Journal of
eISSN: 2373-4345


Case Report Volume 2 Issue 4
1Department of Oral and Maxillofacial Surgery, Army College of Dental Sciences, India
2Department of Pathology, Mount Sinai St. Luke?s-Roosevelt Hospital, USA
Correspondence: Abdul Basit Karim, DDS, Mount Sinai St Luke?s-Roosevelt Hospital, 1111 Amsterdam Ave. Minturn 205 New York, NY 1002, USA, Tel 212-523-3171
Received: May 15, 2015 | Published: June 18, 2015
Citation: Karim AB, Sumarriva L, Sharabi A, et al. Basal cell adenoma of the upper lip: a case report. J Dent Health Oral Disord Ther. 2015;2(4):140-142. DOI: 10.15406/jdhodt.2015.02.00058
Purpose: We report the case of an 84 year old male who had been complaining of a slow growing painless mass on the upper lip. Adequate preoperative imaging and differential diagnosis is paramount before proceeding with surgical intervention.
Materials and Methods: Hematoxylin-Eosin staining
Results: Histopathological examination of the specimen was significant for basal cell adenoma.
Conclusion: Suspicion of malignancy in an upper lip mass is low. Most often, an upper lip mass would be canalicular adenoma. Basal cell adenoma is most common in the parotid gland and rarely presents in the upper lip.
Keywords:Salivary gland, pleomorphic adenoma, Parotid gland, neoplasms, pleomorphic
Salivary gland tumors are uncommon neoplasms, comprising of 2 to 6 percent of all head and neck tumors.1,2 The majority occur in major salivary glands, specifically the parotid gland. Pleomorphic adenomas are the most common benign tumors of salivary glands and occur mainly in the parotid gland. Basal cell adenoma is a benign salivary gland tumor that also primarily occurs in the parotid gland.2,3 Histo pathological examination of the tumor cells of basal cell adenoma shows a basaloid appearance without any presence of myxo chondroid stroma, which is characteristic of pleomorphic adenoma.1,3 Basal cell adenomas are rare and account for 1-3% of all salivary gland tumors.1,3 More than 75% of basal cell adenomas occur in the parotid gland, and are rarely seen in the minor salivary glands.2,3 The goal of this paper is to report an uncommon presentation of this rare tumor of the salivary glands. There has only been one other report of basal cell adenoma of the upper lip in the review of literature.
An 84 year old Hispanic male presented to the Mount Sinai St. Luke’s Hospital Oral and Maxillofacial Surgery Clinic complaining of a painless swelling on the upper lip of two years duration. The patient presented to the clinic due to concern for gradual increase in size of mass. Clinical examination showed a movable, firm, painless, sub mucosal mass located on the upper lip 2 centimeters left of midline (Figure 1). The mass was covered with non-ulcerated pinkish mucosa and measured 2 centimeter in the widest diameter (Figure 2). Magnetic resonance imaging of the upper lip was obtained for further evaluation, and was significant for a well circumscribed, radiopaque, round mass, measuring 2 centimeters at the widest diameter (Figure 3–5). The patient underwent complete excision of the lip mass including 0.5cm margins under general anesthesia in the operating room (Figure 6). Microscopic examination on low power magnification showed a well circumscribed adenoma arising in a dilated salivary gland duct, presenting two patterns, the trabecular component, which is the dominant pattern, and the solid component (Figure 7,8). On high power magnification the trabecular component showed basal cell proliferation growing in elongated, ribbon-like pattern and the solid component with small uniform basal cells (Figure 9,10).

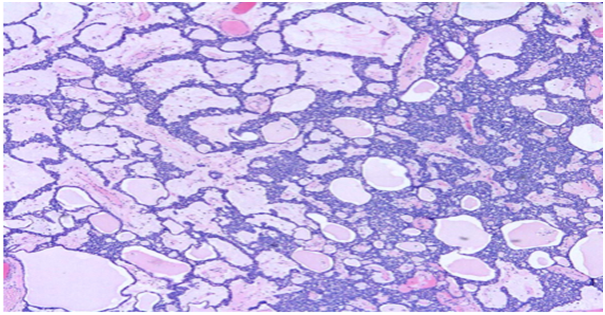
Monomorphic adenomas are a group of benign salivary gland tumors that have a more uniform histopathology pattern than the common pleomorphic adenoma.4 Basal cell adenoma is a histologic variant of monomorphic adenoma of salivary glands.3 However, per WHO recommendation “monomorphic adenoma” is non-specific and basal cell adenoma is preferred.4 Structural and immuno histo-chemical studies have shown that in addition to basaloid cells, basal cell adenomas could also have a combination of salivary ductal epithelium and myoepithelial cells.2 Basal cell adenomas show some histopathologic similarity to the canalicular adenoma; however, histopathologic and clinical differences warrant that they be considered as distinct entities.1,2 The origin of the basal cell adenoma is epithelial, likely in the cells of the terminal duct.1,4 Basal cell adenomas are usually well-circumscribed, and are subdivided into four histologic subtypes including solid, trabecular, tubular, and membranous types.1–3 The solid subtype has large islands with hyper chromatic and palisading peripheral cells, and central cells that are squamous and form keratin pearls.1,3 The solid subtype is most common and the epithelial cells are supported by a small amount of fibrous stroma.2,3 In the trabecular subtype the basal cells are in an elongated, ribbon-like pattern.1,3 The tubular subtype has multiple small duct like structures lined by columnar-appearing cells with uniform, hyper chromatic, and round to oval nuclei1. Both tubular and trabecular subtypes have a prominent vascular stroma.1,3 Frequently, a mixture of tubular-trabecular subtypes is also seen with cellular stroma composed of myoepithelial cells.3 In contrast to other subtypes, the membranous pattern has a jigsaw arrangement of epithelial islands, and is multi lobulated and frequently unencapsulated.2 The islands are surrounded and separated by eosinophilic, periodic acid-Schiff positive, hyalinized material representing reduplicated basal lamina.3 Malignant transformation is highest in association with the membranous subtype.1,3 In our case, the specimen was composed of the more common solid subtype and trabecular pattern. Basal cell adenomas have a varying gender predilection, and occur over a wide age range from the fourth to the ninth decades of life.4 In our case, the patient was male in the eighth decade of life. The clinical presentation most commonly seen is a slow-growing, asymptomatic, movable, well-circumscribed mass, usually measuring less than 3 centimeters in diameter.1–3
Over 75% of basal cell adenomas occur in the parotid gland, and rarely present in minor salivary glands.1–3 When they do occur in oral mucosal sites, they preferentially occur in the upper lip and rarely occur in the palatal mucosa.5 In contrast, when pleomorphic adenomas occur in oral mucosal sites they have a predilection for palatal mucosa rather than the upper lip.1,3 The differential diagnosis for basal cell adenoma should include canalicular adenoma, pleomorphic adenoma, sebaceous adenoma, and adenoid cystic carcinoma. If mass of this nature presents in the parotid or hard palate then fine needle aspiration cytology should be performed to rule out malignancy, including adenoid cystic carcinoma and basal cell adenocarcinoma.6 In our case, the pathology was present in the upper lip, and suspicion for malignancy was low. The treatment used in this case was the same proposed in the literature, complete surgical excision with an extra capsular limit of 0.5cm2. The post-op course was unremarkable, with complete healing of the surgical site, and after a follow-up of two months, there are no signs of local recurrence.
None.
The author declares that there are no conflicts of interest.
None.

©2015 Karim, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.