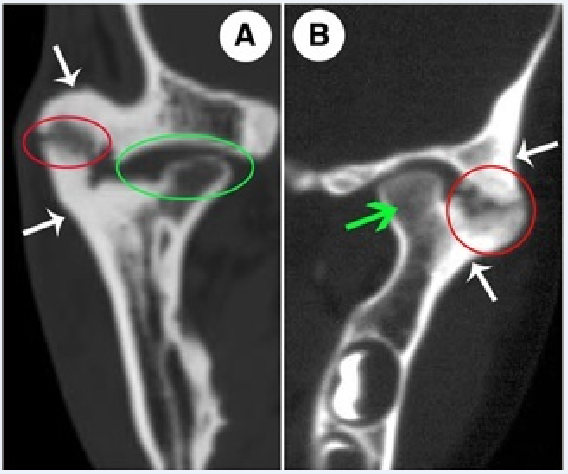
Figure 1 Computed tomographic characteristics of bone ankylosis.
In A, the red circle refers to the area of bone fusion located in the lateral part of the joint, in this area, a radiolucent zone can be observed. The green circle refers to the atrophic condylar head and the rudimentary joint space located in the medial part of the joint. In B, the red circle shows osteosclerosis in the area of bone fusion, and a radiolucent zone can also be seen in this area. The green arrow indicates that the bone mineral density and the morphology of the bone marrow cavity in the non-bone fusion area were normal. In A and B, the white arrows indicate excessive bone formation around the joint. It must be taken into account that, in the radiolucent area, no scattered calcified points can be found.8
Finally, we find Nuclear Magnetic Resonance (MRI), which is the technique of choice for the functional and pathological diagnosis of TMJ, not only because of the anatomical and functional information it provides but also because it is a technique that avoids ionizing radiation. It is also the gold standard for identifying articular disc positions. MRI is capable of establishing the presence of bone, fibrous and fibrous ankylosis, being decisive in the diagnosis of the latter two.1
Now regarding the classification of ankylosis we can summarize it in the following table.
|
Classification |
Description |
|
|
Localization |
Intracapsular |
Pathology involves intracapsular structures. |
|
Extracapsular |
The pathology involves extracapsular structures and may also involve intracapsular structures. |
|
|
Type of tissue involved |
Bone Fibrous |
Involvement of joint osseous tissues. Involvement of fibrous joint tissues. |
|
Fibro osseous |
Combination between involvement of bone tissues and fibrous joints. |
|
|
Extension |
Complete |
Fusion of the structures completely. |
|
Incomplete |
Merging the structures incompletely. |
|
|
Origin |
True |
Origin directly related to the joint. |
|
False |
Origin in pathologies indirectly related to the joint. |
|
|
Severity |
Type I |
Head of the condyle is present but deformed. |
|
Type II |
Fusion occurs between the head of the condyle and the articular surface. |
|
|
Type III |
Formation of a bone block between the branch of the jaw and the zygomatic bone. |
|
|
Type IV |
The anatomy of TMJ is completely altered. |
Table 1 Classification of ankylosis of the temporomandibular joint
Etiology
Regarding the etiology of ankylosis, it should be emphasized that the most frequent is hemarthrosis secondary to a macro-trauma that can constitute a matrix for the development of fibrosis.1,5 These cause a tissue injury that results in secondary inflammation. Another common cause of trauma is from TMJ surgery. Surgical interventions very frequently produce fibrous changes in the capsular ligament, which limit mandibular movement. And third, bone ankylosis could also be associated with a previous infection.5
Clinic history
Patients often report a previous injury or capsulitis, along with an obvious limitation of jaw movement.5
Epidemiology
As a summary, it could be said that ankylosis has as its main etiology a trauma, which occurs at an early adolescent age, more in women, bilaterally. Involving bone tissue, type III ankylosis being the most prevalent. A summary of epidemiological data present in articles of El-Sheik,1 Zhi et al.,1,2,9,10
|
Author |
El-Sheik (1999) |
N=204 |
Zhi et al. (2002) |
N=42 |
Elgazzar et al. (2010) |
N=101 |
Xiaogian (2015) |
N=740 |
Ramat et al. (2018) |
N=36 |
|
Etiology |
Trauma |
98.50% |
Trauma |
83% |
Trauma |
84% |
Trauma |
76.80% |
Trauma |
44.40% |
|
Congenital |
21% |
Infection |
140% |
Surgery |
7% |
Infection |
8.60% |
|||
|
Infection |
0.50% |
Recovery from pneumonia |
3% |
Osteoarthritis |
2% |
Illness |
8% |
|||
|
Hyperplasia |
1% |
Idiopatic |
3.50% |
|||||||
|
Unknown |
5% |
|||||||||
|
Age |
<14 years old |
41% |
<20 years |
59.50% |
<20 years |
60.40% |
10-20 |
52.94% |
13.8average +- 6.6 |
|
|
>14 years |
59% |
>20 years |
40.50% |
>20 years |
39.60% |
|||||
|
Gender |
Men |
48% |
Men |
47.20% |
Men |
38.50% |
Men |
45% |
Men |
58.30% |
|
Women |
52% |
Women |
52.80% |
Women |
61.50% |
Women |
51.32% |
Women |
41.70% |
|
|
Localization |
Unilateral |
45.20% |
Unilateral |
92% |
||||||
|
Bilateral |
54.80% |
Bilateral |
8% |
|||||||
|
Tissue |
Bone Ankylosis |
88.10% |
Bone |
71% |
True |
97.20% |
||||
|
involved |
Fibrous |
6% |
||||||||
|
Fibrous ankylosis |
11.90% |
Fibro |
24% |
False |
2.80% |
|||||
|
Type |
Type I |
11.90% |
||||||||
|
Type II |
23.80% |
|||||||||
|
Type III |
45.20% |
|||||||||
|
Type IV |
19.10% |
|||||||||
Table 2 Summary epidemiological data
Treatments
If the function is insufficient or the limitation is intolerable, surgery is the only definitive treatment available to us. Among the objectives to be achieved with the surgery we have:
Among the surgical techniques, arthroscopic surgery is the least aggressive. Which consists of a minimally invasive procedure where a metal cannula is placed (generally through small incisions in the skin). The cannulas have a camera through which the surgeon can visualize the joint live and perform the indicated procedures such as lavage, disc repair, removal of the bone spur, etc.11
Unfortunately, many ankylosing joints are too immobilized to be released by arthroscopy, and other surgical options need to be considered. When surgical treatment is required, it should be remembered that the levator muscles are likely to be in a state of myostatic contracture, which should be treated once the ankylosis has resolved.5
Arthroplasty is a surgical technique used to treat TMJ ankyloses,2 within them are:
Gap arthroplasty: This type of surgery, which is the oldest, includes the complete resection of the ankylosing block with or without interpositional material, either autogenous or alloplastic. It is used in cases where the ankylosing mass is so small that its resection will not affect the height of the branch. It has the advantage of simplicity and short operation time. On the other hand, it shortens the branch and, therefore, can cause anterior open bite if the ankylosis is bilateral, premature occlusion on the affected side with contralateral and open bite in unilateral cases. The most common complication is recurrence of ankylosis. It has currently been abandoned due to an increased risk of associated failures.
Arthroplasty with joint reconstruction: It is the most used. Excision of the ankylosing block is performed, coronoidectomy on the affected side and ipsilateral coronoidectomy if necessary, reconstruction of the glenoid fossa, reconstruction of the disc with superficial temporal fascia or with a muscle flap if the original disc is not available, the condyle unit is reconstructed. branch according to surgeon's choice with costochondral bone, coronoid process, osteogenic distraction (DO), or total alloplastic replacement. The dead space is filled with a buccal fat graft. This surgical procedure is a good option for patients with ankylosis because it provides restoration of normal joint function both anatomically and mechanically. It also avoids the disadvantage of mandibular ramus shortening, consequent malocclusions, and significantly reduces the incidence of reankylosis.
The preferred method of treatment is primarily interpositional gap arthroplasty (IGA) or reconstruction arthroplasty (RA) depending on age and associated facial deformity.6
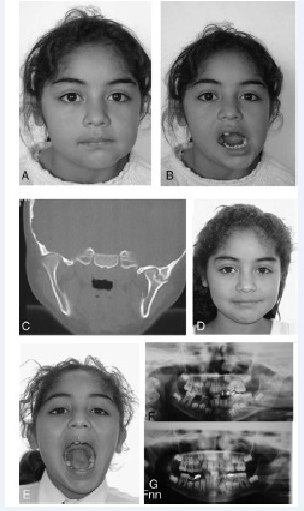
Figure 2 (A) Front view before surgery. (B) Maximum opening of the mouth before surgery. (C) Computed tomography of external TMJ ankylosis. (D) Front view after GAP arthroplasty (3 years post-surgery). (E) Maximum mouth opening after GAP arthroplasty (3 years post-surgery). (F) Panoramic radiograph of left external TMJ ankylosis before surgery. (G) Panoramic radiograph 3 years after GAP arthroplasty.
The greatest difficulty for most clinicians is determining the proper sequence of these procedures because a standardized treatment protocol has not been established.2 That is why we will make a summary table of surgical data present in articles by Xiaohan et al., Mittal et al., Al- Moraissi,12 Xu,13 Elgazzar et al. to allow a better comparison of how they have decided to approach this disease (Table III).
|
Author |
Xiaohan, L |
Mittal, N |
Al-Moraissi, EA |
Xu, F |
Elgazzar, RF |
|
N= |
17 studies with 740 participants |
26 studies 1197 |
16 studies |
18 patients |
101 patients |
|
Technique used |
1. Gap arthroplasty (GA) |
1. Gap arthroplasty (GA) |
1. Gap arthroplasty (GA) |
1. JR using autogenous grafting of coronoid process. (AGCP)for condyle reconstruction |
1. CCG 18.4% |
|
Technique with better outcome |
IGA |
IGA with autogenous or alloplastic material for joint reconstruction. |
IGA > MIO than GA IGA > MIO than CCG autogenous CCG> MIO que JRAG JRAGA > CCG in decreasing pain |
LA |
Arthroplasty with condyle/branch unit reconstruction with autogenous CCG. |
|
What was considered successful |
Increased maximum incisal opening (MIO) greater in IGA |
Maximum mouth opening augmentation (MMO) |
MIO and pain |
Recurrence rate, change in facial pattern and improvement in MIO |
Oral opening of 5.3mm- 32.9mm after 1 year |
|
Follow-up period |
0.5 -11 years |
≥12 months |
0.5-15 years |
12-24 months |
14-96 months |
|
Complications |
GA: open bite, premature occlusion affected side, suboptimal range of motion IGA: graft fracture, infection, overgrowth, donor site morbidity, foreign body reaction and dystrophic bone formation |
IGA: The use of the temporal muscle as interpositional tissue can limit the oral opening leaving scarring in the muscle and thus shortening by muscle damage. |
Re-ankylosis 20% Temporal branch paralysis of the facial nerve 30% |
Re-ankylosis 4.6% Infection 4.6% |
|
|
Recurrence |
2.56% |
IGA y JR<GA |
Decreases by 21.5% IGA v/s GA Decreases by 38% IGA v/s CCG |
20% |
5% |
Table 3 Summary surgical data
It could be concluded that, within the treatments analyzed, interpositional arthroplasty of GAP and arthroplasty with TMJ reconstruction would be the best options to improve maximum oral opening in patients with ankylosis. Being the replacement of the joint with alloplastic materials the one with the best result in patients with pain. However, no consensus has been reached within the publications, and the biggest problem is the recurrence of ankylosis.
The arthroplasty of spaces without interpositional material has been gradually abandoned by many surgeons due to the associated high risk of recurrence.1 Interjecting13 a temporal myofascial flap (TMF) is the most widely used material, with benefits including easy removal and less chance of resorption. However, this flap also presents problems such as donor site morbidity, chronic headache, and trismus. Trismus caused by scarring of the temporal muscle contracture can be prevented by ipsilateral coronoidectomy.
Early treatment of TMJ ankylosis, reconstruction of ramus height with osteogenic distraction or arthroplasty with bone graft combined with interposition followed by vigorous physical therapy, has been seen as a successful treatment for the management of TMJ ankylosis.
None.
None.

©2021 Durán, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.