Journal of
eISSN: 2373-4345


Case Report Volume 9 Issue 2
1Faculty of Dentistry, University of Aleppo, Syria
2Faculty of Dentistry, Reims University, France
Correspondence: Sarraj Faysal, Department of Odontology, Reims Champagne-Ardennes University, 2 rue du General Koenig, 51100 Reims, France, Tel 33788543508, Fax 33326913480
Received: January 11, 2018 | Published: March 13, 2018
Citation: Faysal S, Ayman S, Loïc P, et al. A case report of Keratoacanthoma (KA) of the alveolar ridge of the maxilla. J Dent Health Oral Disord Ther. 2018;9(2):130-133. DOI: 10.15406/jdhodt.2018.09.00344
Keratoacanthoma (KA) is a case related to skin squamous cell carcinoma but it is a self-limited case. It is usually seen in areas of exposed skin and rarely to be seen intra-orally. Here we present a case of oral keratoacanthoma on the alveolar ridge of the maxillae, which may arise as a result of trauma or unknown stimulus. The case was treated with liquid nitrogen for six sessions and completely resolving of the lesion was recorded without a scar formation. Cryosurgery for exophytic lesions either benign or malignant (well differentiated) isworthy to be recommended than traditional surgery.
Keywords: Keratoacanthoma (KA), squamous cell carcinoma, intraoral, cryosurgery, liquid nitrogen
KA, Keratoacanthoma; SCC, squamous cell carcinoma
Keratoacanthoma (self-healing carcinoma) is a relatively common skin lesion and sometimes lips may be affected, but intra-orally structures are rarely affected.1 Habel et al.2 in a review of intraoral keratoacanthoma, described 11 cases of intraoral keratoacanthoma and the patient ages ranged from 12 to 80 years with strong predilection for males. They also denoted the difficulty in distinguishing the central part of these lesions from SCCs microscopically. They considered that the most distinctive microscopic features are the elevation of the abrupt change to hyperplasia. Moreover, Chen et al.3 had discovered a case of keratoacanthoma of the tongue, meanwhile Ramos et al.4 revealed a case of keratoacanthoma of the inferior lip. Keratoacanthoma may be present as solitary or multiple lesions (Table 1).5 The etiological factors for this lesion are sunlight exposure, viruses and possibly other suspected factors such as chemical carcinogens, trauma, and disordered cellular immunity.6 The lesion usually begins as a small red macule that soon becomes a firm papule. Rapid enlargement of the papule occurs over approximately 4-8 weeks, resulting ultimately in a hemispheric, firm, elevated, asymptomatic nodule. When fully developed, a keratoacanthoma contains a core of keratin surrounded by a concentric collar of raised skin or mucosa and a peripheral rim of erythema at the lesion’s base may be parallel the raised margin (the eruptive variant). This variant of the lesion may be distinguished as it is often lacking the central keratin-filled crater which may resemble a neoplastic ulcer clinically. Spontaneous regression over 4-6 months leaving a small scar, but unusual confidence is required to leave such a lesion untreated.1‒7
Ferguson-Smith |
1 to several nodules in succession, benign in adolescence |
Grzybowski |
1-5 mm follicular papules, eruptive and progressive, in adulthood, heal without scarring |
Witten-Zak |
1-5 mm follicular papules and larger nodules; benign in childhood |
Muir-Torre |
Association of ≥ 1 sebaceous neoplasm or ≥ 1 keratoacanthomas with internal malignancy |
Incontinentia pigment |
Subungual tumours |
Xeroderma pigmentosum |
Initial Blaschkoid blisters to verrucous lesions to hyperpigmentation to eventful hypo pigmentation with early development of cutaneous cancers |
Table 1 Disorders with multiple keratoacanthoma
A 59-year old male patient reported to the Out Patient Department of Oral Medicine of Faculty of Dentistry, Aleppo University, Syria, with ten days pain complaint of anterior maxilla and a desire for compensation the missing teeth. He also denoted that he was wearing a partial denture but it has broken since two months ago. His medical history was otherwise unremarkable and he was a smoker. He had smoked 20–35 cigarettes a day for more than 40-years. Clinical examination revealed a rounded ulcer circumscribed by a raised-rolled margin approximately 7-10 mm in diameter on the alveolar ridge of the maxilla at the site of left upper lateral incisor (Figure 1). The ulcer had normal mucosa color with a grayish center. There was no alteration in the face or the neck and no lymph nodes enlargement was recorded. The patient did not mention any other lesion throughout his body. Intraoral examination was also non-contributory but the patient had poor oral hygiene.
Kenalog and nystatine were prescribed to the patient for two weeks but he revealed no improvement. An incisional biopsy under local anesthesia, which included the margin of normal mucosa, was performed. Histological examination of the lesion revealed the presence of hyperplastic epithelium with irregular tongue like projections extending into the underlying connective tissue (pseudoepitheliomatous formation). The epithelium composed of well-differentiated spinous cells with minimal nuclear pleomorphism, few mitotic figures without atypical, intra-epithelial dyskeratosis and hyperkeratosis (Figure 2). Epithelial islands were intermingled with the underlying connective tissue The underlying connective tissue was fibrous with marked infiltration with chronic inflammatory cells infiltration (Figure 3). Margins of the lesion expressed a classical change of normal stratified epithelium to the abrupt change of the lesional tissue without any evidence of malignancy in the marginal epithelium (Figure 4). These findings suggested by two pathologists (oral and general one) a case of keratoacanthoma. The patient was treated with liquid nitrogen for six sessions with one-week rest between each session (after explaining to the patient treatment plane, methods, possibly side effects and getting a written approval from him to the treatment plane in accordance with the ethical standards of the Aleppo University on human experimentation and with the Helsinki Declaration of 1975, as revised in 2000). Each session depended on liquid nitrogen application for three cycles (each cycle consists of freezing for 90 sec with snow-cap formation then thawing for 120 sec) (Figure 5) (Figure 6). No local anesthesia or even an anesthetic spry were used since no compliment of the patient was recorded. After 2 months, the lesion was completely resolved with no scar formation (Figure 7).
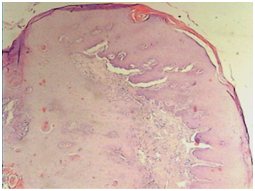
Figure 2 The histological features observed in the biopsy. A Low-power view of the tissue section presenting epithelial proliferation in the upward and downward direction (H&E stain, 40X).
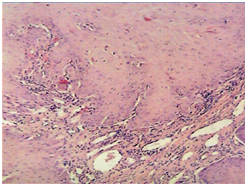
Figure 3 High power magnification of the tissue section revealing the epithelial projection invading the underlying connective tissue. Acanthosis and moderate inflammatory cells infiltration were noticed (H&E Stain, 100X).
Keratoacanthoma is a squamoproliferative lesion of unknown cause that occurs chiefly on sun-exposed skin and less commonly at the mucocuataneous junction. Very rarely has this lesion been reported to arise on mucous membranes.6 Different names have been given to keratoacanthoma such as molluscum sebaceum, molluscum pseudocarcinomatosum, self-healing primary squamous cell carcinoma, tumour-likekeratosis and idiopathic cutaneous pseudoepitheliomatous hyperplasia.7 Chauhan et al.8 expressed in his review the possible cause factors for kearatoacanthoma. They concluded that actinic factor, chemical carcinogens (coal and mechanic oil), trauma, genetics and viruses were contributory factors for this lesion. Other postulated etiologic factors include chemotherapy, circulating carcinogenic factors and immunologic factors.9 Keratoacanthoma has been reported in patients ranging from 14 to 86 years, the average age being 56 years for both males and females. Eighty percent on the patients were over 40 years of age, and the maximum incidence was between 50 to 70 years-old, with male to female ratio of 2:19. Clinically, the lesion appears as painless carter-like and the mature lesion is usually bud- or dome-shaped and is brownish or slightly reddish.10 The eruptive variant of the lesion may be distinguished as it is often lacking the central keratin-filled crater.7 Keratoacanthoma lesions are somewhat difficult to differentiate from SCC or vice versa. Helpful criteria for the diagnosis of keratoacanthoma included epithelial lip, sharp out line between tumour and stroma and ulceration. Criteria more commonly seen in SCCs included numerous mitosis and marked cellular pleomorphism11. Ko5 revealed in his review many markers for epidermal differentiation and intercellular adhesion to differentiate between keratoacanthoma and SCCs. He revealed form one study that filaggrin staining is much more present in keratoacanthoma than SCCs, whole another study did not confirmed that. He also revealed from different studies that fully developed keratoacanthoma expressed VCAM, ICAM, Syndecan-1 and E-cadherin immunoreaction, whereas SCCs expressed focal expression for these proteins. On the contrary, SCCs revealed increased expression of antiapoptotic markers (bcl-2) when compared with well-developed keratoacanthoma. Andrews12 revealed that cryosurgery is a highly effective treatment for a broad range of benign skin problems. Cryosurgery is best suited for use in patients with light skin and for treatment of lesions in most non–hair-bearing areas of the body. Spray methods include the timed spot freeze technique, the rotary or spiral pattern, and the paintbrush method. Benign skin lesions that are suitable for freezing include actinic keratosis, solar lentigo, seborrheic keratosis, viral wart, molluscum contagiosum, and dermatofibroma. Cryosurgery requires little time and fits easily into the physician’s office schedule. Advantages of this treatment include a short preparation time, low risk of infection, and minimal wound care. In addition, cryosurgery requires no expensive supplies or injectable anesthesia, and the patient does not have to return for suture removal. Potential side effects include bleeding, blister formation, headache, hair loss, and hypopigmentation, but rarely scarring. Skin lesions often can be treated in a single session, although some require several treatments.
Cryotherapy, through using liquid nitrogen, depends on three steps; heat transfer, cell injury (damage of the cell wall) and inflammation (as a response to local cell destruction).13 Cryotherapy was broadly used in different treatments as a treating method for superficial lesions and as an adjuvant treatment to surgical procedures for some lesions. Dabak et al.14 had used liquid nitrogen in treating benign aggressive and low-grade malignant bone tumors after curettage of the lesion. They detected no tumor recurrence or complications, including soft-tissue injury, infection, and late fracture after liquid nitrogen application. Giuffrida et al.15 had found that Single freeze-thaw cryosurgery may provide a histologic cure of well-defined, nodulo-ulcerative BCCs of the trunk and extremities less than or equal to 1 cm. Suwalski et al.16 introduced the liquid nitrogen to treat atrial fibrillation as a less invasive, safer and technically easier procedures. Fraunfelder17 stated that liquid nitrogen cryotherapy on the surface of the eye has proven effective in treating malignant and premalignant ocular surface tumors. In malignancies, a rapid freeze and slow thaw is the most tumoricidal, and this is effectively accomplished with liquid nitrogen, as it has the lowest boiling point and can provide the quickest freeze of the cryotherapy agents in use. These findings were in agree with the result of this study since the lesion was totally resolved with very little scar formation and the clinical features (pain and ulcer) were absent after six cession of liquid nitrogen usage. Moreover, Bruggink et al.10 have proved through their randomized clinical trial for treatment of skin warts that liquid nitrogen was more effective than salicylic acid treatment for the common warts. Different aspects of dentistry had employed the using of liquid nitrogen. Zhou et al.18 had applied it through cotton rolls to treat bony walls after enucleation the odontogenic keratocyst which lowered the necessity to ostectomy. Abdullah19 in his review for surgical treatment of keratocystic odontogenic tumour, he cleared that the use of liquid nitrogen to treat the bone cavity after surgical enucleation of KCOT would be of a great help in decreasing recurrence rate. He add that the advantages of liquid nitrogen over alternative methods of devitalizing the tissue beyond the visible lesion of the margin are that the bone matrix is left in place to act as a clean scaffold for new bone formation, a bone graft can be placed immediately to accelerate healing and minimize the risk of a pathologic fracture, and decrease of bleeding and scarring. Moraes et al.20 had presented the treatment of lower lip mucoceles in children via liquid nitrogen cryosurgery performed without local anesthesia. Using of liquid nitrogen in treating keratoacanthoma was approved in this research. In a previous trail, we used the same procedure for liquid nitrogen application in treating squamous cell papilloma at the commissure of the mouth21 through applying 3 cycles of liquid nitrogen but the period of application was shorter (60 sec for freezing and 120 sec for thawing). The lesion was completely resolved after three sessions without recurrence during four months of patient’s control. The increased in freezing time in this work was due to the up-ward & down-ward growth of the keratoacanthoma, while SCP revealed up-ward growth pattern only.
Keratoacanthoma may be included in the differential diagnosis where an ulcerated lesion with circumscribed, rolled margins and keratinized bed are confirmed histopathologically regardless of the position of the lesion. Moreover, some authors consider the lesion to be benign, whereas others classify it as a subtype of SCC. In addition, keratoacanthoma is generally treated rather than observed for spontaneous regression.
None.
There is no conflict of interest.
The patient consented to use his clinical information and photos for publication and education purposes.

©2018 Faysal, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.