Journal of
eISSN: 2373-4345


Research Article Volume 6 Issue 5
Department of Removable Prosthodontics, Alexandria University, Egypt
Correspondence: Mervat Elsayed Abd-Ellah, Department of Removable Prosthodontics, Alexandria University, Egypt, Tel 201000000000
Received: February 03, 2016 | Published: March 10, 2017
Citation: Abdelhamid AM, Abbas FS, Ellah MEA. Integrated versus non integrated reciprocation of attachment used for mandibular distal extension bases. J Dent Health Oral Disord Ther. 2017;6(5):135-142. DOI: 10.15406/jdhodt.2017.06.00213
Statement of the problem: Designing of removable partial denture (RPD) present numerous biomechanical problems regarding the principles of reciprocation. However, extra coronal resilient attachment does not always supply suitable support and bracing because of their resilient nature. Therefore, they require specially designed bracing arms on surveyed crowns that require deeper tooth preparation lingually to prevent over contouring of the abutment teeth crown. Purpose of the study: The aim of this study was to evaluate clinically and radiographically the extra coronal semi precision attachments incorporated in metallic (RPD) with two different designs of reciprocation; parallel interlock and integrated interlock.
Materials and methods: Six patients were selected for this study having maxillary completely dentulous arch against mandibular bilateral distal extension ridges posterior to second premolar. All attachment clinical and laboratory steps were performed for both designs using Split-mouth experimental method. Abutment teeth were examined clinically using; Plaque Index, Gingival Index, Periodontal Probing Pocket Depth and Clinical Attachment Level and radiographically immediately at time of RPD insertion then 3, 6 months of denture use.
Results: Clinical results showed statistically significant increase in all parameters around parallel interlock design than integrated interlock design after six months. There was statistically significant increase in total mesial and distal bone loss associated with parallel interlock design in relation to integrated interlock design at six months follow up period. Conclusions: Absence of lingual bracing arm with integrated interlock design decreased the opportunity for plaque accumulation and enhanced the oral health of the premolar abutment teeth.
Clinical implications: This study recommends the use of integrated interlock design for reciprocation as a common design of extracoronal semiprecision attachment for distal extension RPD for its favorable intraoral health parameters.
Keywords: Integrated interlock, non integrated interlock, extracoronal semiprecision attachment, reciprocation, bracing arm, distal extension bases
RPD, removable partial denture; Design A, integrated interlock; Design B, parallel interlock
Rehabilitation of partially edentulous cases in absence of distal abutments is notably troublesome for both the prosthodontist and the patient. Various methods and materials have been used for the treatment of such patients having distal extension ridges.1 Rehabilitation of Kennedy's Classes I and II partially edentulous patients can be challenging because a natural tooth retained fixed prostheses cannot be fabricated. In those cases, acrylic or cast partial denture have been largely preferred, but with barely satisfactory esthetical results. Implant-retained restoration is an option but this is sometimes not possible due to insufficient amount of bone or economic reasons. An alternative reconstructive option that does not involve complex procedures for the patient is combination prosthesis with fixed and removable partial denture connected with attachments. An attachment retained RPD has long been considered the highest form of partial denture therapy.2,3 Numerous studies had conducted to test effect of distal extension partial dentures on both abutments and residual alveolar ridge.1–5 Removable partial denture should be designed and constructed to preserve the remaining oral structures as well as to restore function.4 The design and construction of removable partial denture present numerous biomechanical problems regarding the principles of support, bracing and retention. In distal extension removable partial denture both the teeth and the underlying supporting structures are used to accomplish these principles and they should be protected from damage by the restoration.6 In clasp retained removable partial denture every effort should be used to apply the force close to the bony support of the tooth and near the long axis of the abutment teeth. Each retentive clasp terminal must be opposed by a reciprocal clasp arm or another element of the partial denture capable of resisting horizontal forces exerted on the tooth by the retentive arm.7 It was stated that a clasp may cause rotation of the teeth, since it is not always possible to apply a reciprocal arm at the same level as retentive part of the clasp. There is no possibility of it occurring if an intracoronal attachment has been used.1 Semiprecision or precision attachments are often used to avoid unaesthetic retentive clasps, however, attachments can contribute to stresses concentration with Kennedy class I or II removable partial denture. Methods were used to control the stresses including splinted abutment teeth, stability of denture base and rigid design of the prostheses, broad denture coverage and occlusal harmony, loading techniques and shimming.8 Thus, this work was carried out to study the effect of two different designs of reciprocation in conjunction with extracoronal semi-precision attachment on preservation of alveolar bone and clinical health of abutment teeth with distal extension bases.
This study was performed on six partially edentulous patients having mandibular class I (Kennedy classification). Patients were selected from the diagnostic clinic of Prosthodontic Department, Faculty of Dentistry, and Alexandria University.
Patient’s selection criteria
All patients were selected to be:
The distance between the gingival margin of the remaining natural teeth lingually and the functional depth of the floor of the mouth of at least 8 mm with no soft tissue undercuts. The two different designs of attachments were used for each patient, one design at each side (split mouth technique). The attachment designs used were identified as Design (A) and Design (B) where:
Method
Pre-prosthetic procedures
For every patient the following steps were performed: Diagnostic panoramic and periapical radiographs for both the first and second premolars at both sides. Periodontal therapy in terms of thorough oral scaling, pocket eradication and hygiene procedures. An accurate reproduction of the maxillary and mandibular arches was performed using irreversible hydrocolloid impression material** (**Cavex CA37, Holland BV, Haalem, The Netherlands) in a modified stock tray to obtain diagnostic casts. Diagnostic maxillary casts were mounted on Whip Mix articulator* (*Whip Mix Articulator 8500 Series, Louisville, KY 40217-0183, USA) using ear-piece face-bow transfer** (**Whip Mix Quickmount Face-Bow, Louisville, KY 40217-0183, USA) while diagnostic mandibular casts were mounted using centric relation. A great deal of information was gathered from articulated diagnostic casts that enabled us to achieve the proposed treatment plan. Diagnostic waxing up (Figure 3) and occlusal analysis were performed then the suitable related adjustments were done intra-orally to have harmonious occlusal balance. Each mandibular diagnostic cast was surveyed to assess the needed intraoral modifications to prepare the abutment teeth at both sides. Distal extension saddle denture was designed as follows: bilateral distal extension bases with two different designs of extracoronal semi-precision attachments (one at each side) using two premolar abutment teeth at each side with lingual bar major connector.
Prosthetic procedures
For each patient splinted crown were prepared as follows: Full Crown preparation for first and second premolars at both sides was performed.9 To insure an accurate reproduction of the entire preparation, the gingival finish line was temporarily exposed by enlarging the gingival sulcus using a retraction cord on a dry field for two to three minutes to prepare for the final impression. Polyvinyl Siloxane impression for the prepared abutments was made using a putty rubber base impression material with secondary wash of light body rubber base impression material*** (***Silicone Impression Material, Zhermack, 45021 Badia Polestine (Rovigo), Italy) then poured in improved dental stone. Temporary crowns were cemented to the prepared teeth to preserve them. On the resulting master cast, the wax pattern of the splinted crowns of the first and second premolar was constructed as one single unit with the adaptation of the plastic castable patrix of the attachments; one side received extracoronal semi-precision attachment with integrated interlock (Design A), while parallel interlock (Design B) was done at the other side. After waxing-up the copings of the crowns, the male part of each attachment was aligned to its respective crown using a Milling Machine BF-2**** (**** Bredent company, GmbH &CoKG.Weissenhorner Str.2.89250 Senden, Germany) with paralleling mandrel. The patrix (male part) should be mounted parallel to the path of insertion, over the center of the residual ridge and as close as possible to the preparation. For design B, a step was prepared in the lingual surface of the waxed-up crown on the second premolar to accommodate a conventional bracing arm (ledge) and an occlusal rest seat (mini-rest) was created to receive a metallic extension from the lingual bracing arm. The wax pattern of the crowns is sprued, invested and cast. Removal of the temporary crowns and Try-in of the metal copings of the crowns with extracoronal semi-precision attachment was done in the patient mouth. Shade selection of the porcelain color that match the patient’s remaining teeth color. Removal of the temporary crowns then Try-in of the porcelain crowns was done (Figure 4A, 4B & 5A, 5B). The porcelain crowns were placed on the abutment teeth and were checked for marginal adaptation, proximal contact, and occlusal refinement, then were cemented to the prepared teeth using temporary cement* to insure absence of any movement of the crowns while making the final mandibular impression. With the splinted crowns in the patient’s mouth, an overall regular body pick up impression* (*Cavex Temporary Cement BV, 852 RW Haarlem (Holland)) was made in a border moulded acrylic resin custom-made tray that was spaced 2-3 mm over the abutments and the remaining teeth but closely adapted on the edentulous ridge. The dies, upon which the crown wax patterns were constructed, were then placed inside the picked up crowns. This impression technique is termed “the two stage elastom eric impression technique” that was recommended for distal extension RPD that are retained by either rigid or resilient attachments.10 The mandibular master cast, including the porcelain crowns with extracoronal semi-precision attachment (Figure 6), was surveyed and removable partial denture was designed (Figure 7), and cast with chromium cobalt alloy (Figure 8). The yellow plastic female component (matrix) was placed in the metal framework using matrix inserting instrument (Figure 9). (*Cavex Temporary Cement BV, 852 RW Haarlem (Holland)) *The metal framework of their movable partial denture was tried in. The maxillary cast was mounted on Whip Mix articulator using ear-piece face bow transfer. Mandibular record block was constructed and jaw relation was registered while the porcelain crowns in place then mounting the mandibular cast are done. Acrylic semi-anatomical teeth** (**Ketac Cem 56900, 3M ESPE, Germany) were selected, arranged, and tried in patient’s mouth. All the crowns were ceme*(*Bredent company, GmbH &CoKG.Weissenhorner Str.2.89250 Senden, Germany) nted at the same time with the insertion of the metallic removable partial denture using Glass Ionomer Cement*** (***Silicone Impression Material, Zhermack, 45021 Badia Polestine (Rovigo), Italy). During the cementation, the partial denture was seated on the crowns to decrease the incidence of occlusal errors introduced by the cement thickness. Patients were dismissed and the partial denture was inserted 24 hours later, which allowed the cement to gain its maximum strength. Maintaining services for denture were carried out at regular intervals (4 weeks). The patients were instructed to:

Figure 4A&4B The porcelain crowns with Design a extra coronal semi precision attachments; A: Buccal view; B: Lingual view.

Figure 5A&5B The porcelain crowns with Design b extra coronal semi precision attachments; A: Buccal view, B: Lingual view.
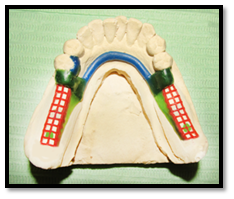
Figure 6 The mandibular master cast including the porcelain crowns with extra coronal semi-precision attachment.
Methods of evaluation
Clinical evaluation
The following clinical parameters of periodontal tissues of the abutment teeth were evaluated at time of denture insertion then 3, 6 months of denture use:
Plaque Index (PI): The plaque index used in the study was according to Silness & Loe11 with scoring from (0-3) to assess the thickness of plaque at the gingival one third of the abutment teeth by examining them at four surfaces; buccal, lingual, mesial and distal.
Gingival Index (GI): Gingival index (GI) was assessed according to Loe & Silness.12 The examination is done on mandibular premolars at both the right and left sidesat four surfaces; buccal, lingual, mesial and distal by blunt probe. Each of the selected surfaces of the tooth was allocated a score from 0 to 3.
Periodontal Probing Pocket Depth (PPD): Pocket depth was measured on all axial surfaces of abutment teeth according to the standard procedures described by Glavind & Loe.13 The measurements were carried out manually with a Michigan "O" periodontal probe with Williams's calibrations. Pocket depth refers to the distance from the gingival margin to the bottom of the clinical pocket in millimeters. Pocket depths of 1 mm or less were recorded as "1 mm measurements exceeding 1 mm, but less than 2 mm, was recorded as "2 mm", etc. Measurements were made at six specific sites on each treated abutment tooth: mesiobuccal, mid-buccal, distobuccal, mesio-lingual, mid-lingual and distolingual. Efforts were made to insert the probe parallel to the long axis of the roots. Light force was used during the introduction of the probe to the bottom of the pocket. The PPD score for a tooth was obtained by totalling the six pocket depth scores per tooth then the sum of t scores was divided by six.
Clinical Attachment Level (CAL):13 Clinical attachment level refers to the distance from the cervical margin of the crown to the apical extent of the probe penetration. It was measured by a periodontal probe on the six sites of abutment teeth surfaces; mesiobuccal, mid-buccal, distobuccal, mesio-lingual, mid-lingual and distolingual. Same way of measurements as pocket depth, 1mm or less was recorded as 1mm, measurements exceeding 1mm but less than 2mm were recorded as 2mm, etc…The attachment loss for each tooth was determined. It is important to note that the measurements were taken from the crown margins as a reference point rather than Cement-Enamel Junction (CEJ), due to the fact that the abutment teeth were covered by the permanently cemented crowns, concealing the CEJ. The CAL score for a tooth was obtained by totalling the six Clinical Attachment Level scores per tooth then the sum of t scores was divided by six.
Radiographic evaluation14
Standardized digital periapical film (Figure 10) was done at time of denture insertion then 3, 6 months of denture use to evaluate marginal bone height around the abutment teeth using Suni Ray digital charge-coupled device (CCD) for Digital Radiography* (*Whip Mix Articulator 8500 Series, Louisville, KY 40217-0183, USA) and XCP device for standardization. The distance from the cervical margin of the crown and the crest of the alveolar bone was measured mesially and distally using the digital ruler. The observer was allowed to use different image processing facilities provided by the software of the system if required to enhance the image quality* * (*Suni Medical Imaging Inc. San Jose, CA).
The data collected from both the clinical and radiographic surveys were tabulated and statistically analyzed within and in between the two designs of attachments. The collected data were fed to the computer and analyzed using IBM SPSS software package version 20.0. Quantitative data were described using range (minimum and maximum), mean, standard deviation and median. The distributions of quantitative variables were tested for normality using Kolmogorov-Smirnov test, Shapiro-Wilk test and D'Agstino test, also Histogram and QQ plot were used for vision test. If it reveals normal data distribution, parametric tests was applied. If the data were abnormally distributed, non-parametric tests were used. For abnormally distributed data, comparison between two independent populations were done using Mann Whitney test. To compare between the different periods Friedman test was applied and Wilcoxon signed ranks test. Significance test results are quoted as two-tailed probabilities. Significance of the obtained results was judged at the 5% level.
Results of clinical evaluation
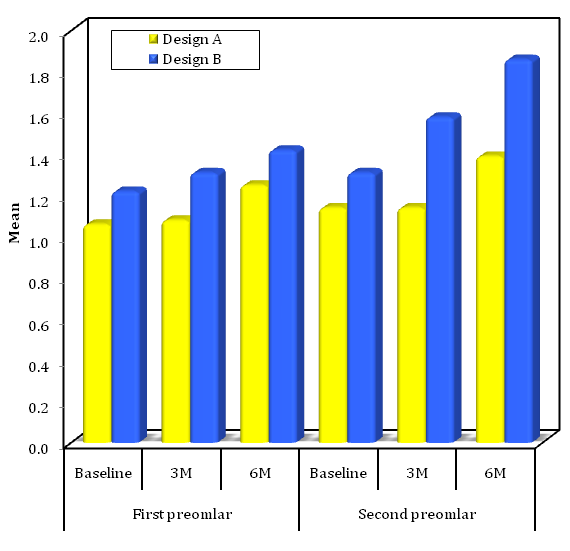
Clinical results showed that after six months, there was statistically significant increase in all parameters around parallel interlock (Design B) than integrated interlock (Design A) (Graphs 1–4).
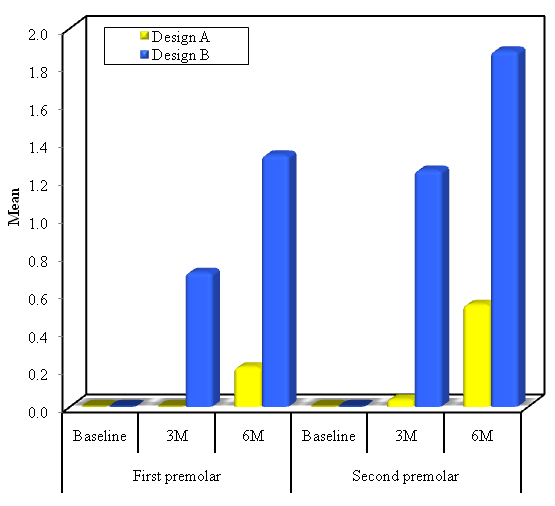
Graph 1 Comparison between studied periods regarding plaque index for both premolars at both designs at each period of follow-up.
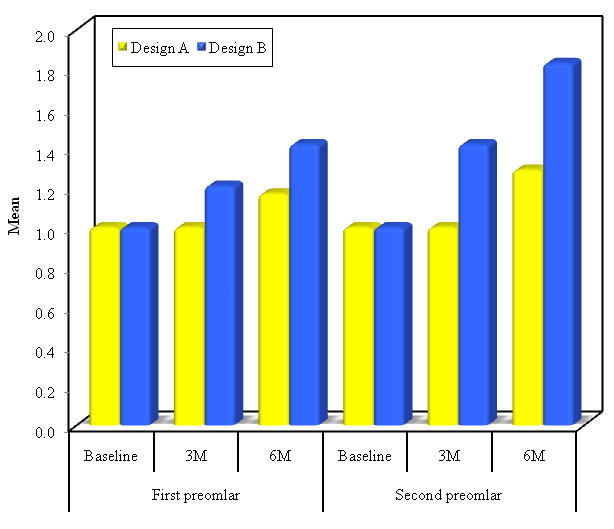
Graph 2 Comparison between studied periods regarding Gingival Index for both premolars at both designs at each period of follow-up.
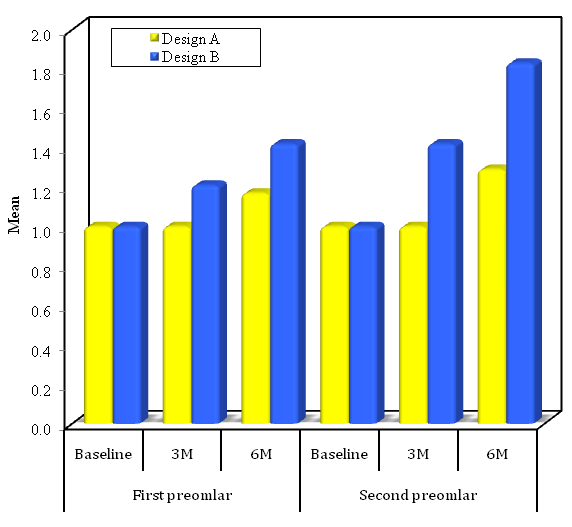
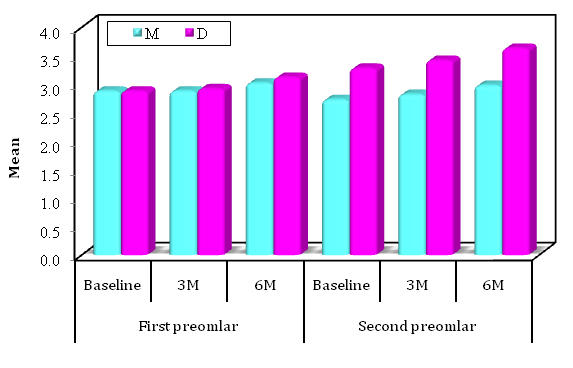
Graph 3 Comparison between studied periods regarding periodontal probing depth for both premolars at both designs at each period of follow-up.
Graph 4 Comparison between studied periods regarding Clinical Attachment Level for both premolars at both designs at each period of follow-up.
Results of radiographic evaluation
Graph 5 Comparison between the studied periods according to results of radiographic evaluation at design B.
Understanding the difference in nature and behavior of the tissues supporting RPD is critical for long term success of the prosthesis. These differences multiplied by the function, create major stresses on the tooth-tissue prostheses 10. So, it is necessary for an attachment used in conjunction with RPD to be with proper design of reciprocation to reduce the lateral load to which the RPD is subjected.5 In this study we suggest the use of extracoronal resilient attachment retained RPD in mandibular distal extension ridges, to reduce the forces transmitted to the underlying tissues, which is agreed with some authors15–17 but with certain limitations to avoid excessive torque applied to the most distal abutment. Moreover, extracoronal attachments are castable attachments with plastic retentive portion. With its elasticity, it is possible to control the flexure and construct a resilient and shock absorbing prostheses.18 Williamson M19 advocates the use of extracoronal attachments to adjust the abutment alignment and to select the proper path of insertion. Furthermore, Baker & Goodkind15 stated that attachment retainer decreases the caries susceptibility as it eliminates food stagnation around clasps, and provide splinting effect of the abutment teeth. In this study, there was a slight increase in all clinical parameters at both sides, but it was higher at abutment teeth with parallel interlock design (Design B). By excluding patient factor, as both designs were included in the same RPD for the same patient, it was explained that presence of lingual bracing arm with Design B increased the opportunity for plaque accumulation which is one of the main causes of gingival inflammation. On the other hand, reduction of the clinical parameters was revealed at integrated interlock design (Design A) in relation to Design B which can be attributed to the preservation of the lingual normal artificial crown contours without need of modification for the reciprocal arm, so patient comfort was enhanced, also stagnation of food and plaque was reduced when compared with a lingual reciprocal arm. Both attachment designs were associated with little amount of bone loss which was clinically acceptable as the extracoronal resilient attachments induced more favorable stress patterns and the least force transmitted to the abutment teeth.20 Bone loss at the second premolar abutment tooth was more than that at the first premolar abutment tooth at both designs as attachment retained RPD tend to concentrate more stress at the terminal abutment tooth.21 But, parallel interlock design (Design B) showed statistically significant increase of bone resorption around both abutment teeth where there was lingual bracing arm, this is agreed with Saito et al.20 who showed in his study that attachment denture to which a lingual stabilizing arm had been added produced more stress on the abutment teeth than did the attachment denture without a stabilizing arm. It seems reasonable to assume that with lingual stabilizing arm, there was more rigidity than was without it inducing more stresses. From mechanical point of view the bracing arm occupy most of the occluso-gingival height of the abutment tooth in a closer location to the center of rotation of the tooth so, the resultant forces from the RPD are passing through the long axis of the tooth, this is ideal in case with conventional clasp.20 While the attachment retainer is less stressful to the abutment tooth than is the conventional clasp. The basis for this reasoning is that the retentive clasp arm is positioned on the facial or lingual surface of the tooth while an attachment retainer is located at the axial proximal surface therefore all stresses are directed along the long axis of the tooth and resisted by virtually all the fibers of periodontal ligament. Stress directed in this manner is concentrated nearer to the center of rotation of the tooth than is the case with a conventional clasp, which is more ideal from a standpoint of leverage.22 Moreover, the extracoronal attachment reduces the lever arm in relation to the root length as it places the support for removable partial denture closer to bony support of abutment teeth,23 and this explains the reduction of bone loss with attachment retained RPD. For the integrated interlock attachment design of reciprocation, it includes a shear distributer within the confines of the attachment itself that directs leverage along the long axis of the tooth eliminating the need for RPD component of reciprocation. Thus the integrated interlock can counteract the lateral force which has the greatest effect on the terminal abutment in distal extension base PRDs with universal hinge attachments.24 Fixed splinting of abutment teeth for attachment retained RPD provides increased resistance only to antero-posterior forces, and the removable partial denture being anchored on both sides of the arch and joined together with rigid major connector, can provide cross arch stabilization to forces operating in a buccolingual direction.25 This support the results of this study that the lingual bracing arm is not mandatory for reciprocation in attachment retained RPD, on the contrary, it affects the health of abutment teeth negatively. Furthermore, integrated interlock design (Design A) for reciprocation can afford the required reciprocal effect with healthy behavior of the abutments. From previous discussion we can advocate the use of integrated interlock design (Design A) for reciprocation as it allows a degree of indirect retainer and simplicity of selection of path of insertion. Furthermore, the location of integrated interlock closer to the long axis of the abutments may decrease the torque, enhance clinical oral parameters and cause less bone resorption than the parallel interlock design (Design B).
With the limitations of the present study, we can conclude the followings;
None.
None.
The authors declare that there is no conflict of interest.

©2017 Abdelhamid, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.