Journal of
eISSN: 2373-4345


Research Article Volume 1 Issue 5
1Orthodontist, Private Practice, USA
2Private Practice, Greece
3Department of Restorative Dentistry and Biomaterials Sciences, Harvard School of Dental Medicine, USA
Correspondence: Tom C Pagonis, Department of Restorative Dentistry and Biomaterials Sciences, Harvard School of Dental Medicine, 188 Longwood Avenue, Boston, MA 02115, USA, Tel 1617-432-5846, Fax 1617-432-0901
Received: August 24, 2014 | Published: September 30, 2014
Citation: Viazis AD, Viazis E, Pagonis TC. The Concept of a new dental disease: orthodontosis and orthodontitis. J Dent Health Oral Disord Ther. 2014;1(5):141-145. DOI: 10.15406/jdhodt.2014.01.00030
Introduction: Angle’s 110 year old classification of malocclusion lacks verifiable scientific validity, and lacks substantiation on whether ideal occlusion significantly improves oral function or provides significant benefits in oral or general health. We propose a new orthodontic classification based on evaluating the position of roots and location of bone in the horizontal dimension.
Materials and Methods: Thousands of completed orthodontic cases, with an overwhelming majority treated non-extraction were subjected to photographic and radiographic evaluation. Based upon this we propose new orthodontic classifications of
Discussion: To date, a link between malocclusions and periodontal condition remains unclear and controversial. With this new classification patients will be diagnosed and treated accordingly based on their own individual genetic and morphologic appearance rather than an arbitrary ideal.
Conclusion: A new orthodontic classification namely Orthodontosis and Orthodontitis is proposed for malpositioned teeth based on the clinical morphology, appearance and contour of the alveolar bone and ridge. This new classification, as a replacement of or as a supplement to traditional classifications may lead to more non- extraction orthodontic therapeutic modalities.
Keywords: orthodontitis, orthodontosis, dentistry, orthodontics, periodontics, braces
PAR, peer assessment rating, IOTN, index of orthodontic treatment need, OHP, oral health promotion, TBI, tooth bone interface, OTM, orthodontic tooth movement, PDL, pressure within periodontal ligament
A critical prerequisite for orthodontic treatment is the understanding of and classification of malocclusion. Currently there are several classifications of malocclusion which include classic qualitative methods such as Angle1 and more contemporary quantitative methods and indices such as Peer assessment rating (PAR) and Index of orthodontic treatment need (IOTN). First developed in 1899, Angle’s classification2 has remarkably endured the test of time and continues to be utilized as the main language of malocclusion among orthodontic specialists. Yet, there continues to be an emerging body of literature that exposes the lack of evidence for this conventional classification of malocclusion in Class 1 (ideal), II or III. Graverly et al.3 showed poor diagnostic inter-provider reliability while Siegel’s survey study4 among 34 chairpersons of Orthodontics Departments in the U.S. showed that fewer than 65% were in agreement on the meaning of a Class II sub-division. An editorial published in the American Journal of Orthodontics in 20095 stated that, although the concept of ideal occlusion has taken precedence as the ultimate goal in clinical orthodontics for some 110 years and serves as an adopted arbitrary method convention and clinical gold standard, it has no verifiable scientific validity, and that no one has yet demonstrated that ideal occlusion provides significant benefits in oral or general health, or that it significantly improves oral function. Rinchuse et al.6 also question the arbitrary nature of this classification that suggests a change in a stable, functional mandibular position in order to achieve a morphologic occlusion that conforms to an arbitrary ideal.
It is estimated that the teeth are in contact for less than 20 minutes per day.7 Why then should a dentist base his/her diagnosis of a patient's malpositioned teeth on the occlusion and not on the alveolar bone that is a constant 24 hours a day? Why shouldn't the same principles that apply to the evaluation of the bone and roots in the vertical dimension utilized in the field of Periodontics also apply to the field of orthodontics in the horizontal dimension? Clinical observations after two decades of orthodontics practice leads us to propose the establishment of a new classification for malpositioned teeth based on the clinical morphology and appearance of the alveolar bone and ridge. This classification is a paradigm shift from the traditional orthodontic thinking and more in line with the current accepted theories found in the periodontal literature and the specialty of Periodontics.
Thousands of completed orthodontic cases, with an overwhelming majority treated non-extraction over a span of two decades of clinical practice utilizing a system of braces that upright the roots from the beginning of treatment8-21 were subjected to photographic and radiographic evaluation. Clinical observation leads us to propose the establishment of a new classification for malpositioned teeth based on the clinical morphology of the alveolar bone and ridge.
Localized Orthodontosis, This term replaces the old Angle term of Class I ideal occlusion. This condition typically has an overbite/overjet relation of 2-3mm which is adequate for anterior guidance. Orthodontosis is the non-inflammatory deficiency of the alveolar bone in the horizontal dimension caused by the displaced root(s) of the tooth, typically palatally or lingually. This result in excess soft tissue and chronic inflammation called Orthodontitis. Once the root is upright then the alveolar bone is restored and the Orthodontitis (the gingivitis from malpositioned teeth) is alleviated (Figure 1–5).
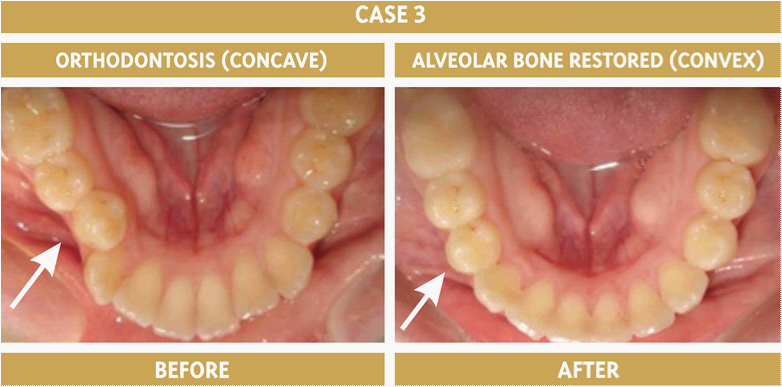
Figure 3 Orthodontosis in the right mandibular premolar area. Orthodontosis is the deficiency of alveolar bone in the horizontal dimension caused by the displaced root(s) of the tooth, typically palatally or lingually.
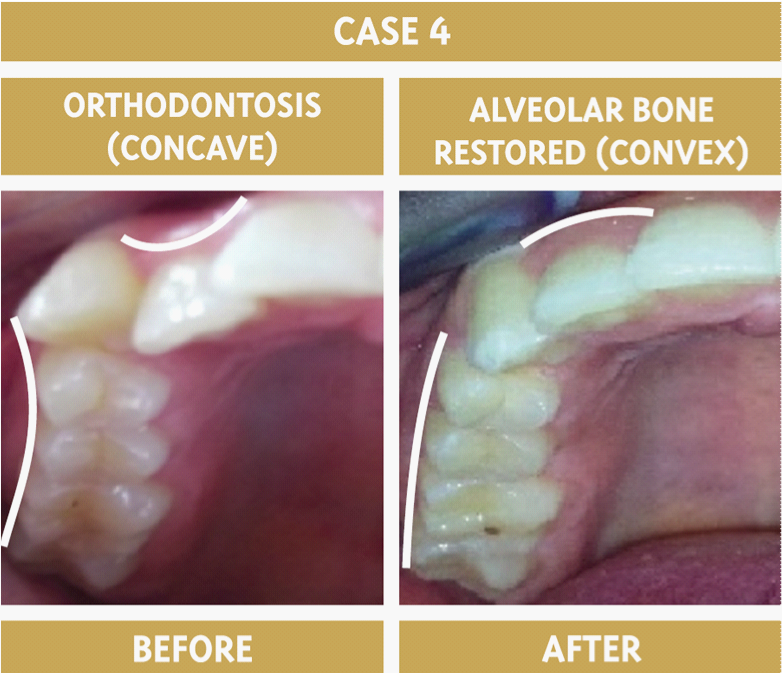
Figure 4 The maxillary right premolars and maxillary right lateral incisor have Orthodontosis. The canine tooth should be bracketed after the lateral and premolar roots have up righted in order for the alveolar bone to be restored beforehand.
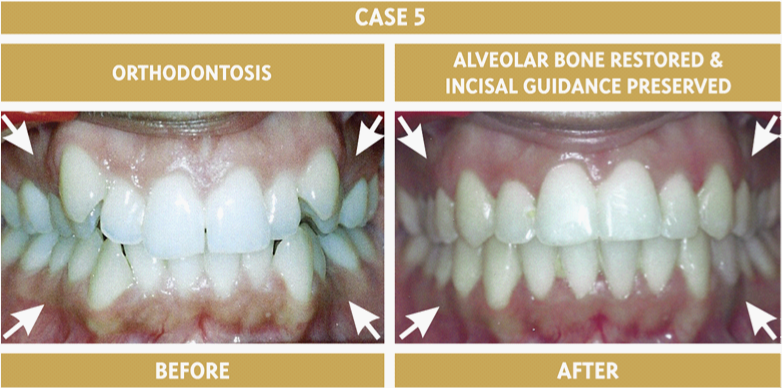
Figure 5 The deficiency of the alveolar bone morphology by the first premolars is restored after their roots orthoerupted in their upright position. Non-extraction therapy restores the mouth to its natural dental arches as if the teeth erupted normally to these positions in the first place.
Premaxillary Orthodontosis, This term replaces the old Angle term of Class II malocclusion. These types of cases typically demonstrate flared upper anterior teeth and a premaxilla that seems underdeveloped as the roots of the upper anterior teeth did not erupt to their full upright potential. As a result, the overbite/overjet relation is excessive. Upper interproximal reduction molar to molar can easily help alleviate this condition and restore the alveolar bone to the level it should have always had. If the patient also demonstrates mandibular retrognathia, then a surgical procedure may also be indicated (Figure 6).
Mandibular Orthodontosis, This term replaces the old Angle term of Class Ill malocclusion. These types of cases typically demonstrate minimal overbite/overjet with retro lined lower incisors or negative overjet (underbite). Apart from a slight maxillary deficiency, these cases show excess alveolar bone and/or basal bone formation with retro lined incisors. Lower interproximal reduction molar to molar can alleviate this condition for up to three lower anterior teeth in underbite relation. If more teeth are in anterior crossbite then a surgical procedure may also be indicated (Figure 7).
Periodontic orthodontic interrelationships, Generally, treatment planning of orthodontic care is based primarily on the premise of improvements of function, dental and facial esthetics and general dental health. Yet, a link between malocclusions and periodontal condition remains unclear and controversial at best. Van Gastel’s 22 findings in a literature review on the impact of malocclusion and orthodontic treatment of periodontal health does not show a clear correlation. Furthermore, a systematic review by Gray and McIntyre23 shows a positive association of orthodontic care and periodontal health by quantifying the impact of orthodontic oral health promotion (OHP) which produced a reduction in plaque with an improvement in gingival health.
Microbial sub gingival plaque composition of malpositioned Vs non-malpositioned teeth, Our proposed classification of malpositioned teeth by the evaluation of alveolar bone and roots in the horizontal dimension is consistent with differences found in the microbial composition of sub gingival plaque of malpositioned Vs non-malpositioned teeth. While several factors contribute to the microbial colonization of dental plaque including pH, temperature and osmotic pressure,24-28 physical barriers to self-cleansing caused by malpositioned teeth facilitate the accumulation of plaque and its microbial constituents.29 Chung et al.30 concluded that compared to non-malpositioned anterior dentition in adults, malpositioned anterior dentition exhibited greater plaque accumulation, a greater number of periodontopathogens present in sub gingival plaque with a significantly more common presence of Fusobacterium species, Capnocytophaga species, C rectus and P micros. In addition, a study by Thornberg et al.31 examined levels of eight periodontal pathogens, Actinobacillus actinomycetemcomitans, Eikenella corrodens, Fusobacterium nucleatum, Porphyromonas gingivalis, Prevotella intermedia, Tannerella forsythia, Treponema denticola, and Campylobacter rectus on adolescents pre operatively, pre operatively and post operatively. They concluded that orthodontic treatment had a positive effect post treatment and protective for four of the pathogens, namely Eikenella corrodens, Fusobacterium nucleatum, Treponema denticola, and Campylobacter rectus.
Current concepts of tooth eruption, The formation of the human tooth represents a complex participation of various cell/tissue types involving interactions between ectoderm and neural-crest-derived mesenchyme.32,33 A process of differentiation ultimately gives way to the development of a functional unit which includes the tooth and surrounding periodontal tissue (i.e. alveolar bone, periodontal ligament).34 The area between the alveolar bone and tooth cementum, which has been referred to as the tooth-bone interface (TBI),35 houses the soft tissue of the periodontal ligament in a developed and functional tooth. During the development of a tooth crown the TBI creates space for the developing tooth to grow while providing a soft tissue space for periodontal ligament formation during root development. While the TBI possesses an osteogenic potential36,37 it is essential that the space remain free from mineralization in order to prevent ankylosis of the developing tooth and root. This appears to involve the coordinated action of osteoclasts. The impaired function of osteoclasts in the adjacent tooth-bone interface would cause alveolar bone growth into the space, impaired development of the growing tooth germ and primary failure of eruption in humans.38 Therefore the regulation of osteoclastogenesis plays a critical role by providing a clear path in bone for tooth eruption and root formation.39
Eruption of a developing tooth crown begins with root development by the movement of the crown away from the point of initial root development.29 Eruption requires the fulfillment of two criteria,
Orthodontic tooth movement (OTM) and accompanying bone remodeling processes are caused by varying changes in the stress/strain distribution in the periodontium caused by intra-alveolar movement of the roots. The mechanical stimulus provided by the moving roots translates into a biological response which is termed mechanotransduction.42 Commonly accepted theories of tissue reaction to orthodontic forces include,
The new concept of “orthoeruption”, up righting the roots of malpositioned teeth from the beginning of orthodontic treatment represents a new theory of orthodontic tooth movement after completion of tooth eruption. Based upon generally accepted concepts of resorption from compression and bone formation by tension forces, this new technology of orthodontic tooth movement contemplates that light forces may possibly stimulate bone remodeling around the area of displaced roots. This would allow for the up-righting of displaced roots into a straight position as if the tooth erupted in that position, thus we propose the term “orthoeruption”. Orthoeruption results in the alveolar bone remodeling and restoration of the dental arch to its appropriate natural size and shape for each specific mouth. Accordingly non-extraction therapy is almost always achieved through this bone “growth” remodeling as the alveolar bone reacts to a tooth erupting in its correct place in the arch and follows accordingly. The accompanying bracket technology attempts to deliver very light forces to simulate the low force eruption stimuli that is possibly needed to allow for bone remodeling around the displaced root area of the alveolar bone and thus achieve correction of root position.
Furthermore, the authors believe that orthodontic diagnosis based on the morphology of the alveolar bone accepts the patient’s natural dentition within its own hard tissue and soft tissue substrate. Therefore patients are simply diagnosed and treated accordingly based on their own individual genetic and morphologic appearance and not based on arbitrary ideals. As a result of the proposed new concept, people’s faces all over the world are accepted de facto and would not be subject to alteration from extractions that would mutilate the natural facial and alveolar morphology. For example, a patient with bimaxillary protrusion would be accepted as normal and natural for that specific individual. If that individual wishes any facial alteration of their alveolar appearance beyond a straight smile then the authors believe that belongs under the realm of periodontal/oral maxillofacial and or plastic surgery.
Thousands of completed orthodontic cases, with an overwhelming majority treated non-extraction utilizing a system of braces that upright the roots from the beginning of treatment were subjected to photographic and radiographic evaluation. Based upon this large body of clinical observation, a new orthodontic classification namely Orthodontosis and Orthodontitis is proposed for malpositioned teeth based on the clinical morphology, appearance and contour of the alveolar bone and ridge. This new classification, as a replacement of or as a supplement to traditional classifications may lead to more non extraction orthodontic therapeutic modalities.
None.
The authors declare that there is no conflict of interest.

©2014 Viazis, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.