Journal of
eISSN: 2373-4345


Case Report Volume 4 Issue 5
1Department of Oral Medicine & Radiology, JSS University, India
2Post Graduate Student, Department of Oral Medicine & Radiology, JSS University, India
Correspondence: Karthikeya Patil, Professor and Head of Department of Oral Medicine & Radiology, JSS Dental College & Hospital, JSS University, Mysore, India
Received: December 09, 2015 | Published: May 11, 2016
Citation: Patil K, Mahima VG, Keshari D. Solitary central neurofibroma of the mandible. J Dent Health Oral Disord Ther. 2016;4(5):122-124. DOI: 10.15406/jdhodt.2016.04.00122
Solitary, intraosseous neural tumours of the jaws are a rare occurrence. Central neurofibromas are benign tumours of non-odontogenic origin. Neurofibromatosis may present with soft tissue lesions in the head and neck region. However, occasional cases of such tumours arising within the jaw bones have been reported. We report a case of central neurofibroma in a young female patient with a brief review of literature.
Keywords: central, mandible, neurofibroma, solitary, swelling, parasymphysis
Neurofibroma or neurinoma is a moderately firm, benign, well-circumscribed tumour caused by proliferation of Schwann cells in a disorderly pattern that includes portions of nerve fibers, such as peripheral nerves, axons, and connective tissue of the sheath of Schwann. As neurofibromas grow, they incorporate axons. In contrast, neurilemomas are composed entirely of Schwann’s cells and grow by displacing axons.1
Majority of the neurofibromas of the head and neck region are found affecting the soft tissues.2 Intraosseous or central neurofibroma is a rarity as only very few cases have been described in the literature. Bruce in 1954 first described solitary neurofibroma of the oral cavity. Since then less than 50 cases have been documented in the literature.3 This can be explained by the fact that bone marrow spaces don’t have nerve sheaths or myeli¬nated nerves.2
We present a case of central neurofibroma affecting the left side of mandible in a 25 year old female patient.
A 25 year old female patient reported to us with a chief complaint of swelling on the left side of face since 5 weeks which was not preceded by any trauma or toothache. There was no history of associated pain or mobility of any teeth in the region of complaint. Patient gave history of self fall 4 weeks back following which she developed pain in the region of swelling. She was otherwise in good health and her medical history was unremarkable. Family history of the patient was non-contributory. General physical examination did not reveal any cutaneous nodules, cafe au lait pigmentation or axial freckling.
Extra-oral examination showed a solitary, diffuse, smooth swelling in the left mandibular parasymphysis region measuring about 3 X 2 cms in size. The swelling was mildly tender on palpation and firm to hard in consistency. Intra-orally, buccal vestibular tenderness and expansion with decortication was noted in relation to 34, 35 and 36. Lingual cortical plate expansion was also noted (Figure 1). There was no evidence of any tooth related abnormalities such as caries, fracture and wasting diseases. The concerned teeth also did not show any signs of mobility or periodontal pockets. There was no evidence of any discharge or ulceration in the affected area. The surrounding area and other oral mucosal sites appeared to be normal.
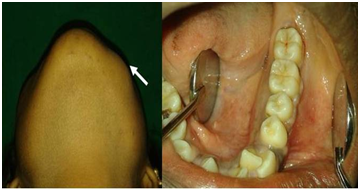
Figure 1 Basal view of the patient showing swelling in the left parasymphysis region and intra-oral view showing buccal vestibular obliteration and expansion of cortical plates.
Orthopantamograph showed a well defined, homogeneous, unilocular radiolucent lesion in relation to 33, 34, 35, 36 and 37 measuring about 4 cm X 3 cm in greatest dimension. The internal structure was suggestive of a cyst within a cyst appearance without any internal calcifications. Divergence of the roots of 35 and 36 was noted with mild amount of root resorption of the distal surface of the 35 and mesial surface of distal root of 36. The continuity of the inferior alveolar canal was lost and mental foramen could not be traced. The lower border of the mandible appeared intact (Figure 2).

Figure 2 Orthopantamograph showing well-defined, homogeneous, unilocular lesion in the left mandibular parasymphysis region.
Mandibular lateral occlusal view was taken which revealed bicortical plate expansion (Figure 3a). Fine needle aspiration was attempted which yielded negative results. Following clinical and radiographic examination, a differential diagnosis of unicystic ameloblastoma, keratocystic odontogenic tumour, traumatic bone cyst, neurofibroma and neurilemmoma was considered.
Enucleation of the lesion was done under local anaesthesia and the specimen was sent for histopathological analysis. Miscoscopic examination showed tumour composed of spindle cells with elongated wavy nuclei, fine chromatin and fibrillary cytoplasm. Stroma showed prominent myxoid change. Based on the clinical, imaging and histopathologic findings, a final diagnosis of central neurofibroma was made (Figure 3b). The post-operative period was uneventful. The patient was followed up after 3 months and showed satisfactory healing.
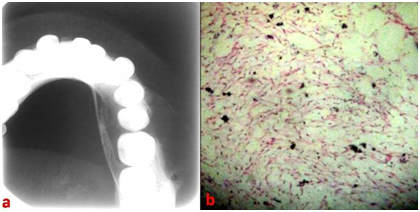
Figure 3 Mandibular lateral occlusal view showing bicortical expansion and photomicrograph showing spindle cells with elongated wavy nuclei, fine chromatin and fibrillary cytoplasm.
Neurofibroma is usually considered to be an essential characteristic of a generalized syndrome known as neurofibromatosis (NF), a neurocutaneous systemic disease that arises from an autosomal dominant mutation. NF includes a heterogeneous spectrum of disorders. NF-1 is the most common form and is characterized by a range of neurocutaneous and soft-tissue lesions. NF type 2 is characterized by the development of bilateral acoustic neuromas.4
Ninety percent of the neurofibromas are associated with neurofibromatosis type 1. However, occurrence of a solitary case is a rarity. Literature review also revealed scarce number of reported cases (approximately 50) of solitary intraosseous neurofibromas. The finding of a solitary case necessitates physical examination and fami¬ly history in order to exclude the disease.2 The present case presented with a negative family history of neurofibromatosis. Also general physical examination did not reveal any abnormalities. Majority of the cases reported are found in the posterior mandible and few in the maxilla.5 The predisposition of its occurrence mostly in mandible is due to thick nerve bundles of inferior alveolar nerve.6 Our patient also presented with a solitary lesion in the left mandible.
Hubner and Lewis investigated the factors responsible for the development of the lesion through an animal model and stated that the peripheral nerve section resulted in the formation of an expanded connective tissue cap at the end of the proximal segment. In an attempt to re-establish continuity with the distal segment, the nerve fibres penetrated into and beyond the cap, becoming entangled and entrapped within the soft tissue.7
Neurofibroma occurs at various ages between 14 and 45 years old, and the average age range is 27.5 years old.8 A male: female ratio of 1:2 has been observed.5 Our patient was a 25 year old female. In the mandible, patients report with pain and paraesthesia.7 Our patient reported with swelling in the left mandible and pain initiated only after the traumatic event.
Neurofibroma is accompanied with fusiform enlargement of the foramen and the inferior canal, a branched mandibular canal, a deep sigmoid notch, a decreased mandibular angle, a deformed condyle, non eruption of the teeth and a cyst like lesion. Hypo- or hyperplasia of the mandible, maxilla, zygoma and the temporomandibular joints has also been reported.9 Enlargement of the mental foramen has also been reported.10
The importance of the use of modern imaging modalities such as CT and MRI, and their superiority over plain film radiography for early detection and precise delineation can also be seen. On CT scans without contrast, NF lesions appear almost isodense with neural tissue, and bone erosion in the vicinity may be the only visible manifestation of the tumour. Contrast enhancement is generally homogeneous and clearly demonstrates the margins of the lesion,10 logically; solitary neurofibromas are similar to the lesions seen in neurofibromatosis.2 These tumors are not encapsulated and comprise a mixture of Schwann cells, perineural cells, and endoneural fibroblasts. Neurofibromas show haphazard arrangement of nerve fibers on a background of irregularly distributed collagen matrix, with a few areas showing spindle cells and mucinous stroma. Mast cells are frequently present with hyaline changes in older lesions.6
Since neurofibromas are not usually encapsulated, a wide margin is essential if they are excised.10 The lack of encapsulation may lead to recurrences as complete surgical removal may be difficult. Thus, it would be appropriate to perform a more radical resection.
Radiotherapy as an alternative to surgery may retard growth and shrink the size of the tumor, but it may not be sufficient alone. Small and accessible lesions of neurofibroma show excellent results when treated with diode lasers.6
Neurofibrosarcomas can develop in about 5-16% of all patients with multiple neurofibromas associated with neurofibromatosis.2 Increased incidence of pheochromocytoma is also seen. Malignant potential of solitary neurofibroma is not known, but is considered to be negligible. Once malignancy develops in any of the lesions of neurofibromatosis, the prognosis becomes poor.6
Although the recurrence rate is low, there have been reports of a malignant transformation of these tumors, with the possibility that the presumed lesion may have been the first manifestation of von Recklinghausen’s disease. Thus a close follow up is warranted.11
Neurofibromatosis is a relatively common disorder, but intraosseous neurofibroma is a rarity. As a solitary lesion, it might present with diagnostic difficulties. Hence it is essential for the oral diagnosticians to be aware of even the rare presentations of relatively common disorders which might also be the first indicator of the disease process.
The author declares that there was no conflict of interest.

©2016 Patil, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.